Abstract
Background
Geographic cohorting is a hospital admission structure in which every patient on a given physician team is admitted to a dedicated hospital unit. Little is known about the long-term impact of this admission structure on patient outcomes and resident satisfaction.
Objective
To evaluate the effect of geographic cohorting on patient outcomes and resident satisfaction among inpatient internal medicine teaching services within an academic hospital.
Design and Intervention
We conducted an interrupted time series analysis examining patient outcomes before and after the transition to geographic cohorting of our 3 inpatient teaching services within a 520-bed academic hospital in November 2017. The study observation period spanned from January 2017 to October 2018, allowing for a 2-month run-in period (November–December 2017).
Participants
We included patients discharged from the inpatient teaching teams during the study period. We excluded patients admitted to the ICU and observation admissions.
Main Measures
Primary outcome was 6-month mortality adjusted for patient age, sex, race, insurance status, and Charlson Comorbidity Index (CCI) analyzed using a linear mixed effects model. Secondary outcomes included hospital length of stay (LOS), 7-day and 30-day readmission rate, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, and resident evaluations of the rotation.
Key Results
During the observation period, 1720 patients (mean age 64, 53% female, 56% white, 62% Medicare-insured, mean CCI 1.57) were eligible for inclusion in the final adjusted model. We did not detect a significant change in 6-month mortality, LOS, and 7-day or 30-day readmission rates. HCAHPS scores remained unchanged (77 to 80% top box, P = 0.19), while resident evaluations of the rotation significantly improved (mean overall score 3.7 to 4.0, P = 0.03).
Conclusions
Geographic cohorting was associated with increased resident satisfaction while achieving comparable patient outcomes to those of traditional hospital admitting models.
Similar content being viewed by others
INTRODUCTION
Hospital admissions are an increasingly complex and high-risk time in the care of patients.[1,2,3] Residents on inpatient services are charged with rising to these demands of inpatient care despite frequent transitions between hospital sites and changes in schedules and workflow.[4] Organizational strategies that help to simplify the delivery of high-value, patient-centered, and interdisciplinary care within the hospital are critical.[5]
Geographic cohorting is one organizational strategy of growing interest. Geographic cohorting is a model of structuring admissions such that patients on a given physician service are admitted to a dedicated hospital unit.[6] Geographic cohorting may help expedite the delivery of care by clustering the patients that each physician team cares for within the hospital, thereby facilitating bedside care for each patient and minimizing travel time between patients. In addition, by assigning physicians to a consistent unit and interprofessional team of nurses, case managers, social workers, and therapists, geographic cohorting has been associated with improvements in provider satisfaction, perceived efficiency, interprofessional collaboration, and physician-patient communication.[6,7,8]
Importantly, less is known about the effect of geographic cohorting upon patient outcomes, patient satisfaction, or resident physician training. Studies comparing geographic cohorting to traditional models have shown similar lengths of stay and 30-day return rates.[7, 8] Findings on patient satisfaction in these studies differ: one showed improvement[8] and another showed no impact.7 Additionally, while one study found lower in-hospital mortality for patients admitted to geographically cohorted units when compared to patients cared for by the same physician teams but admitted to different hospital units, none reports on post-hospital mortality before and after transitioning to geographic cohorting.[9]
Similarly, little is known about the impact of geographic cohorting upon resident satisfaction.[6] One study surveyed both attending and resident physicians and found that geographic cohorting collectively led to a perceived increase in the quality of care, amount of time communicating with patients and nurses, and sense of teamwork among the interprofessional team.[7] Geographic cohorting may be particularly beneficial to resident physicians, compared to attending hospitalists, as residents rotate between different clinical sites with variable clinical duties and workflows, and as residents are not expected to be as efficient or clinically experienced as attending hospitalists.
To build upon this literature, we assessed the impact of the transition from a traditional, non-geographic model of admissions to geographic cohorting on patient outcomes, patient satisfaction, and resident evaluations of the rotation upon our inpatient medicine teaching services.
METHODS
Context and Intervention
In November 2017, the internal medicine teaching services transitioned to geographic cohorting within our 520-bed academic tertiary hospital. The hospital is home to three inpatient medicine teaching services, each comprising an attending physician, a second- or third-year senior resident, two first-year residents, and one to three medical students. Residents and students rotate approximately every 4 weeks and attending physicians rotate every 2 weeks. Prior to the intervention, the teaching services cared for up to 20 patients at a time distributed across the hospital, ranging from 3 to 7 different units, and admitted daily based on an every-other-daylong- and short-call structure. While pre-intervention teams would cap at 20 patients, the consistent norm for average team census was 12–13 patients.
With the transition to geographic cohorting, each team was assigned 13 to 16 beds on a dedicated unit with a continuous admitting structure (i.e., daily admitting and discharging from assigned geographically cohorted unit as appropriate). This was designed and coordinated with the support of key stakeholders from physician (hospital and residency), nursing, case management, and bed management leadership. Our study was approved by the University of Pittsburgh Medical Center’s Quality Review Committee.
Study Design and Population
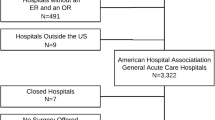
We conducted a retrospective interrupted time series (ITS) analysis[10] to compare outcomes of patients discharged from January to October 2017 (before the intervention) to the outcomes of patients discharged from January to October 2018 (following the intervention), allowing for a 2-month run-in period.
All patients discharged from the inpatient teaching services at UPMC Shadyside Hospital from January 2017 to October 2018 were eligible for inclusion. We excluded patients admitted first to the intensive care unit (ICU), rather than directly to our teaching services, in order to minimize confounding of patient outcomes including satisfaction and mortality related to their ICU care. Observation admissions were also excluded due to their lower medical complexity and exclusion from HCAHPS survey data. We also excluded patients with sickle cell disease because of an administrative decision to triage this population to a different hospital in May 2018.
Outcome Measures
Our primary outcome was 6-month mortality adjusted for age, gender, race, ethnicity, insurance type (private, Medicare/Medicaid, uninsured), and Charlson Comorbidity Index (CCI).[11] Our secondary outcomes included hospital length of stay, 7-day and 30-day readmission rates, patient satisfaction, and change in resident evaluation scores of the rotation. Patient level data was collected from an institutional database, which collates both local electronic health records and national social security registry data. Readmission rates were measured using inpatient readmissions to any of the 40 affiliated regional hospitals within the next 7 or 30 days. Patient satisfaction was measured by percent of top box scores rating physicians as “excellent” among questionnaire items pertaining to physician communication on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, a 32-item tool required by the United States Centers for Medicare and Medicaid Services, administered after discharge to a random number of inpatients.[12] Resident rotation evaluations were collected via a 10-item electronic survey, including one overall item that asks the resident to rate the “overall impression of the quality of the rotation” on a 5-point Likert scale, ranging from poor to excellent (Supplementary Appendix A). The year prior to the intervention, 2017, was compared to the second year after the intervention, 2019, to compare resident views on the rotation itself and not the implementation of the transition.
Statistical Analysis
We conducted ITS analyses to assess the impact of this intervention on patient outcomes using monthly time intervals and the individual patient as the unit of analysis. ITS analysis is a quasi-experimental design that uses regression modeling to estimate the effects of a given intervention when randomization is not possible or practical.[10]. When one patient contributed multiple observations (i.e., admitted multiple times), we used the characteristics from the patient’s first encounter in the EHR during the study period. We stratified patients by whether their first encounter happened before or after the intervention and conducted t tests and chi-square tests to determine if significant differences existed between patients who were first admitted pre- versus post-intervention.
We then constructed a mixed effects logistic regression model fit via maximum likelihood estimation to assess the impact of this intervention on our primary patient outcome, 6-month mortality rate. We included fixed effects for continuous time, a binary pre-post intervention indicator, and the interaction between time and intervention. Additionally, we adjusted for fixed effects including patient race, sex, health insurance type, health plan, and CCI.[11] To account for repeated measures from the same patient over time, a random patient effect as well as a random time effect with an autoregressive covariance pattern was included. Similar ITS models were employed to evaluate the secondary outcomes of 7-day and 30-day returns. For the length of stay, a mixed effects linear regression model with the same fixed and random effects was used, given the continuous nature of the outcome.
To evaluate changes in patient satisfaction, we modeled the proportion of top box scores rating physicians as “excellent” using a mixed effects logistic regression model including year (2017 vs. 2019) as a binary fixed effect and physician as a random effect to account for the clustering of multiple patient satisfaction ratings within the same physician. The percentage of “excellent” ratings pre- and post-intervention, as well as their difference, was then obtained. Overall scores on resident evaluations were modeled using a linear mixed model that included a binary fixed effect for year (2017 vs. 2019) and a random effect for resident to account for clustering of multiple evaluations per resident. Mean overall scores pre- and post-intervention, as well as the estimated difference in pre-post mean scores, were obtained via least squares estimation.
Lastly, we ascertained the reason for missing CCI data and assessed its impact in our longitudinal modeling. Outpatient records and diagnoses were used to calculate each patient’s CCI, and therefore, a patient without a prior outpatient encounter within our healthcare system may not have a CCI for their first encounter. As CCI was a fixed effect in all ITS models, encounters without a CCI could not be included in model estimation. To assess the impact of this, we compared baseline characteristics between patients with complete CCI data versus those without, using t tests for continuous variables and chi-square tests for categorical variables. Characteristics for which significant differences were identified were adjusted for in the ITS models. Under the assumption that our data are missing at random (MAR), likelihood-based estimation such as that employed for our ITS models provides valid inferences in the face of missing data.
All point estimates are reported along with corresponding 95% confidence intervals and p values. A significance level of α=0.05 was assumed, and no adjustments were made for multiplicity. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
A total of 1720 patients were discharged from the inpatient teaching services during the observation period. Patient census on each team and number of patients seen remained unchanged, with 904 discharges prior to the intervention and 911 discharges after the intervention (of which 95 patients were in both groups). Patient demographic and baseline clinical characteristics, including mean age, sex, race, health insurance type, and CCI, are summarized in Table 1. Of those, 28 patients had a missing CCI and were unable to be included in the final model. We did not find any significant differences between the observed characteristics of the excluded patients with missing CCI and those with a CCI (eTable 1 in the Supplement).
There was no difference in 6-month mortality among patients discharged prior to the intervention and those discharged afterwards (3.1% immediately prior to intervention vs. 3.9% after; OR 1.13; 95% CI 0.99, 1.30; P = 0.083). Furthermore, we found no difference in length of stay (2.84 days immediately prior to intervention vs. 3.22 days after; slope change 0.046; 95% CI −0.07, 0.16; P = 0.43), 7-day return rate (4.1% immediately prior to intervention vs. 3.67% after; OR 1.02; 95% CI 0.88, 1.18; P = 0.79), or 30-day return rate (18.6% immediately prior to intervention vs. 12.99% after; OR 0.95; 95% CI 0.87, 1.04; P = 0.28) to a UPMC facility.
Patient response rates on our HCAHPS scores ranged from 36 to 38% (339/904 discharged patients in 2017 and 333/911 discharged patients in 2018), which is higher than reported national survey response rates of 27% in 2017.[13] HCAHPS scores improved but not significantly (Table 2). Resident satisfaction with the overall rotation significantly increased (+0.2870; 95% CI 0.0376, 0.5364; P = 0.03) (Table 2).
DISCUSSION
Overall, in this ITS analysis, we found no significant change in 6-month mortality, length of stay, 7- or 30-day return rate, or HCAHPS scores after transitioning to geographic cohorting among inpatient teaching teams at a large academic medical center. Resident satisfaction with the rotation significantly improved.
Our study is one of the largest retrospective analyses of geographic cohorting to date and the first to evaluate the effect of this transition upon post-discharge mortality. It is also the first to use a pre- and post-study design to assess mortality. Prior studies in this literature differ from ours in several key ways. For example, in the only other analysis of the effect of geographic cohorting on mortality, Bai et al. evaluated in-hospital mortality, rather than post-discharge mortality, across 3243 consecutive admissions and found that the 1125 patients admitted to “off-service” wards had significantly higher in-hospital mortality compared with 2118 propensity score–matched patients admitted to geographically cohorted units (hazard ratio 3.20 upon admission, 95% CI 1.92 to 5.33; P < 0.0001) within a large Canadian tertiary care hospital.9 Similar to our findings, length of stay did not differ between the two groups. Mortality after 6 months, return rates, and HCAHPS scores were not evaluated.
There are a number of reasons why our findings may not have shown the positive impact on mortality shown by Bai et al., including differences in study design and primary outcomes.
Bai et al. compared patients that were admitted to geographically cohorted units to patients admitted to other hospital units contemporaneously, rather than using a pre/post study design. These analyses are fundamentally different. Improved in-hospital mortality among patients in a geographic unit compared to those contemporaneously on another unit may be more influenced by factors, such as hospital and physician census and resource availability, that may be less likely to have a post-discharge impact. In addition, evaluating in-hospital mortality cannot reflect ways in which post-discharge access to care, quality of care, etc. could mitigate a possible detrimental short-term impact of non-geographic cohorting. Additionally, in-hospital mortality necessarily does not inform how the totality of the hospital stay, including discharge planning and communication on geographically cohorted units, may impact patient outcomes, since by definition the hospital stay ends in the patient’s death. Post-hospital mortality is a better measure to this end. Overall, our combined findings offer strong evidence that mortality is not adversely impacted, immediately or post-discharge, by geographic cohorting.
One of the most notable findings of our study is that resident rotation evaluations significantly improved after the transition to geographic cohorting. While the effect size is small (3.7 to 4.0), our experience demonstrates a meaningful improvement, as significant quantitative changes in resident rotation evaluations occur quite infrequently. Notably, this remained true despite the fact that resident workload and patient volume remained unchanged (904 patients discharged prior vs 911 patients discharged after). With rotating schedules and clinical responsibilities, geographic cohorting may lessen the demands of the inpatient rotation by providing a consistent clinical location and interprofessional team. This consistency may help to minimize extraneous cognitive load and help residents focus on their patients’ care, rather than time spent navigating variable realities of different hospital units including differences in case management, nursing ratios, unit culture, and many other impactful aspects of different clinical sites. Indeed, in their pre-post evaluation of transitioning to geographic cohorting, Bryson et al. found that participating residents, hospitalists, and nurses reported improved communication and quality of care.[7] This suggests that improved communication, in addition to more efficient workflows, is likely some of the important reasons for which the residents viewed this transition positively. With an ongoing imperative to combat resident burnout[14,15,16] and a growing need to train dedicated future hospitalist physicians[17, 18], resident satisfaction is an important outcome to target, especially when it can be optimized without impacting patient outcomes.
Prior studies which have evaluated length of stay, return rates, and patient/provider satisfaction before and after geographic cohorting have found similar findings to ours. Using a before and after cross-sectional survey involving 159 patients (93 before, 64 after), Olson et al. evaluated the effects of implementing geographic cohorting among their general internal medicine teaching services on patient-physician communication, physician and nursing perceptions, length of stay, and 30-day return rate at a 367-bed, community teaching hospital in Connecticut.[8] Olson et al. found no difference in length of stay (6.8 days pre vs. 6.8 days post) or 30-day return rates (32.1% pre vs. 34.1% post; P > 0.05). Our results corroborate these findings within a larger, tertiary care academic setting.
Drawbacks to geographic cohorting have been described.[6, 19] Two of the most universal barriers include increased interruptions due to increased physician availability to the rest of the interprofessional team and significant logistical challenges to implementation. While each hospital will have its own unique barriers, a major lesson learned was the critical importance of engaging key stakeholders throughout the design, implementation, and evaluation of this transition. Our team included leadership from the department of medicine, the internal medicine residency program, the department of emergency medicine, nursing, case management, admissions, bed management, and hospital administration. We learned early the importance of regular meetings both prior to and after implementation to discuss challenges that emerged and reach consensus on process solutions. This allowed us to anticipate, prevent, and adapt to unforeseen problems as they presented. A similar approach of stakeholder engagement and open communication is essential to the success of this transition within any hospital that is considering implementation of geographic cohorting.
Our study has several limitations. Our retrospective ITS study design does not allow us to fully account for any confounding hospital initiatives that may have been implemented contemporarily with our study. As mentioned, we excluded patients admitted to the ICU or under observation. While we have no reason to suspect otherwise, it is a limitation of our study that we do not have data to confirm that the number of patients excluded for these reasons was similar pre- and post-intervention. Additionally, we only assessed residents’ evaluations of the rotation and did not gather evaluative data from other members of the interprofessional team such as our nurses, case managers, administrators-on-duty, or hospital leadership. These evaluations would provide a more complete picture of the impact of geographic cohorting on hospital workflow and employee satisfaction, in addition to the patient outcomes which we assessed.
Future research should focus on the impact of geographic cohorting on resident competencies, particularly those of patient care, professionalism, communication, and system-based practice. An assessment of geographic cohorting’s impact on time of patient discharge would also be of significant interest to hospital leadership given growing financial pressures on hospital systems.[20] Finally, evaluating additional outcomes of key importance to other stakeholders, such as emergency medicine providers, nursing, rehab therapists, case management, bed management, and hospital administration, will be important to creating a holistic understanding of the potential benefits and drawbacks of geographic cohorting.
CONCLUSION
Geographic cohorting was associated with increased resident satisfaction, while achieving comparable patient outcomes and patient satisfaction scores to those of traditional hospital admitting models. These findings suggest that many teaching hospitals would benefit from adopting a geographic cohorting admission model.
References
Ricciardi R, Roberts PL, Read TE, Baxter NN, Marcello PW, Schoetz DJ. Mortality Rate After Nonelective Hospital Admission. Arch Surg. 2011;146(5):545-551. doi:https://doi.org/10.1001/archsurg.2011.106
Quinn KL, Stall NM, Yao Z, et al. The Risk of Death Within 5 Years of First Hospital Admission in Older Adults. CMAJ. 2019;191(50):E1369-E1377. doi:https://doi.org/10.1503/cmaj.190770
Centers for Medicare & Medicaid Services (CMS). Complications and Deaths - National. https://data.medicare.gov/Hospital-Compare/Complications-and-Deaths-National/qqw3-t4ie. Accessed May 4, 2020.
Wiese J, ed. Teaching in the Hospital. Philadelphia: American College of Physicians Press; 2010.
Institute of Medicine (US) Committee on Quality of Health Care in America, Kohn LT, Corrigan JM, Donaldson MS, Eds. To Err Is Human: Building a Safer Health System. Washington (DC); 2000.
Kara A, Johnson CS, Hui SL, Kashiwagi D. Hospital-Based Clinicians’ Perceptions of Geographic Cohorting: Identifying Opportunities for Improvement. Am J Med Qual. 2018;33(3):303-312. doi:https://doi.org/10.1177/1062860617745123
Bryson C, Boynton G, Stepczynski A, et al. Geographical assignment of hospitalists in an urban teaching hospital: feasibility and impact on efficiency and provider satisfaction. Hosp Pract (1995). 2017;45(4):135-142. doi:https://doi.org/10.1080/21548331.2017.1353884
Olson DP, Fields BG, Windish DM. Geographic Localization of Housestaff Inpatients Improves Patient-Provider Communication, Satisfaction, and Culture of Safety. J Healthc Qual. 2015;37(6):363-373. doi:https://doi.org/10.1111/jhq.12054
Bai AD, Srivastava S, Tomlinson GA, Smith CA, Bell CM, Gill SS. Mortality of Hospitalised Internal Medicine Patients Bedspaced to Non-internal Medicine Inpatient Units: Retrospective Cohort Study. BMJ Qual Saf. 2018;27(1):11-20. doi:https://doi.org/10.1136/bmjqs-2017-006925
Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression Based Quasi-Experimental Approach when Randomisation Is Not an Option: Interrupted Time Series Analysis. BMJ. 2015;350:1-4. doi:https://doi.org/10.1136/bmj.h2750
Charlson M, Pompei P, Ales K, McKenzie C. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373-383.
Tefera L, Lehrman W, Conway P. Measurement of the patient experience clarifying facts, myths, and approaches. JAMA. 2016;315(20):2167-2168.
Godden E, Paseka A, Gnida J, Inguanzo J. The Impact of Response Rate on Hospital Consumer Assessment of Healthcare Providers and System (HCAHPS) Dimension Scores. Patient Exp J. 2019;6(1):105-114. doi:https://doi.org/10.35680/2372-0247.1357
Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358-367. http://www.ncbi.nlm.nih.gov/pubmed/11874308. .
National Academies of Sciences, Engineering, and Medicine. Taking Action Against Clinician Burnout: a Systems Approach to Professional Well-Being. Washington, DC: The National Academies Press; 2019. doi:https://doi.org/10.17226/25521
Raimo J, LaVine S, Spielmann K, et al. The Correlation of Stress in Residency With Future Stress and Burnout: a 10-Year Prospective Cohort Study. J Grad Med Educ. 2018;10(5):524-531. doi:https://doi.org/10.4300/JGME-D-18-00273.1
Auerbach AD, Chlouber R, Singler J, Lurie JD, Bostrom A, Wachter RM. Trends in Market Demand for Internal Medicine 1999 to 2004: an Analysis of Physician Job Advertisements. J Gen Intern Med. 2006;21(10):1079-1085. doi:https://doi.org/10.1111/j.1525-1497.2006.00558.x
Epane JP, Weech-Maldonado R, Hearld LR, Sen B, O’Connor SJ, McRoy L. Hospitalists, Two Decades Later: Which US Hospitals Utilize Them? Heal Serv Manag Res. 2020. doi:https://doi.org/10.1177/0951484820962295
Singh S, Fletcher KE. A Qualitative Evaluation of Geographical Localization of Hospitalists: How Unintended Consequences May Impact Quality. J Gen Intern Med. 2014;29(7):1009-1016. doi:https://doi.org/10.1007/s11606-014-2780-6
Wertheimer B, Jacobs REA, Bailey M, et al. Discharge Before Noon: an Achievable Hospital Goal. J Hosp Med. 2014;9(4):210-214. doi:https://doi.org/10.1002/jhm.2154
Acknowledgements
Contributors
The authors would like to thank the nurses, case managers, administrators, and hospital leadership for their support, collaboration, and teamwork essential to facilitating the transition to geographic cohorting. The authors also thank Swati Bhosale, MHA, HCSE for her data mining and initial analytics, Robert Feldman, MS for his statistical support, and Ethan Lennox, MA, for his thoughtful feedback on our manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations: These findings wer presented as a virtual poster at the 2020 Society of General Internal Medicine Annual Meeting, May 6, 2020.
Supplementary Information
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Klein, A.J., Veet, C., Lu, A. et al. The Effect of Geographic Cohorting of Inpatient Teaching Services on Patient Outcomes and Resident Experience. J GEN INTERN MED 37, 3325–3330 (2022). https://doi.org/10.1007/s11606-021-07387-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07387-z