Abstract
Background
An inappropriately low frequency of healthcare utilization has been reported to be associated with poor control of chronic diseases, accelerating healthcare disparities. However, the evidence is limited regarding the association between no healthcare utilization and mortality.
Objectives
To examine whether individuals without healthcare utilization have the increased risks of mortality among the US general population.
Design
Prospective cohort study
Participants
Adults aged ≥ 20 years (n = 39,067) in the National Health and Nutrition Examination Survey (NHANES)1999–2014 linked to national mortality data through December 2015.
Main Measures
The exposure was the number of visits to healthcare providers during the past year (healthcare utilization): none, 1–3 times (referent), 4–9 times, or ≥ 10 times. Cox hazard regression models were employed to estimate the adjusted hazard ratios (aHR) of all-cause, cardiovascular, and cancer mortality adjusting for socio-demographic characteristics and comorbidities.
Key Results
During a median follow-up of 7.4 years, participants without visit over the past year showed higher risks of all-cause mortality (aHR [95% CI] = 1.16 [1.04–1.30]) and cardiovascular mortality (aHR [95% CI] = 1.62 [1.28–2.05]) than those who visited the office 1–3 times. We found no evidence of the association between no visit and cancer mortality. The association between no providers’ office visit and all-cause mortality was stronger among males (aHR [95% CI] = 1.22 [1.06–1.40]) than females (aHR [95% CI] = 0.97 [0.79–1.19]; p-for-interaction = 0.01) and among uninsured individuals (aHR [95% CI] = 1.22 [0.98–1.51]) than insured individuals (aHR [95% CI] = 1.09 [0.95–1.25]; p-for-interaction = 0.04).
Conclusion
No providers’ office visit over a year was associated with increased risks of all-cause and cardiovascular mortality. Further investigations are warranted to identify the underlying reasons for the elevated mortality risks due to no healthcare utilization.
Similar content being viewed by others
Association of No Healthcare Utilization with Mortality Among Adults in the USA
INTRODUCTION
Limited healthcare utilization is considered as one of the key upstream determinants of health disparity—a major public health issue in the USA,1,2,3 and is strongly related to social determinants of health (e.g., sex, race/ethnicity, socio-economic status, geography).3,4,5,6,7,8,9,10 In general, individuals with severe medical conditions are likely to visit clinics or be admitted to hospitals frequently,11,12 while relatively healthy individuals use healthcare services less frequently. In this context, the association between the number of healthcare utilization and adverse health outcomes is expected to be positive (or close to the null if all information on disease severity is controlled for). Meanwhile, it is also true that some people, even with health problems, do not have access to or cannot afford healthcare services due to limited financial support, literacy or awareness of diseases, and geographical reasons.2,6,7,13,14 Previous cross-sectional studies have shown that an inappropriately low frequency of healthcare utilization was associated with poor control of chronic conditions including diabetes mellitus,15 hypertension,15,16,17 and dyslipidemia.18 Possible mechanisms of this association may include the lack of optimal interaction between patients and healthcare providers or the lack of opportunities to take optimal management or medication among the individuals with the lower frequency of healthcare utilization.15,18 However, it is still unclear whether individuals with few or no healthcare utilization are associated with long-term health outcomes such as mortality.
In addition, the possible impact of limited healthcare utilization on health outcomes may differ by individuals’ socio-demographic characteristics. For example, individuals with insurance are more likely to utilize healthcare services and have better health outcomes than those without insurance.19,20 A previous evidence showed that the improvement of insurance coverage, through Medicare expansion, has increased appropriate healthcare utilization and reduced overall mortality.5 Furthermore, a previous study has shown that the relationship between socio-demographic characteristics and frequency of healthcare utilization differs between males and females.21 In this context, it is imperative to identify the subpopulation which has a high mortality risk due to an inappropriately low frequency of healthcare utilization so that decision-makers could build an effective strategy targeting such population to improve their health and potentially achieve health equity.
In this study, we hypothesized that people with no healthcare utilization would have higher mortality risks than those with moderate (considered adequate) frequency of healthcare utilization, and the association would vary by their socio-demographic characteristics. To address this hypothesis, we examined the association of the frequency of providers’ office visits (as a proxy of healthcare utilization), particularly no visit (vs. 1–3 times of visits), with all-cause mortality and cause-specific(cardiovascular and cancer, the leading causes of death in the USA22) mortality of the US general population. To identify the subpopulation at high risk of mortality related to no visit of healthcare providers, we also examined whether the association differs by individuals’ socio-demographic characteristics.
METHODS
Data Source and Study Cohort
We used the National Health and Nutrition Examination Survey (NHANES)1999–2014 linked with national mortality data through December 2015. The NHANES had been conducted to assess the health and nutritional status of the non-institutionalized US civilian population using a stratified, multistage probability sampling design. This survey included structured interview data, physical examination data, and laboratory test data, which were released every 2 years.23 The unweighted response rates for the household interview and physical examinations during 1999–2014 were 71–84% and 69–80%, respectively.24 Among 43,793 adults aged ≥ 20 years enrolled in the NHANES 1999–2014, we excluded participants without the data of the number of visits to healthcare providers (n = 34), self-reported health condition (n = 30), smoking status (n = 56), marital status (n = 581), educational status (n = 102), income levels (n = 3,889), insurance status (n = 293), history of cardiovascular diseases (CVD) (n = 218), and history of cancer (n = 53). The final analytical sample included 39,067 participants (89%). The NHANES study protocols were approved by the National Center for Health Statistics Research Ethics Review Board, and the informed consent of all participants was obtained at enrollment.25 This study was conducted following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.26
Exposure Ascertainment: the Frequency of Healthcare Utilization
This household interview collects information on the frequency of provider visits (healthcare utilization) during the past year of the NHANES interview. Participants are asked the following question: “During the past 12 months, how many times have you seen a doctor or other healthcare professional about your health at a doctor’s office, a clinic, hospital emergency room, at home or some other place?” Based on the answer to this question (“none,” “once,” “twice or 3 times,” “4 to 9 times,” “10 to 12 times,” or “13 times or more”), we divided the participants into four groups as follows: no visit (n = 6244), 1–3 times of visits (reference group; n = 17,168), 4–9 times of visits (n = 9751), and 10 or more times of visits (n = 5904). We set 1–3 times of visits instead of once as the reference group to ensure a sufficient statistical power in our main and subgroup analyses for death outcomes as a previous study did.15
Outcome Ascertainment: All-Cause and Cardiovascular Mortality
Our primary outcome was all-cause mortality, and secondary outcomes were cardiovascular and cancer mortality based on the National Death Index (NDI) ascertained from the NCHS using probabilistic matching based on social security number, name, date of birth, race/ethnicity, sex, state of birth, and state of residence.27 Cardiovascular mortality was defined as death from heart diseases and stroke by using the International Classification of Diseases, 10th revision (ICD-10) including acute rheumatic fever and chronic rheumatic heart diseases (I00–I09), hypertensive heart disease (I11), hypertensive heart and renal disease (I13), ischemic heart diseases (I20–I25), other heart diseases (I26–I51), and cerebrovascular diseases (I60–I69). Cancer mortality was defined as malignant neoplasm (C00–C97) in the ICD-10. Time to events was defined as days between the interview date and the end of follow-up (i.e., December 2015) or the date of death.
Other Covariates
Socio-demographic characteristics including age (years), sex (male, female), race/ethnicity (white, black, Hispanic, others), self-reported health condition (excellent, very good, good, fair, poor), smoking status (ever, never), drinking status (never, former, current light/moderate [≤ 2 drinks per day for men or ≤ 1 drink per day for women], current heavy [> 2 drinks per day for men or > 1 drink per day for women]), marital status (married, unmarried), educational status (less than high school, high school, college, graduate), income levels (family poverty-income ratio), and insurance status (uninsured, private, public) were self-reported. Income levels were assessed using the family poverty-income ratio that was calculated from the ratio of the family income to the federal poverty level.23,28 We defined the history of diabetes mellitus, hypertension, and dyslipidemia based on self-report of clinical diagnosis and medications. We also defined the history of CVD (heart attack, angina, heart failure, and stroke) and cancer based on self-report.
The physical examination data and biomarkers of metabolic disorders were measured according to the NHANES laboratory procedure guideline,23 including body mass index (BMI), systolic blood pressure, diastolic blood pressure, estimated granular filtration rate (eGFR), glycated hemoglobin (HbA1c), total cholesterol (T-Chol), high-density lipoprotein cholesterol (HDL-Chol), and triglyceride. BMI was calculated as weight in kilograms divided by height in meters squared. eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation (eGFR = 141 × min[Scr/k, 1]a × max[Scr/k, 1]−1.209 × 0.993age × 1.018[if female] × 1.159[if black]; k = 0.9 for male and 0.7 for female, a = − 0.411 for male and − 0.329 for female, and minimum indicates the minimum of Scr/k or 1 and max indicates the maximum of Scr/k or 1).29Low-density lipoprotein cholesterol (LDL-Chol) was calculated from measured values of T-Chol, triglyceride, and HDL-Chol using the Friedewald calculation ([LDL-Chol] = [T-Chol] − [HDL-Chol] − [triglyceride/5]).
Statistical Analysis
First, we described socio-demographic characteristics according to the frequency of visits to healthcare providers during the past year of the study enrollment. Next, we employed multivariable linear regression models to investigate the cross-sectional association between the frequency of visits to healthcare providers and metabolic markers including BMI, systolic blood pressure, diastolic blood pressure, eGFR, HA1c, T-Chol, HDL-Chol, LDL-Chol, and triglyceride. In these models, we adjusted for age and sex, and then race/ethnicity, self-reported health condition, smoking status, marital status, educational status, family poverty-income ratio, insurance status, and the NHANES survey cycles per 4 years (1999–2002, 2003–2006, 2007–2010, or 2011–2014) (model 1). Using the obtained parameters in the regression models, we calculated the adjusted mean value of the metabolic markers in each exposure category. Third, we employed the multivariable Cox proportional hazard models to estimate the adjusted hazard ratio (aHR) of all-cause and cardiovascular mortality according to the frequency of visits to healthcare providers. In model 2, we included the history of comorbidities (e.g., diabetes mellitus, hypertension, dyslipidemia, CVD, and cancer) in addition to covariates in model 1.
To evaluate the heterogeneity of aHR by individuals’ socio-demographic characteristics, we conducted stratified analyses by age, sex, race/ethnicity, self-reported health condition, smoking status, marital status, education status, income levels, and insurance status. As sensitivity analyses, we re-analyzed the data (i) additionally adjusting for drinking status in our main models (n = 34,123), (ii) restricting participants to those without a history of severe medical conditions such as CVD and cancer (n = 31,925), and (iii) by redefining the groups and setting participants who visited the providers’ office at once (n = 6891) during the past year instead of 1–3 times of visits as the reference group. We applied the NHANES sampling weights to account for the differential probability of selecting the participants and nonresponse of those eligible and approached. All statistical analyses were conducted using R software version 4.0.3.
RESULTS
Socio-demographic characteristics according to the frequency of healthcare utilization are shown in Table 1. The mean ± standard deviation of age was 49.4 ± 18.5 and females were 51.8%. Participants with lower numbers of healthcare utilization were more likely to be young, male, less educated, with low-income levels, and uninsured. They were also less likely to be White, married, and with chronic comorbidities compared with participants with higher numbers of healthcare utilization.
Association Between the Frequency of Healthcare Utilization and Metabolic Markers
After adjusting for socio-demographic characteristics (model 1), we found that participants with no visit during the past year of the study enrollment had higher systolic and diastolic blood pressure, higher total cholesterol, higher HDL-cholesterol, and higher LDL-cholesterol compared with participants who visited the healthcare providers 1–3 times (p value < 0.05 for all outcomes) (Table 2). We also found that the group with higher frequency of healthcare utilization showed a relatively higher adjusted mean of BMI, HbA1c, and triglyceride, and lower adjusted mean of systolic and diastolic blood pressure, eGFR, T-Chol, HDL-Chol, and LDL-Chol.
Association of the Frequency of Healthcare Utilization and Mortality
During the median follow-up of 7.4 (interquartile range, 4.1 to 11.4) years, we observed 5271 (13.5%) all-cause mortality, 1152 (2.9%) cardiovascular mortality, and 1146 (2.9%) cancer mortality. After adjusting for socio-demographic characteristics (model 1), we found higher aHRs for all-cause and cardiovascular mortality among participants with no visit compared with those with 1–3 times of visits (aHR [95% CI] = 1.16 [1.04–1.29] for all-cause mortality and aHR [95% CI] = 1.53 [1.21–1.93] for cardiovascular mortality), but not for cancer mortality (aHR [95% CI] = 1.11 [0.88–1.39]) (Table 3). We also found the increased risk of mortality among participants with 4–9 times of visits (aHR [95% CI] = 1.21 [1.13–1.30] for all-cause mortality, aHR [95% CI] = 1.30 [1.12–1.51] for cardiovascular mortality, and aHR [95% CI] = 1.25 [1.07–1.45] for cancer mortality) and ≥ 10 times of visits (aHR [95% CI] = 1.57 [1.46–1.70] for all-cause mortality, aHR [95% CI] = 1.51 [1.29–1.78] for cardiovascular mortality, and aHR [95% CI] = 1.81 [1.54–2.12] for cancer mortality). The results did not change when additionally adjusting for history of comorbidities (model 2).
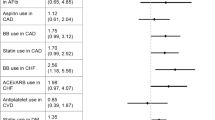
In the subgroup analysis of the association between no visit of healthcare providers (vs. 1–3 times of visits) and mortality (Fig. 1), we found the higher aHR of all-cause mortality among males than females (males, aHR [95% CI] = 1.22 [1.06–1.40]; females, aHR [95% CI] = 0.97 [0.79–1.19]; p-for-interaction = 0.01), and among the uninsured individuals than the insured individuals (uninsured, aHR [95% CI] = 1.22 [0.98–1.51]; insured, aHR [95% CI] = 1.09 [0.95–1.25]; p-for-interaction = 0.04). We found no evidence of heterogeneity of the association between no visits and cardiovascular or cancer mortality by any socio-demographic characteristics (Figs. 2 and 3).
In the sensitivity analyses, the results did not substantially change when additionally adjusting for drinking status (Supplemental Table 1), restricting participants to those without a history of CVD and cancer (Supplemental Table 2), or re-analyzing the data by setting participants who visited the office once during the past year as the reference group (Supplemental Table 3).
DISCUSSION
Using the nationally representative sample of US adults, we found that participants with no healthcare utilization during the past year of the study enrollment were associated with higher risks of all-cause and cardiovascular mortality compared with those with 1–3 times of healthcare utilization. The association between no healthcare utilization and all-cause mortality was stronger among males than females and uninsured individuals than insured individuals.
Consistent with previous studies,15,16,17,18,30,31 our study using the most updated NHANES cohort showed that some physical examination data and biomarkers (i.e., systolic and diastolic blood pressure, LDL-Chol) were less favorable among individuals without providers’ office visit during the past year of the study enrollment than those with 1–3 times of visits, and extended these findings to all-cause and cardiovascular mortality. Although our findings do not necessarily indicate the causal relationship mainly due to the presence of unmeasured common causes of healthcare utilization and mortality such as disease severity and healthcare literacy,7,11,12,13,14 the present study identified the important fact that there is a certain number of individuals who had unfavorable medical conditions increasing mortality risks but have inadequate interaction with healthcare providers and thus fewer opportunities to receive treatment and care for their conditions.15,18 The underlying reasons may include the lack of affordability and accessibility to healthcare services due to limited financial supports and geographical barriers,2,7,14 low healthcare literacy,13 and unawareness of diseases.7,14,18 In addition, the annual checkup and screening program for some diseases (e.g., cancer, diabetes, hypertension, dyslipidemia, etc.) may contribute to better health outcomes among individuals with 1–3 visits than those with no healthcare utilization. Given many other factors that could prevent people from using healthcare services such as geographic area, language barrier, immigration status, and religion,6,7,14 our findings suggest the need for further studies to identify the effective interventions to ensure the optimal healthcare utilization for people who need the care that would eventually reduce health disparities by social risks.32
Our subgroup analyses showed that the association between no healthcare utilization (vs. 1–3 times) and all-cause mortality was stronger among males than females. Although the underlying reasons are unclear, the sex difference in preference of using healthcare services (i.e., females are more likely to visit the clinic than males) might have contributed to the heterogeneous association by sex.10 Another possible reason may include the favorable role of sex steroid hormones, particularly estrogen, on cardiovascular systems. In general, cardiovascular mortality risk among males accelerates at a relatively young age while that among females tends to increase in postmenopausal years due to the lack of estrogen.33,34 Because individuals with no healthcare utilization in our study were younger than other groups, our null findings for mortality among females might be partially explained by such protective effect of estrogen among younger individuals with no healthcare utilization.
We found a stronger association between no healthcare utilization (vs. 1–3 times) and all-cause mortality among uninsured individuals than insured individuals. Given the beneficial impact of insurance coverage on healthcare utilization,5,19,20 most of the insured individuals without healthcare utilization in our study sample might have not needed to use healthcare services while a certain number of uninsured individuals without healthcare utilization might have needed but not been able to use them. Because our follow-up data was collected before the implementation of the Affordable Care Act (ACA)35 and the longitudinal data on insurance status was not available, future studies will be called for to evaluate the association between no healthcare utilization and long-term adverse health outcomes among insured and uninsured individuals after the expansion of insurance coverage through ACA.
Our results suffer from confounding due to disease severity, as indicated by the observed increased mortality risks among participants with ≥ 4 times of healthcare utilization compared with those with 1–3 times of healthcare utilization. However, given the negative relationship between disease severity and no healthcare utilization (i.e., individuals at lower mortality risks are less likely to use healthcare services11,12), such confounding introduces bias toward the null for the association between no healthcare utilization (vs. 1–3 visits) and mortality risks.36 Thus, our findings of the increased mortality risks among people with no healthcare utilization are considered to be robust even in the presence of confounding bias due to disease severity.
There are several other limitations of this study. First, we cannot rule out other potential uncontrolled confounders such as healthcare literacy, which would introduce bias away from the null (i.e., overestimation because people with low healthcare literacy are less likely to use healthcare services and more likely to have high mortality risks due to worse health behaviors or lower perceived health competence7,13,14). Second, as the information on healthcare utilization and participants’ medical conditions were reported at the NHANES enrollment, the temporal ordering of these variables was not clear. Our consistent findings of model 1 (without adjusting for comorbidities) and model 2 (with adjusting for comorbidities) indicate that this limitation would not change our conclusion. Given that some participants without insurance before 2013 might have received insurance coverage after the Medicaid expansion,35 future studies are needed to validate our findings after the implementation of the Affordable Care Act. Third, our study might have a risk of misclassification due to self-report of healthcare utilization and comorbidities. Lastly, although we included around 40,000 US adults, statistical power was not sufficient to assess the heterogeneity of cardiovascular mortality risks related to no healthcare utilization.
CONCLUSION
To the best of our knowledge, this is the first study to investigate the association between the frequency of healthcare utilization and mortality in the US general population. We found an increased risk of all-cause and cardiovascular mortality among individuals without healthcare utilization over the past year of the study enrollment, particularly among males and uninsured individuals. These results generate a hypothesis that a certain number of individuals without healthcare utilization might have needed to use healthcare services to improve their health. Further studies are needed to validate our hypothesis, clarify the underlying reasons for the elevated mortality risks due to inappropriately low healthcare utilization, and identify the high-risk subpopulations for future interventions to reduce health disparity.
References
Bassett MT, Galea S. Reparations as a Public Health Priority — A Strategy for Ending Black–White Health Disparities. N Engl J Med 2020;383(22):2101-2103. doi:https://doi.org/10.1056/NEJMp2026170
Bosworth B. Increasing Disparities in Mortality by Socioeconomic Status. Annu Rev Public Health 2018;39(1):237-251. doi:https://doi.org/10.1146/annurev-publhealth-040617-014615
Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969-2009. J Urban Health 2014;91(2):272-292. doi:https://doi.org/10.1007/s11524-013-9847-2
The Lancet. Cardiology’s problem women. Lancet 2019;393(10175):959. doi:https://doi.org/10.1016/S0140-6736(19)30510-0
Sommers BD, Baicker K, Epstein AM. Mortality and Access to Care among Adults after State Medicaid Expansions. N Engl J Med 2012;367(11):1025-1034. doi:https://doi.org/10.1056/NEJMsa1202099
Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of Primary Care Physician Supply With Population Mortality in the United States, 2005-2015. JAMA Intern Med 2019;179(4):506. doi:https://doi.org/10.1001/jamainternmed.2018.7624
Havranek EP, Mujahid MS, Barr DA, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873-898. doi:https://doi.org/10.1161/CIR.0000000000000228
Manuel JI. Racial/Ethnic and Gender Disparities in Health Care Use and Access. Health Serv Res 2018;53(3):1407-1429. doi:https://doi.org/10.1111/1475-6773.12705
Chen J, Vargas-Bustamante A, Mortensen K, Ortega AN. Racial and Ethnic Disparities in Health Care Access and Utilization Under the Affordable Care Act. Med Care 2016;54(2):140-146. doi:https://doi.org/10.1097/MLR.0000000000000467
Koopmans GT, Lamers LM. Gender and health care utilization: The role of mental distress and help-seeking propensity. Soc Sci Med 2007;64(6):1216-1230. doi:https://doi.org/10.1016/j.socscimed.2006.11.018
Yan S, Seng BJJ, Kwan YH, et al. Identifying heterogeneous health profiles of primary care utilizers and their differential healthcare utilization and mortality – a retrospective cohort study. BMC Fam Pract 2019;20(1):54. doi:https://doi.org/10.1186/s12875-019-0939-2
Owlia M, Dodson JA, King JB, et al. Angina Severity, Mortality, and Healthcare Utilization Among Veterans With Stable Angina. JAHA. 2019;8(15):e012811. https://doi.org/10.1161/JAHA.119.012811
Mayberry LS, Schildcrout JS, Wallston KA, et al. Health Literacy and 1-Year Mortality: Mechanisms of Association in Adults Hospitalized for Cardiovascular Disease. Mayo Clin Proc 2018;93(12):1728-1738. doi:https://doi.org/10.1016/j.mayocp.2018.07.024
Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health 2013;12:18. doi:https://doi.org/10.1186/1475-9276-12-18
Zhang X, Bullard KM, Gregg EW, et al. Access to Health Care and Control of ABCs of Diabetes. Diabetes Care 2012;35(7):1566-1571. doi:https://doi.org/10.2337/dc12-0081
Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States, 1999 to 2012: Progress Toward Healthy People 2020 Goals. Circulation. 2014;130(19):1692-1699. doi:https://doi.org/10.1161/CIRCULATIONAHA.114.010676
Wozniak G, Khan T, Gillespie C, et al. Hypertension Control Cascade: A Framework to Improve Hypertension Awareness, Treatment, and Control. J Clin Hypertens 2016;18(3):232-239. doi:https://doi.org/10.1111/jch.12654
McDonald M, Hertz RP, Unger AN, Lustik MB. Prevalence, Awareness, and Management of Hypertension, Dyslipidemia, and Diabetes Among United States Adults Aged 65 and Older. J Gerontol Ser A Biol Med Sci 2009;64A(2):256-263. doi:https://doi.org/10.1093/gerona/gln016
Baicker K, Finkelstein A. The Effects of Medicaid Coverage — Learning from the Oregon Experiment. N Engl J Med 2011;365(8):683-685. doi:https://doi.org/10.1056/NEJMp1108222
Woolhandler S, Himmelstein DU. The Relationship of Health Insurance and Mortality: Is Lack of Insurance Deadly? Ann Intern Med 2017;167(6):424. doi:https://doi.org/10.7326/M17-1403
Xu KT, Borders TF. Gender, Health, and Physician Visits Among Adults in the United States. Am J Public Health 2003;93(7):1076-1079.
Kochanek KD. Mortality in the United States, 2019. 2020;(395):8.
NHANES-National Health and Nutrition Examination Survey Homepage . Published September 17, 2020. Accessed October 14, 2020. https://www.cdc.gov/nchs/nhanes/index.htm
NHANES Response Rates and Population Totals. Accessed November 10, 2020. https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx
NHANES - NCHS Research Ethics Review Board Approval. Published May 8, 2019. Accessed October 14, 2020. https://www.cdc.gov/nchs/nhanes/irba98.htm
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies | The EQUATOR Network. Accessed October 14, 2020. https://www.equator-network.org/reporting-guidelines/strobe/
Fillenbaum GG, Burchett BM, Blazer DG. Identifying a National Death Index Match. Am J Epidemiol 2009;170(4):515-518. doi:https://doi.org/10.1093/aje/kwp155
Prior HHS Poverty Guidelines and Federal Register References. ASPE. Published November 23, 2015. Accessed November 10, 2020. https://aspe.hhs.gov/prior-hhs-poverty-guidelines-and-federal-register-references
Levey AS, Stevens LA, Schmid CH, et al. A New Equation to Estimate Glomerular Filtration Rate. Ann Intern Med 2009;150(9):604-612.
Paulose-Ram R. Characteristics of U.S. Adults With Hypertension Who Are Unaware of Their Hypertension, 2011–2014. 2017;(278):7.
Kim EJ, Kim T, Conigliaro J, Liebschutz JM, Paasche-Orlow MK, Hanchate AD. Racial and Ethnic Disparities in Diagnosis of Chronic Medical Conditions in the USA. J Gen Intern Med 2018;33(7):1116-1123. doi:https://doi.org/10.1007/s11606-018-4471-1
Vart P, Gansevoort RT, Crews DC, Reijneveld SA, Bultmann U. Mediators of the Association Between Low Socioeconomic Status and Chronic Kidney Disease in the United States. Am J Epidemiol 2015;181(6):385-396. doi:https://doi.org/10.1093/aje/kwu316
Atsma F, Bartelink M-LEL, Grobbee DE, van der Schouw YT. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: a meta-analysis. Menopause. 2006;13(2):265-279. doi:https://doi.org/10.1097/01.gme.0000218683.97338.ea
Mikkola TS, Gissler M, Merikukka M, Tuomikoski P, Ylikorkala O. Sex Differences in Age-Related Cardiovascular Mortality. PLoS One. 2013;8(5):e63347. https://doi.org/10.1371/journal.pone.0063347
The Uninsured and the ACA: A Primer - Key Facts about Health Insurance and the Uninsured amidst Changes to the Affordable Care Act. :28.
Rothman KJ, Greenland S, Lash TL, eds. Modern Epidemiology. Lippincott Williams & Wilkins. 2008.
Funding
KI was supported by Honjo International Foundation Scholarship and National Institutes of Health (NIH)/NIDDK grant F99DK126119. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 170 kb)
Rights and permissions
About this article
Cite this article
Katsuragawa, S., Goto, A., Tsurutani, Y. et al. No Healthcare Utilization and Death. J GEN INTERN MED 37, 1648–1657 (2022). https://doi.org/10.1007/s11606-021-07138-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07138-0