Abstract
Background
Cervical cancer is the third most common malignancy affecting women. Screening with Papanicolaou (Pap) tests effectively identifies precancerous lesions and early-stage cervical cancer. While the nationwide rate of cervical cancer screening (CCS) is 84%, our urban general internal medicine (GIM) clinic population had a CCS rate of 70% in 2016.
Objective
To improve our clinic’s CCS rate to match or exceed the national average within 18 months by identifying barriers and testing solutions.
Design
A quality improvement project led by a multidisciplinary group of healthcare providers.
Participants
Our GIM clinic includes 16 attending physicians, 116 resident physicians, and 20 medical assistants (MAs) with an insured and underserved patient population.
Intervention
Phase 1 lasted 9 months and implemented CCS patient outreach, patient financial incentives, and clinic staff education. Phase 2 lasted 9 months and involved a workflow change in which MAs identified candidates for CCS during patient check-in. Feedback spanned the entire study period.
Main Measures
Our primary outcome was the number of Pap tests completed per month during the 2 study phases. Our secondary outcome was the clinic population’s CCS rate for all eligible clinic patients.
Key Results
After interventions, the average number of monthly Pap tests increased from 35 to 56 in phase 1 and to 75 in phase 2. Of 385 patients contacted in phase 1, 283 scheduled a Pap test and 115 (41%) completed it. Compared to baseline, both interventions improved cervical cancer screening (phase 1 relative risk, 1.86; 95% CI, 1.64–2.10; P < 0.001; phase 2 relative risk, 2.70; 95% CI, 2.40–3.02; P < 0.001). Our clinic’s CCS rate improved from 70% to 75% after the 18-month intervention.
Conclusions
The rate of CCS increased by 5% after a systematic 2-phase organizational intervention that empowered MAs to remind, identify, and prepare candidates during check-in for CCS.
Similar content being viewed by others
INTRODUCTION
Worldwide, cervical cancer is the third most common malignancy affecting women. Screening with a Papanicolaou (Pap) test has decreased the incidence of invasive cervical cancer. In areas where cervical cancer screening (CCS) rates are low, cervical cancer deaths remain high.1 CCS rates are defined as the percentage of eligible women aged 21–64 years who complete CCS using a year-to-date or rolling 12 month average and are based on Healthcare Effectiveness and Data Information Set (HEDIS) measures.2 The US Office of Disease Prevention and Health Promotion’s Healthy People 2020 goal for CCS is 93%3; however, the CCS rate nationwide in 2016 was 84.2%, and was even less for African American women.4,5 In 2016, our urban academic general internal medicine (GIM) clinic had a low CCS rate of 70%, thus prompting an intervention.
A review of the literature shows many effective approaches for increasing cancer screening, including healthcare provider education,6 patient reminders,7,8,9,10,11,12,13,14,15 provider feedback,10,16,17 elimination of structural barriers,7,18 involving non-physician staff,11,19,20,21,22,23 scheduling separate preventive visits,22,24 organizational change,5 and combining multiple strategies at once.25 Shifting top of license responsibilities from physicians to other members of the care team, such as medical assistants (MAs), has been reported to improve quality of patient care.26,27,28,29 Based on these findings, we formed a multidisciplinary group to design an intervention to improve the CCS rate in our clinic to match the nationwide US rate within 18 months.
METHODS
Led by a multidisciplinary team, this quality improvement study used Lean tools to identify barriers to CCS in clinic and target areas for intervention. The study proposal was reviewed by our institutional review board, and was determined to be exempt from full review, as it was a quality improvement project and did not meet criteria for human subjects research by the Revised Common Rule. We followed the SQUIRE guidelines in the reporting of this study.30
Setting
Our urban academic GIM clinic comprises 16 faculty, 116 resident physicians, 20 MAs, and 6 nurses. The MA full-time equivalent (FTE) is 0.73 per 1.0 physician FTE. Annual clinic volume is about 40,000 visits, the majority of which are for chronic disease management, as 22% of our patients have diabetes and 61% have hypertension. The majority (74%) of our patients are African American. All patients seen in our clinic are insured, with approximately 46% commercial, 16% Medicare, 24% Medicare Advantage, and 14% Medicaid.
Prior to our intervention, patients overdue for CCS were contacted 1 to 2 times per year through the electronic portal with letters or by up to 3 telephone calls, after which they were considered lost to follow-up. Approximately half of our patients enrolled in the electronic portal. Education on CCS occurred during the patient clinic encounters and by displays in exam rooms. Provider-level CCS rates were reviewed with physicians twice yearly using a web-based dashboard. We used the electronic medical record (EMR) Epic, which includes alerts to patients and providers when patients are overdue for CCS.
Prior to our intervention, providers identified and offered CCS to patients who were overdue at the end of a visit. If patients were agreeable, the MA would retrieve and set up equipment, and then the provider and MA would reenter the room together to complete the Pap test. Training of residents included a checklist of how to perform a Pap test and practice on a simulation model during onboarding. At minimum, the first 5 Pap tests performed by residents required direct supervision per our institutional policy.
Intervention
Our intervention was designed by a multidisciplinary group of MAs, nurses, and faculty and resident physicians using Lean methods to identify areas for improvement through discussion and by asking our colleagues for input. The barriers identified included patient awareness, cost of visits (including the cost of parking and co-pays), provider knowledge of CCS (as approximately 60% of visits are with resident physicians), and time. CCS extended the length of the clinic visit, which is already time pressured. This was thought to occur because identification of overdue patients by the provider occurred late in the visit and it took time for the patient to gown for CCS and for the MA to retrieve supplies from the supply room.
To address the first 3 identified barriers (patient awareness, cost, and provider knowledge), the first 9-month phase of our intervention implemented patient outreach, financial incentives, and provider education. The second 9-month phase targeted the fourth identified barrier (increased length of visit) and involved a workflow change to allow for early identification of patients overdue for CCS and to shift this task from physicians to MAs.
Phase 1: Outreach, Education, and Financial Incentives
We identified patients who were overdue for CCS using our EMR and selected those who had visits in the last 2 years who were paneled to physicians in our group with low CCS rates. An MA called patients using a standard script to inform them that they were overdue for CCS and offered them a visit for a Pap test including a parking voucher. Patients who indicated that they had a Pap test at an outside facility were asked to have their records faxed. Patients were provided Pap-only visits focusing on CCS and were billed as preventive visits to eliminate co-pays. Small signs were put at the front desk that advertised our women’s health services to improve patient awareness.
All physicians were reeducated on indications for CCS, the role of human papillomavirus (HPV) testing, Pap technique, EMR billing, and documentation procedures using PowerPoint presentations during regular staff meetings. Feedback on the number of Pap tests completed each month was provided to all team members including physicians, MAs, nurses, and secretaries by monthly emails and at staff meetings. Feedback on CCS rate was given quarterly. Data were trended over time and stratified by clinic group. The feedback portion continued throughout the intervention, including phase 2.
Phase 2: Workflow Change
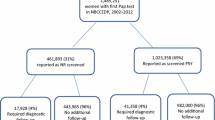
This intervention assigned MAs to identify candidates for CCS from an EMR prompt during a patient’s check-in process (Fig. 1). Patients were asked, using standard scripting, if they were amenable to a Pap test during that visit if time allowed. If the patient agreed, the MA directed the patient to undress from the waist down, the patient was provided a gown and sheet, and a tray was retrieved that was used to set up supplies. When the time came for the Pap test, the MA re-entered the room when the physician was ready and prepared supplies. If the patient declined, the MA informed the physician team by notation in the EMR.
To support this intervention, we ensured that all Pap supplies were available in each exam room, except for trays due to limited supply. This meant that the MA simply had to enter the room when the patient was ready and set up the tray while the patient was being positioned. We opted for this workflow to reduce any waste of supplies in case the Pap test was not completed. The switch to MAs for identifying overdue patients for CCS was implemented through brief presentations at division meetings, email reminders, and discussion during our multidisciplinary huddles.
Outcome Measures
For the 18-month intervention, we measured the number of CCS completed in our clinic each month. We calculated a CCS rate which is defined as the percent of CCS completed in eligible women empaneled to the clinic and is based on HEDIS measures using a 12-month rolling denominator of CCS due in the entire eligible clinic panel population. Eligible women were age 21–64 years and had no history of hysterectomy, had not received a CCS with cytology in the prior 3 years, or for those over 30, a CCS with cytology plus HPV testing in the prior 5 years. As the study period progressed, the number of women overdue for CCS decreased due to routine Pap testing. To account for this reduction in denominator, we calculated a CCS completion index representing the proportion of the CCS completed in our clinic relative to the total remaining CCS due in the panel population at the end of each intervention period. While the number of Pap tests completed and the CCS rate were looked at throughout the intervention, the CCS completion index was calculated after the intervention. All data were extracted from our EMR, which automatically updated when CCS was done in our health system. When CCS was done elsewhere, providers were encouraged to manually update the EMR after obtaining records. We also tracked the number of referrals to obstetrics/gynecology (OB/GYN).
To ensure that our intervention did not increase low-value care, we performed a random chart audit of patients with CCS before and during the intervention. We defined low-value care in accordance with the American College of Physicians31 as CCS performed in patients < 21 years, ≥ 65 years with prior appropriate screening, women with total hysterectomy, HPV screening at age < 30, and more frequent intervals than recommended. However, we used the intervals of 2.5 years for cytology and 4.5 years for HPV testing, as it is considered acceptable by our health system to perform CCS in patients who will be overdue in the next 6 months.
Statistical Analysis
Overall CCS rates were calculated for the following three periods: pre-intervention, phase 1, and phase 2. The relative risks, as the ratio of CCS rates from different periods, and 95% CI were computed to evaluate the effectiveness of the interventions. Interrupted time series analysis adjusted for temporal dependency was also conducted retrospectively to assess the intervention effect, both immediately and over time. The relative risks (RR) and 95% CIs were calculated to evaluate the effects of outreach and workflow interventions compared to baseline. A P < 0.05 was considered statistically significant. Chi-square tests were used to determine the difference. Statistical analysis was done at the end of the study. All data analysis was performed using SAS 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
In the 15 months prior to our intervention, 541 Pap tests were completed in our clinic, averaging 36 per month (Fig. 2), and the CCS rate was 70%. The CCS completion index was 2.86%.
During phase 1 of our intervention, which spanned 9 months, 563 telephone calls were made to 385 patients identified as overdue for CCS. The average age of patients overdue for CCS was 42 years, of which 78% were African American, 13% White, and 9% other. A total of 283 (73%) appointments were scheduled, of which 80 (28%) were cancelled, 87 (31%) were no-show, and 115 (41%) completed their appointments. Overall, 115 patients of the 385 identified (30%) completed their appointments. Of those patients who completed their appointments, 77% were African American, 14% were White, and 9% other. The average number of Pap tests completed in our clinic increased to 56 per month (Fig. 2), totaling 501 Pap tests. The CCS completion index increased to 5.31% (RR, 1.86; 95% CI, 1.64–2.10; P < 0.001) (Fig. 3). Phase 1 was difficult to sustain as it required redirecting MAs to do outreach to patients in an already under-staffed clinic.
During phase 2, which occurred during the subsequent 9 months, the number of Pap tests increased to an average of 71 per month (Fig. 2), totaling 632 Pap tests during this phase. Of the patients who completed CCS, 474 (75%) were African American, 93 (15%) were White, and 65 (10%) were other. The average age was 45 years. The CCS completion index increased further to 7.71% (RR, 2.70; 95% CI, 2.40–3.02; P < 0.001) (Fig. 3). At the end of phase 2, our clinic’s CCS rate improved to 75%.
With both interventions, the number of completed Pap tests increased, while the number of patients overdue for CCS decreased (Fig. 2). The total number of eligible patients for CCS fell from 3643 at the beginning of phase 1 to 3570 at the end of phase 2, while the total number of patients with CCS overdue fell from 1065 to 898 during the same time period. The number of referrals to OB/GYN decreased from 610 in the 9 months pre-intervention to 474 in phase 1 and 518 in phase 2. The number of clinic appointments available remained relatively constant. After outreach and workflow interventions, the number of Pap tests completed increased, with a more significant increase seen with workflow change in phase 2 compared to phase 1 (RR, 1.45; 95% CI, 1.29–1.63; P < 0.001).
Interrupted time series analysis indicated overall significant variation between intervention periods (P = 0.013). After implementation of each intervention, we observed immediate improvement of the CCS rates, with sustained improvement during phase 2 but not in phase 1 (Fig. 4). There was a trend toward increasing CCS rate in the end of the pre-intervention phase. The observed CCS rate of 4.27% at the end of the phase 1 was lower than the predicted rate of 4.92% based on pre-intervention trends. The CCS completion rate at the end of phase 1 was not significantly different from the predicted phase 1 values, had the pre-intervention rate continued (95% CI −1.34 to 2.62; P = 0.52). However, the overall CCS completion rate for the entirety of phase 1 was higher than the pre-intervention rate (5.32% vs 2.90%). In phase 2, we saw an immediate rate increase in the intercept at implementation, a higher increase in positive slope change than the pre-intervention slope increase (0.46 versus 0.12), and a higher than predicted completion rate at the beginning of phase 2 than if the pre-intervention trend had continued (6.04% vs 5.05%).
We performed a random chart audit of 75 patients (25 pre-intervention, 25 in phase 1, and 25 in phase 2). There were no CCS performed in patients younger than 21 years of age, greater than 65 years of age with prior appropriate screening, or in patients with total hysterectomy. There was 1 patient in the control group who had HPV testing at age < 30 and 0 during the intervention. There was 1 patient in the control group and 3 patients during the intervention who had CCS done at sooner intervals than recommended. We found that 4 Pap tests were counted in our total CCS that were ordered but not completed (1 prior to intervention and 3 during the intervention).
DISCUSSION
This quality improvement intervention showed a significant increase in cervical cancer screening within our large, urban GIM clinic during an 18-month period. We used Lean processes to identify the most prominent barriers to CCS within our institution and developed multiple solutions that we implemented in two phases. Both phases involved a team-based organizational change in which MAs identified patients overdue for CCS. During phase 1, we used outreach, education, and financial incentives and observed an increase in the number of Pap tests completed. During phase 2, we used a workflow change which led to a more significant increase in CCS than in phase 1. Our study implemented a unique team-based approach for increasing CCS, suggesting that modest adjustments to clinical workflow may improve CCS rates for certain patient populations.
Phase 1 of our intervention included patient outreach, financial incentives, and provider education. Due to our academic environment, we felt that enhancing provider education was necessary, although it is not possible to know what amount this contributed to the increased rate. Outreach by telephone led to an increase in CCS, but these benefits were offset by the disadvantages of high no-show and cancellation rates and a staffing burden incurred by having MAs make telephone calls. Our clinic has reduced MA staffing compared to other internal medicine clinics, with an average ratio of MA FTE to physician FTE being 0.73, relative to 1.11 nationally.32 Thus, sustainability of phase 1 was challenging. Prior to the initiation of phase 1, we saw an immediate increase in the CCS rate in our clinic, which we believe may have been due to an increased awareness of our low CCS rates. Although the overall CCS rate was higher during phase 1 than in the pre-intervention period, the observed CCS rate for the end of phase 1 was lower than the predicted rate based on pre-intervention trends. We believe this may have been because the intervention was not practically sustainable. This led to the development of our phase 2 intervention.
We found that phase 2 of our intervention, which empowered MAs to identify patients in clinic who were overdue for CCS, was sustainable and led to a significant improvement in CCS. This intervention did not require any additional time or resources aside from the initial education on the workflow change. In other studies involving MA interventions, some of the greatest barriers included time pressure to keep workflow going33 and the need for significant training.27 In contrast, our intervention helped save time by moving the preparation for the Pap test forward in the process. Our intervention did not contribute to a significant increase in low-value care, and the number of referrals to OB/GYN decreased. There were no other system changes.
Although our CCS rate improved from 70% to 75%, we fell short of our target of 83% which may have occurred for several reasons. First, our CCS rate uses a 12-month rolling average, which may have blunted the immediate effect of our intervention. Second, this may have been due in part to a shifting denominator of eligible patients. A total of 1144 Pap tests were done during the 18-month intervention; however, the number of patients overdue for CCS fell by only 167. We postulate several possible reasons for this. First, women enter the study cohort at age 21 and exit the study cohort at age 65, creating a persistent change in the population. Also, women may get a total hysterectomy or change primary care providers. We offered Pap tests to all patients regardless of whether they had a provider within or outside our health system. Some Pap tests are done in women over 65 or sooner than within 3- to 5-year intervals if an abnormal test occurs. Lastly, it was noted in our random chart audit that a small number of CCS ordered were not completed but had been counted in our total CCS count.
Limitations to our study included lack of a control group. As an observational study, our findings are not generalizable to other populations. Since we used CCS ordered as a marker for CCS completion before and during the intervention, our numbers may be slightly higher than the actual number of CCS completed, since a small percentage of patients may not have had CCS completed despite it having been ordered. We were unable to analyze the effect of our increased CCS on patient outcomes due to our small sample size. We did not include patient-stakeholders in the design of our interventions. Our future goal is to expand our organizational intervention to other clinics within our health system to improve our health system CCS rate.
In conclusion, we believe that our systematic organizational intervention empowering MAs to identify and prepare patients for CCS early in the visit could be applied in a variety of clinical settings to help close gaps in care. We found that a combination of outreach, financial incentives, and education were impactful, but were less sustainable over time.
References
National Institutes of Health. NIH Fact Sheets: cervical cancer. Available at: https://archives.nih.gov/asites/report/09-09-2019/report.nih.gov/nihfactsheets/Pdfs/CervicalCancer(NCI).pdf. .
National Committee for Quality Assurance. HEDIS measures and technical resources: cervical cancer screening (CCS). Available at: https://www.ncqa.org/hedis/measures/cervical-cancer-screening/. .
Office of Disease Prevention and Health Promotion. Healthy People 2020: cancer. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/cancer/objectives. .
American Cancer Society. Cancer statistics: Michigan at a glance. Available at: https://www.cancerstatisticscenter.cancer.org/#!/state/Michigan. .
MacLaughlin KL, Jacobson RM, Radecki Breitkopf C, et al. Trends over time in Pap and Pap-HPV cotesting for cervical cancer screening. J Womens Health (Larchmt). 2019;28:244-9.
Mader EM, Fox CH, Epling JW, et al. A practice facilitation and academic detailing intervention can improve cancer screening rates in primary care safety net clinics. J Am Board Fam Med. 2016;29:533-42.
Spadea T, Bellini S, Kunst A, Stirbu I, Costa G. The impact of interventions to improve attendance in female cancer screening among lower socioeconomic groups: a review. Prev Med. 2010;50:159-64.
Hendren S, Winters P, Humiston S, et al. Randomized, controlled trial of a multimodal intervention to improve cancer screening rates in a safety-net primary care practice. J Gen Intern Med. 2014;29:41-9.
Phillips CE, Rothstein JD, Beaver K, Sherman BJ, Freund KM, Battaglia TA. Patient navigation to increase mammography screening among inner city women. J Gen Intern Med. 2011;26:123-9.
Brouwers MC, De Vito C, Bahirathan L, et al. What implementation interventions increase cancer screening rates? A systematic review. Implement Sci. 2011;6:111.
Rees I, Jones D, Chen H, Macleod U. Interventions to improve the uptake of cervical cancer screening among lower socioeconomic groups: a systematic review. Prev Med. 2018;111:323-35.
Peitzmeier SM, Khullar K, Potter J. Effectiveness of four outreach modalities to patients overdue for cervical cancer screening in the primary care setting: a randomized trial. Cancer Causes Control. 2016;27:1081-91.
Everett T, Bryant A, Griffin MF, Martin-Hirsch PP, Forbes CA, Jepson RG. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database Syst Rev. 2011:CD002834.
Tseng DS, Cox E, Plane MB, Hla KM. Efficacy of patient letter reminders on cervical cancer screening: a meta-analysis. J Gen Intern Med. 2001;16:563-8.
Abdul Rashid RM, Mohamed M, Hamid ZA, Dahlui M. Is the phone call the most effective method for recall in cervical cancer screening?--results from a randomised control trial. Asian Pac J Cancer Prev. 2013;14:5901-4.
Sabatino SA, Habarta N, Baron RC, et al. Interventions to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers systematic reviews of provider assessment and feedback and provider incentives. Am J Prev Med. 2008;35:S67-74.
Hwang AS, Harding AS, Chang Y, O’Keefe SM, Horn DM, Clark AL. An audit and feedback intervention to improve internal medicine residents’ performance on ambulatory quality measures: a randomized controlled trial. Popul Health Manag. 2019;22:529-35.
Holden DJ, Jonas DE, Porterfield DS, Reuland D, Harris R. Systematic review: enhancing the use and quality of colorectal cancer screening. Ann Intern Med. 2010;152:668-76.
Han HR, Song Y, Kim M, et al. Breast and cervical cancer screening literacy among Korean American women: a community health worker-led intervention. Am J Public Health. 2017;107:159-65.
Clark CR, Baril N, Kunicki M, et al. Addressing social determinants of health to improve access to early breast cancer detection: results of the Boston REACH 2010 Breast and Cervical Cancer Coalition Women's Health Demonstration Project. J Womens Health (Larchmt). 2009;18:677-90.
Shah SK, Nakagawa M, Lieblong BJ. Examining aspects of successful community-based programs promoting cancer screening uptake to reduce cancer health disparity: a systematic review. Prev Med. 2020;141:106242.
Martinez-Gutierrez J, Jhingan E, Angulo A, Jimenez R, Thompson B, Coronado GD. Cancer screening at a federally qualified health center: a qualitative study on organizational challenges in the era of the patient-centered medical home. J Immigr Minor Health. 2013;15:993-1000.
Wells KJ, Luque JS, Miladinovic B, et al. Do community health worker interventions improve rates of screening mammography in the United States? A systematic review. Cancer Epidemiol Biomarkers Prev. 2011;20:1580-98.
Arroyave AM, Penaranda EK, Lewis CL. Organizational change: a way to increase colon, breast and cervical cancer screening in primary care practices. J Community Health. 2011;36:281-8.
Rodríguez-Gómez M, Ruiz-Pérez I, Martín-Calderón S, Pastor-Moreno G, Artazcoz L, Escribà-Agüir V. Effectiveness of patient-targeted interventions to increase cancer screening participation in rural areas: a systematic review. Int J Nurs Stud. 2020;101:103401.
Baron RC, Melillo S, Rimer BK, et al. Intervention to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers a systematic review of provider reminders. Am J Prev Med. 2010;38:110-7.
Chapman SA, Blash LK. New roles for medical assistants in innovative primary care practices. Health Serv Res. 2017;52:383-406.
Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129-46.
Willard-Grace R, Chen EH, Hessler D, et al. Health coaching by medical assistants to improve control of diabetes, hypertension, and hyperlipidemia in low-income patients: a randomized controlled trial. Ann Fam Med. 2015;13:130-8.
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25:986-92.
Wilt TJ, Harris RP, Qaseem A. Screening for cancer: advice for high-value care from the American College of Physicians. Ann Intern Med. 2015;162:718-25.
Peikes DN, Reid RJ, Day TJ, et al. Staffing patterns of primary care practices in the comprehensive primary care initiative. Ann Fam Med. 2014;12:142-9.
Ferrer RL, Mody-Bailey P, Jaen CR, Gott S, Araujo S. A medical assistant-based program to promote healthy behaviors in primary care. Ann Fam Med. 2009;7:504-12.
Acknowledgements
The authors thank Karla D Passalacqua, PhD, at Henry Ford Hospital for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations: Henry Ford Quality Expo 2/18/20.
Rights and permissions
About this article
Cite this article
Heidemann, D.L., Adhami, A., Nair, A. et al. Using a Frontline Staff Intervention to Improve Cervical Cancer Screening in a Large Academic Internal Medicine Clinic. J GEN INTERN MED 36, 2608–2614 (2021). https://doi.org/10.1007/s11606-021-06865-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-06865-8