Abstract
Background
When working with surrogate decision-makers, physicians often encounter ethical challenges that may cause moral distress which can have negative consequences for physicians.
Objective
To determine frequency of and factors associated with physicians’ moral distress caring for patients requiring a surrogate.
Design
Prospective survey.
Participants
Physicians (n = 154) caring for patients aged 65 years and older and their surrogate decision-makers (n = 362 patient/surrogate dyads). Patients were admitted to medicine or medical intensive care services, lacked decisional capacity and had an identified surrogate.
Main Measures
Moral distress thermometer.
Key Results
Physicians experienced moral distress in the care of 152 of 362 patients (42.0%). In analyses adjusted for physician, patient, and surrogate characteristics, physician/surrogate discordance in preferences for the plan of care was not significantly associated with moral distress. Physicians were more likely to experience moral distress when caring for older patients (1.06, 1.02–1.10), and facing a decision about life-sustaining treatment (3.58, 1.54–8.32). Physicians were less likely to experience moral distress when caring for patients residing in a nursing home (0.40, 0.23–0.69), patients who previously discussed care preferences (0.56, 0.35–0.90), and higher surrogate ratings of emotional support from clinicians (0.94, 0.89–0.99). Physicians’ internal discordance when they prefer a more comfort-focused plan than the patient is receiving was associated with significantly higher moral distress (2.22, 1.33–3.70) after adjusting for patient, surrogate, and physician characteristics.
Conclusions
Physician moral distress occurs more frequently when the physician is male, the patient is older or requires decisions about life-sustaining treatments. These findings may help target interventions to support physicians. Prior discussions about patient wishes is associated with lower distress and may be a target for patient-centered interventions.
Similar content being viewed by others
INTRODUCTION
Some of the most challenging decisions in medical care involve choices between life-prolonging treatment and comfort care. This becomes even more difficult when patients are unable to make their own decisions and require a surrogate decision-maker. Surrogate decision-making for seriously ill, hospitalized patients is a frequent occurrence.1,2,3 Ethical concerns, particularly issues related to physician/surrogate conflict, have been discussed in the ethics literature.4,5,6,7 There is evidence that some surrogates and physicians have high levels of overall distress associated with decision-making.8, 9 However, there are few data about the frequency or severity of moral distress among physicians.
Moral distress is an emotional experience in which an individual feels constrained from acting on deeply held beliefs, resulting in the sense of compromising one’s professional integrity.10 First described in the nursing literature, there is a growing body of evidence that moral distress is a common experience regardless of profession and also has negative consequences for physicians.11 It has been correlated with secondary traumatic stress, burnout, intent to leave a position, and depressive symptoms.12,13,14,15
Physicians may experience moral distress in situations when surrogates are asked to make decisions for patients who cannot express values and preferences, especially when the surrogate must make life and death decisions for the patient 3. In fact, prior studies have found that surrogate decision-making related to end-of-life decisions is one important cause of moral distress, particularly when clinicians feel they are following a plan of care inconsistent with a patient’s best interest because it is what a family wants.11, 16, 17 Physicians may feel tension between the family’s perspective on the patient’s wishes and interest and their own perspective. The current study explored moral distress related to the care of hospitalized elderly patients requiring a surrogate in order to describe the frequency of moral distress and association with particular physician, surrogate or patient characteristics. Due to the importance of conflict in surrogate decision-making, our pre-specified hypotheses were as follows: discordance between the physician and the surrogate regarding the preferred plan of care would be associated with higher physician moral distress, and discordance between physicians’ preference for the plan of care and their perceptions of the actual plan of care would be associated with higher physician moral distress.
METHODS
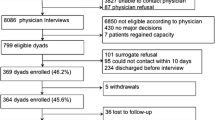
We conducted a secondary analysis of a study that was originally designed to validate a survey of surrogate related communication quality.18 The sample size for the original study was determined for purposes of validating a survey of clinician/surrogate communication. Power for this secondary analysis is provided in the “Results” section. This prospective observational study was conducted in medicine and medical intensive care unit services of three hospitals in one Midwestern city. The hospitals included services where medical residents and fellows cared for patients and services staffed only by attending physicians. The Indiana University institutional review board approved the study.
Participants
Eligible participants for this analysis were physicians, regardless of specialty who cared for patients requiring a surrogate decision-maker within 96 h after patient admission. Eligible patients were 65 years and older, admitted to medicine or medical ICU services, hospitalized for at least 48 h, lacked decisional capacity, and had a qualified surrogate based on state law.18 Surrogate decision-makers for each of these patients provided consent for participation for both themselves and the patient.
Study Procedures
For each patient, a trained research assistant conducted a 3–5-min telephone interview with the available physician caring for the patient (intern, resident, fellow or attending) between 48 and 96 h after patient admission. Physicians were identified using a service call schedule. We typically started with the most junior member of the team because on teaching services, junior physicians spend the most time in direct patient care and likely would know the patient’s situation the best. The patient’s surrogate was then surveyed between hospital day 3 and 10 to obtain patient and surrogate characteristics and the surrogate’s judgment about the best course of treatment, perception of medical care and decision-making. Time frames for physician and surrogate interviews were determined based on feasibility of data collection.
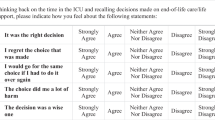
Instruments
Physician demographics included gender, role on the team, years of clinical experience, (intern, resident, fellow, or attending) and knowledge of patient preferences. Also, the physician was asked if he or she was aware that the patient had expressed preferences for medical treatment prior to losing capacity (see Appendix online). Physician moral distress was measured using an oral version of the moral distress thermometer (MDT) regarding the care of a specific patient.19 Physicians were provided a definition of moral distress and asked to rate their moral distress on a 0–10 scale regarding the care of the patient. Additionally, physicians and surrogates were asked to identify their preferred course of treatment and their perception about the course of treatment the patient was receiving. The courses of treatment options were (1) focused on extending life as much as possible, (2) focused on relieving pain and discomfort, and (3) in between, (some treatments might be too burdensome). Physicians identified whether any of a number of predefined major decisions had been considered during the hospitalization, e.g. life-sustaining treatment, procedures, or hospital discharge to a skilled nursing facility. Acceptance of discharge to a skilled nursing facility was included because it can be a strong reflection of values and preferences regarding quality of life and rehabilitative goals of care.
Surrogates were asked to complete a survey that included information about patient and surrogate demographic variables, the Family Inpatient Communication Survey (FICS) 18 to measure surrogate perceptions of clinician emotional support and information provided, and the Generalized Anxiety Disorder-7 (GAD-7) 20 to assess anxiety. Surrogates were also asked about their judgment regarding the best course of treatment for the patient and whether the patient had discussed their preferences for medical care with anyone in the past (Appendix online). Patient medical data obtained by a trained research assistant from the electronic medical record included age, location of admission (ICU versus medical bed), and reason for incapacity. The research assistant also reviewed diagnoses to calculate the Cumulative Illness Rating Scale (CIRS) 21, 22 to assess the patient’s illness severity
Statistical Analysis
We selected physician, surrogate, and patient characteristics variables that we hypothesized would be associated with physician moral distress, based on our review of the literature. Bivariate analyses using logistic regression were performed to determine the degree to which moral distress is associated with each variable. Because 58% of physicians reported a moral distress score of 0, and no other distribution adequately fit the model, including zero-inflated models, this variable was dichotomized into no moral distress versus any moral distress (0 vs. ≥ 1) for all analyses. Because we were interested in patient and surrogate characteristics as well as physician characteristics associated with moral distress, we conducted the analysis at the patient level. Physicians could have more than one patient, and hence more than one moral distress score in the data set. This intra-physician correlation was handled by the use of generalized linear mixed models (GLMMs), with the use of random intercepts for physician.
“Course of Treatment” variables (physician preferred, physician perceived, surrogate preferred) were paired to assess for discordance: physician preferred with surrogate preferred; physician preferred with physician perceived. Additional covariates were examined as predictors of secondary interest based on (1) clinical and demographic relevance and (2) results from previous analyses on the same data for the primary and other secondary analyses, in order to adjust for their potentially confounding effects. The two primary predictors of interest (physician/surrogate discordance and physician preference/perceived discordance) were tested in different models due to their theoretical and conceptual correlation with each other. Due to some physicians having all zero scores and some physicians having all high, 8+, scores and the small number of large moral distress scores, we wanted to ensure our results were robust and therefore performed sensitivity analyses by removing such observations to examine whether results were similar All analyses were performed using SAS v9.4 (SAS Institute, Cary, NC). All analytic assumptions were verified. Collinearity was tested.
RESULTS
Overall, our data did not support our pre-specified hypothesis that physician moral distress would be more likely when there was discord between the physician and surrogate preference for treatment. However, there was increased moral distress when the physician perceived the plan of treatment to be different than what they would prefer. A close examination of other variables revealed some additional interesting findings.
Demographic and Moral Distress Characteristics
There were 154 eligible physicians. These physicians provided moral distress ratings for 362 of enrolled 364 patient/surrogate dyads (ratings were missing for two patients).18 Physicians had an average of 5.8 years of experience since graduating from medical school. Most saw only one patient (64.9%), but some saw more than one, with a maximum of 32 (Table 1). Enrolled patients had a mean age of 81.8, 61.9% were women, 68.8% white, and 27.9% African American (Table 2). The most frequent reason for patient incapacity identified in the medical record was dementia (221 or 61.1%). Surrogates’ mean age was 58.3, 71.0% were women, 68.7% white, and 28.5% African American. The majority of surrogates were the patient’s adult children at 69.3%, with 17.1% being spouses (Table 2).
MDT scores by patients ranged from 0 to 9 (Fig. 1). Physicians reported experiencing any moral distress in the care of 42% of patients (152/362). Most scores were low, with only 16.5% (60/362) having scores of 4 or higher (Fig. 1).
Moral Distress and Physician/Surrogate Treatment Preference Discordance
Physician and surrogates agreed about the preferred plan of treatment in 42.5% (151/362) of cases, with the physician preferring more aggressive treatment than surrogates in 31.3% (111/362) cases and more comfort than surrogates preferred in 26.2% (93/362) cases (Table 3). Physician surrogate discordance about the preferred plan of care was not significantly associated with moral distress in unadjusted analysis (Table 3) or when adjusted for physician, patient, and surrogate characteristics (Model 1, Table 4).
Moral Distress and Physician Characteristics
In adjusted analyses controlling for physician/surrogate discordance, and patient and surrogate characteristics, female physicians were less likely to experience moral distress than male physicians in the adjusted analysis (odds ratio (OR) 0.45; 95% confidence interval (CI) 0.21, 0.93; p = .0316; Model 1, Table 4).
Moral Distress and Patient/Surrogate Characteristics
Patient and surrogate characteristics that were significantly associated with having moral distress when controlling for other patient and surrogate characteristics and physician/surrogate discordance (Model 1, Table 4) included older patient age (1.06, 1.02–1.10; p = .0013) and facing a decision about life-sustaining treatment (3.58, 1.54–8.32; p = .0031). Physicians were less likely to report moral distress when caring for patients who reside in nursing homes (0.40, 0.23–0.69; p = .0010), patient previously discussing care preferences with anyone (0.56, 0.35–0.90; p = .0170), and higher surrogate ratings of emotional support from clinicians (0.94, 0.89–0.99; p = .0128). In the parallel model addressing physician internal discordance (Model 2, Table 4), there was a similar pattern of associations with moral distress for the patient and surrogate characteristics, except that having a living will was associated with lower physician moral distress (0.54, 0.31–0.94; p = .0305, Model 2, Table 4).
Moral Distress and Physician Preferred/Perceived Treatment Discordance
Physicians’ preferred and perceived plan of treatment was the same in 77.8% (281/362) cases (Table 2). The physician reported preferences for comfort care more often than they perceived the patient was receiving it in 21.6% (78/362) cases. The physician preferring more aggressive treatment was rare (0.6%, 2 cases) and was not included in multivariable analysis (Table 3). Physicians’ preferring a more comfort-focused plan than the patient was receiving were more likely to experience moral distress when adjusted for physician, patient, and surrogate characteristics (OR = 2.22, 95% CI 1.33–3.70; p = .0022, Table 3).
Sensitivity Analyses
For the sensitivity analyses, we analyzed the data after removing moral distress scores that were above a threshold, applying a different threshold in separate analyses (≥ 4, ≥ = 5, and equal to 10). In a separate analysis, we removed all of a physician’s data if their moral distress scores were all equal to zero or were all > = 8. Results from all sensitivity analyses were similar to those using the entire data, except that physician gender became marginally non-significant. No physician with four or more measurements had consistently high scores (4 or 5) or consistently low scores (0 or 1 or 2), with the exception of five physicians who had four or more measurements, all of which were zero.
Post hoc power analyses showed that, with an alpha of 0.05, the power for two-sided chi-square tests in logistic regression to detect the effect sizes, with the given sample sizes, observed in Table 3 between moral distress (yes/no) and discordance (3 categories) ranged from 78% for physician/surrogate discordance to 94% for physician preference/perceived discordance, with slightly less power than that after accounting for within-physician correlation.
DISCUSSION
This study helps characterize the patterns of physician moral distress found in the care of hospitalized older adults requiring a surrogate decision-maker. Most of the time, moral distress was rated as low to moderate. However, even low-grade moral distress may accumulate over time and have negative consequences.23 There is evidence that it is not just intensity of moral distress but the frequency of morally distressing situations that contributes to negative consequences for clinicians and patients.24, 25 Additionally, although highly distressing situations are uncommon, they are often salient and memorable. As the situation is resolved, acute moral distress decreases; however, a moral residue remains, raising a baseline level of moral distress, contributing to what Epstein and Hamric describe as the crescendo effect.23 A higher baseline level of moral residue can create higher crescendos, evoking more intense moral distress when encountering ethically challenging situations. Given that we found physicians reported moral distress in roughly half of cases when older adults required surrogates and was severe in some cases, interventions are needed to help prevent the cumulative effects over time.
Prevention efforts are important because clinician moral distress is correlated with secondary traumatic stress and burnout.13 The impact on patients is less well studied; however, high levels of moral distress are associated with poor relationships between physicians and nurses.26,27,28 Clinicians may also distance themselves from patients at a time when intense engagement, particularly clear communication is needed to improve end-of-life care.29
We found that male physicians were more likely to experience moral distress than female physicians. Junior physicians were more likely to experience moral distress than more senior physicians. This may be due to the hierarchical nature of medicine, particularly at training institutions. Junior level physicians may form an opinion about the course of treatment, however ultimately an attending physician is responsible for medical decisions. This may contribute to a feeling of powerlessness, a known contributor to the experience of moral distress.11, 12, 26 A larger study may be needed to further investigate this trend.
Consistent with prior literature, we found that an important cause of distress for physicians is feeling like the care plan includes more life-sustaining treatment than they believe is appropriate.17 The physician may experience discordance when they choose to honor a surrogate’s request for a particular plan of care even if the physician disagrees with it. This may be an ethically sound approach because ethical guidelines for surrogate decision-making give surrogates the authority to speak for the patient. However, it has been argued that physicians have an obligation to ensure that non-beneficial treatments are not provided to patients even if a surrogate prefers them.30, 31 Balancing these conflicting priorities may lead to moral distress .
Several patient factors were important predictors of moral distress. Consistent with other studies, our findings showed that physicians were more likely to experience moral distress in the care of patients who required decisions about life sustaining treatments.32, 33, 34 Our findings highlight that for hospitalized patients, as a patient’s age increases, so does the likelihood of physician moral distress. Advance care planning, in the form of conversations about patient preferences and living wills, was associated with reduced moral distress. This suggests that decisions about the treatment of incapacitated patients may be easier to achieve if the patient has previously expressed his or her own preferences for care. There is evidence that high quality advance care planning can affect the care of patients and reduce surrogate distress.35 Our study supports the hypothesis that advance care planning may also decrease moral distress for physicians.
Finally, we found a lower incidence of moral distress in cases when surrogates reported better emotional support from clinicians. The direction of cause and effect cannot be determined—physicians who are better communicators may also have less distress, or alternatively better communication may lead to lower physician-surrogate conflict and thus to lower incidence of physician moral distress. Further randomized controlled intervention research is needed to explore whether better emotional support of the surrogate could improve the decision-making process and reduce physician moral distress.
Physician moral distress is a cause of concern for the profession of medicine.36 It may also be an indicator of conflicting perceptions of the goals of care, differing opinions about how to best serve the patient and disappointment in the limited treatment options. Physicians’ ability to identify ethical concerns in the care of patients is necessary to high-quality medical treatment, but is insufficient if the physician feels constrained from carrying out an ethical plan of care. Future work is needed to determine whether interventions that provide decision-making support before and during the acute hospitalization can affect the plan of care and reduce moral distress. This may include existing interventions such as ethics or palliative care consultation or communication interventions to address advance care planning or in-hospital communication.37, 38, 39
This study has several limitations. We did not explore the particular causes of the discordance or the distress in each case. Future work could examine high distress cases using qualitative methods in order to explore situations where there is discordance. Future studies also could use the MMD-HP, a more detailed instrument that identifies contributing factors to and measures both intensity and frequency of moral distress.40 There may be other characteristics of physicians associated with distress that we did not measure. Our finding that physician/surrogate discordance was not found to be associated with moral distress may be due to the difference in the timing of data collection. Physicians were interviewed less than 96 h after admission, early on in the course of treatment, and surrogates were interviewed up to 10 days after admission when there may be more clarity around the plan of treatment. This suggests an opportunity for future research to explore impressions of the plan of treatment at the same point in time to better determine more precisely whether or not there is discordance between physicians and surrogates.
In conclusion, providers caring for older adults who must rely on surrogate decision-making experience moral distress about half the time, although most cases involve low to moderate distress. Physician moral distress in this setting is associated with physician, surrogate and patient characteristics, especially the need for decisions about life-sustaining treatments. Interventions to support physicians and improve the quality of decision-making could target these situations. Our data reveals that a particular aspect of the situation, namely when there is knowledge about a conversation about patient preferences, physicians are less likely to experience moral distress. Future research could investigate whether advance care planning and emotional support of surrogates could reduce the levels of physician moral distress.
References
Raymont V, Bingley W, Buchanan A, et al. Prevalence of mental incapacity in medical inpatients and associated risk factors: cross-sectional study. Lancet. 2004;364:1421–7.
Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306:420–7.
Torke AM, Sachs GA, Helft PR, et al. Scope and outcomes of surrogate decision making among hospitalized older adults. JAMA Intern Med. 2014;174:370–7.
Buchanan AE, Brock DW. Deciding for others: The ethics of surrogate decision making. Cambridge: Cambridge University Press; 1989.
Prendergast TJ. Resolving conflicts surrounding end-of-life care. New Horiz. 1997;5:62–71.
Emanuel EJ, Emanuel LL. Proxy decision making for incompetent patients. An ethical and empirical analysis. JAMA. 1992;267:2067–71.
Pellegrino ED. Patient and physician autonomy: conflicting rights and obligations in the physician-patient relationship. J Contemp Health Law Policy. 1994;10:47–68.
Torke AM, Siegler M, Abalos A, Moloney RM, Alexander GC. Physicians' experiences with surrogate decision making for hospitalized adults. J Gen Intern Med. 2009;24:1023–8.
Wendler D, Rid A. Systematic Review: The effects on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154:336–46.
Dudinski DM. Navigating moral distress using the moral distress map. J Med Ethics. 2016;42:321–3245.
Whitehead PB HR, Hamric AB, Epstein EG, Fisher JM. Moral distress among healthcare professionals: Report of an institution-wide survey. J Nurs Scholarsh. 2015;47:117–25.
Austin CL, Saylor R, Finley PJ. Moral distress in physicians and nurses: Impact on professional quality of life and turnover. Psychol Trauma. 2017;9:399–406.
Fumis RRL JAG, de Fátima Nascimento A, Vieira Junior JM. Moral distress and its contribution to the development of burnout syndrome among critical care physicians. Ann Intensive Care. 2017:71.
Henrich NJ, Dodek PM, Gladstone E, et al. Consequences of Moral Distress in the Intensive Care Unit: A Qualitative Study. Am J Crit Care. 2017;26:e48-e57.
Lamiani G, Dordoni P, Argentero P. Value congruence and depressive symptoms among critical care clinicians: The mediating role of moral distress. Stress and Health. 2018;34:135–42.
Dodek PM, Wong H, Norena M, et al. Moral distress in intensive care unit professionals is associated with profession, age, and years of experience. J Crit Care. 2016;31:178–82.
Dzeng E, Colaianni A, Roland M, et al. Moral Distress Amongst American Physician Trainees Regarding Futile Treatments at the End of Life: A Qualitative Study. J Gen Intern Med. 2016;31:93–9.
Torke AM, Monahan P, Callahan CM, et al. Validation of the family inpatient communication survey. J Pain Symptom Manage. 2017; 53(1):96–108.
Wocial LD, Weaver MT. Development and psychometric testing of a new tool for detecting moral distress: the Moral Distress Thermometer. J Adv Nurs. 2013;69:167–74.
Kroenke K, Spitzer RL, Williams JBW, Löwe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32 345–59.
Linn BS, Linn MW, Gurel L. Cummulative Illness Rating Scale. J Amer Geriatr Soc. 1968;16:622–6.
Salvi F, Miller MD, Grilli A, et al. A Manual of Guidelines to Score the Modified Cumulative Illness Rating Scale and Its Validation in Acute Hospitalized Elderly Patients. J Amer Geriatr Soc. 2008;56:1926–31.
Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20:330–42.
Gutierrez KM. Critical care nurses' perceptions of and responses to moral distress. Dimens Crit Care Nurs. 2005;24(5):229–41
McAndrew NS, Leske JS and Garcia A. Influence of moral distress on the professional practice environment during prognostic conflict in critical care. J Trauma Nurs. 2011; 18: 221–230.
Hamric AB, Borchers CT and Epstein EG. Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Prim Res. 2012; 3: 1–9.
Weinzimmer S, Miller SM, Zimmerman JL, et al. Critical care nurses’ moral distress in end-of-life decision making. J Nurs Educ Pract. 2014; 4: 6–12.
Wiegand D and Funk M. Consequences of clinical situations that cause critical care nurses to experience moral distress. Nurs Ethics. 2012; 19: 479–487.
De Villers MJ and DeVon HA. Moral distress and avoidance behavior in nurses working in critical care and noncritical care units. Nurs Ethics. 2013; 20: 589–603.
Bosslet GT, Pope TM, Rubenfeld GD, et al. An Official ATS/AACN/ACCP/ESICM/SCCM Policy Statement: Responding to Requests for Potentially Inappropriate Treatments in Intensive Care Units. Am J Respir Crit Care Med. 2015;191:1318–30.
Kon AA SE, Sederstrom NO, Swoboda SM, Marshall MF, Birriel B, Rincon F. . Defining futile and potentially inappropriate interventions: a policy statement from the Society of Critical Care Medicine Ethics Committee. Crit Care Med. 2016;44:1769–74.
Oberle K HD. Doctors’ and nurses’ perception of ethical problems in end-of-life decisions. J Adv Nurs. 2001;33:707–15.
Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit Care Med. 2007;35:422–9.
St Ledger U BA, Reid J, Prior L, McAuley D, Blackwood B. Moral distress in end-of-life care in the intensive care unit. J Adv Nurs. 2015;69:1868–80.
Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345.
Halpern SD. Perceived Inappropriateness of Care in the ICU: What to Make of the Clinician’s Perspective?. JAMA. 2011; 306:2725–6.
Schneiderman LJ. Effect of Ethics consultations on non-beneficial life-sustaining treatments in the intensive care setting: A randomized control trial. JAMA. 2003;290:1166–72.
Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11:180–90.
Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU.[see comment]. New Engl J Med. 2007;356:469–78.
Epstein EG, Whitehead PB, Prompahakul C, Thacker LR, Hamric AB. Enhancing Understanding of Moral Distress: The Measure of Moral Distress for Health Care Professionals. AJOB Empir Bioeth. 2019;2:113–124.
Funding
This study was funded by the Research in Palliative and End-of Life Communication and Training (RESPECT) Signature Center, Indiana University–Purdue University Indianapolis, the Greenwall Foundation, and The National Institute on Aging (R01 AG044408 and K24AG053794).
Author information
Authors and Affiliations
Contributions
Dr. Torke had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Torke, Sachs, Helft, Montz, Wocial, Callahan.
Acquisition of data: Torke, Montz.
Analysis and interpretation of data: All authors.
Drafting of the manuscript: Wocial, Torke, Slaven, Montz.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Torke, Slaven, Monahan
Obtained funding: Torke, Callahan.
Administrative, technical, or material support: Sachs, Helft, Montz, Callahan, Inger, Burke.
Study supervision: Sachs, Callahan.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentation
None.
Electronic supplementary material
ESM 1
(DOCX 25 kb)
Rights and permissions
About this article
Cite this article
Wocial, L.D., Slaven, J.E., Montz, K. et al. Factors Associated with Physician Moral Distress Caring for Hospitalized Elderly Patients Needing a Surrogate Decision-maker: a Prospective Study. J GEN INTERN MED 35, 1405–1412 (2020). https://doi.org/10.1007/s11606-020-05652-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-05652-1