Abstract
Background
Previous studies have suggested that a healthy lifestyle (HL) may prolong the years of life spent in good health. However, the impact of HL on disability-free survival (DFS) among the elderly is still uncertain.
Objective
To investigate the relationship between HL and DFS in the general elderly population.
Design
Prospective cohort study with a 10-year follow-up (2006–2016).
Participants
9910 community-dwelling elderly people (≥ 65 years).
Main Measures
A HL index derived by summing the number of HL behaviors. Data on incident disability were retrieved from the public Long-term Care Insurance database. Multivariate-adjusted 50th percentile differences (PDs) in age at disability or death (months) and their 95% CIs were estimated with the Laplace regression model.
Key Results
During the 10 years, 4562 disability or death events occurred. Participants who adhered to all three HL behaviors lived 17.1 (95% CI 12.7, 21.5) months longer without disability than those who adhered to zero or one. Each 1-point increase of the index score conferred 8.8 months additional life without disability. The tendency for the 50th PDs to increase with a higher HL index score did not differ according to age (< 75 or ≥ 75 years), sex, or the presence of chronic conditions (none, or ≥ 1 chronic condition).
Conclusions
A combination of HL behaviors may substantially increase DFS, even for late-elderly (≥ 75 years), or elderly people with chronic conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Rizzuto et al. found that healthy lifestyle (HL) behaviors were associated with longer survival.1 However, whether the extra years of life gained are spent in good health is a crucial issue that has not been addressed. May et al. reported that combined HL behaviors result in an increase in the number of years spent in good health (as measured in terms of disability-adjusted life years).2 However, in that study, the age of the participants ranged widely (between 20 and 70 years), which may have hindered accurate estimation of the impact of combined HL behaviors on incident disability and premature death among elderly people, especially those in late old age (≥ 75 years). Moreover, since participants with prevalent diseases at the baseline were excluded, it was not possible to assess the impact of combined HL behaviors among participants with chronic conditions, regardless of the high prevalence of chronic conditions among the elderly population.3 Therefore, it still remains undetermined whether combined HL behaviors are able to prolong disability-free survival (DFS) in the general elderly population.
Our previous study showed that combined HL behaviors (i.e., not current smoker, time spent walking ≥ 0.5 h/day, and vegetable and fruit consumption volume ≥ 270 g/day) are related to a lower risk of incident disability in the general elderly population.4 In the present study, we further estimated the relationship between combined HL behaviors and DFS with differences in median age at disability or death. This approach is informative because the results are expressed directly in the context of time (years), thus aiding communication and interpretation of the results.5
METHODS
Study Cohort
The design of the Ohsaki Cohort 2006 Study has been described in detail elsewhere.6 In brief, the source population for the baseline survey comprised 31,694 men and women aged ≥ 65 years who were living in Ohsaki City, northeastern Japan, on 1 December 2006. The survey included questions about lifestyle behaviors (including smoking, time spent walking, sleep time, and food consumption), as well as items on body weight, height, history of disease, education level, social support, motor function, and cognitive function.
The baseline survey was conducted between 1 and 15 December 2006, and follow-up of the participants began on 16 December 2006.
Healthy Lifestyle Index (Exposure)
In accordance with our previous study,4 a HL index (ranging from 0 to 3) was the summed number of the following variables: (1) never or former smoker; (2) time spent walking ≥ 0.5 h/day; (3) eating ≥ 270 g/day of fruit and vegetables (for more details, see Online Appendix). We categorized the HL index into three groups: (1) “0–1 point,” (2) “2 points,” and (3) “3 points.”
Follow-up and Case Ascertainment
We counted the person-years of follow-up for each subject from 16 December 2006 until the date of incident disability, the date of death, the date of emigration from Ohsaki City, or the end of the study period (30 November 2016), whichever occurred first.
A composite outcome was set as our primary endpoint, defined as Long-term Care Insurance (LTCI) certification (Support Level 1 or higher) or death (without LTCI certification). Considering that the relationship between HL index and incident disability may differ according to the severity of disability, a secondary composite outcome was defined as LTCI certification (Care Level 2 or higher, i.e., greater disability) or death (without LTCI certification).
All data pertaining to LTCI certification, death, or emigration were transferred from the Ohsaki City Government under the agreement related to Epidemiologic Research and Privacy Protection yearly each December.
The LTCI System in Japan
Japan uses a nationally uniform standard of functional disability. The LTCI is a form of mandatory social insurance to assist the frail and the elderly in their daily activities.7, 8 Everyone aged ≥ 40 years pays a premium, and everyone aged ≥ 65 years is eligible for formal caregiving services. When a person applies to the municipal government for benefits, a care manager visits his or her home and assesses the degree of functional disability using a questionnaire developed by the Ministry of Health, Labour and Welfare. The municipal government calculates the standardized scores for physical and mental function on the basis of the questionnaire and classifies the applicant as being eligible or ineligible for LTCI benefits (certification). If a person is judged to be eligible for benefits, the Municipal Certification Committee decides on one of the seven levels of support, ranging from Support Level 1, Support Level 2, and Care Level 1 to Care Level 5. In brief, LTCI certification levels are defined as follows: Support Level 1 is defined as “limited in instrumental activities of daily living but independent in basic activities of daily living (ADLs),” Care Level 2 is defined as “requiring assistance in at least one basic ADL task,” and Care Level 5 is defined as “requiring care in all ADL tasks.” A community-based study has shown that the level of LTCI certification is well correlated with ability to perform ADLs, and with the Mini-Mental State Examination score.9 A prospective study has also indicated that the level of LTCI certification is associated with mortality risk.10 LTCI certification has been used as a measure of incident functional disability in the elderly.11, 12
Covariates
Body mass index (BMI) was categorized into four groups: < 18.5, 18.5–25, ≥ 25 (kg/m2), and missing. Education level was assessed as “How old were you when you completed your education?” and answered using a positive integer. Based on the answer, we classified education level into four groups: < 16, 16–18, ≥ 19 (years), and missing.
The degree of social support available to each individual was assessed by a social support questionnaire consisting of five questions, each requiring a “yes” or “no” answer13: Do you have someone (1) with whom you can talk when you are in trouble, (2) whom you can consult when you do not feel well, (3) who can help you with your daily housework, (4) who can take you to a hospital when you feel ill, and (5) who can take care of you if you become bedridden? A validation study had reported that persons who responded “yes” had a higher average score on the Lubben Social Network Scale for each of these items.14
The Kihon Checklist was developed by the Ministry of Health, Labour and Welfare of Japan to predict functional decline in community-dwelling elderly. With regard to the motor function score in the Kihon Checklist, respondents were asked about their current motor function status using five binary questions, yielding total point scores ranging from 0 to 5. Based on the optimal cutoff point for functional decline suggested in the validation study, we classified individuals with scores of < 3 as having better motor function.15 With regard to the cognitive function score in the Kihon Checklist, respondents were asked about their current cognitive function status using three binary questions yielding total point scores ranging from 0 to 3. The validity of the cognitive function score in the Kihon Checklist had been confirmed in a previous study,16 and we classified individuals with scores of 0 as having better cognitive status.
Ethical Issues
We considered the return of completed questionnaires to imply consent to participate in the study involving the baseline survey data and subsequent follow-up of death and emigration. We also confirmed information regarding LTCI certification status after obtaining written consent along with the questionnaires returned from the subjects at the time of the baseline survey. The Ethics Committee of Tohoku University Graduate School of Medicine (Sendai, Japan) reviewed and approved the study protocol.
Statistical Analysis
The multivariate-adjusted Cox proportional hazards model was used to calculate the HRs and 95% confidence intervals (95% CI) for incident composite outcome, using age as the time scale (HL index of 0 or 1 was treated as the reference). Multivariate models were adjusted for sex, body mass index (in kg/m2; < 18.5, 18.5–25, ≥ 25, or missing), presence of chronic conditions (stroke, hypertension, myocardial infarction, diabetes, joint diseases, or cancer; yes/no, for each term), education level (age at last school graduation: < 16 years, 16–18 years, ≥ 19 years, or missing), social support situation (supported, not supported, or missing for each of five kinds of social support, separately), baseline motor function status (motor function score of the Kihon Checklist < 3, ≥ 3, or missing), and baseline cognitive function status (cognitive function score of the Kihon Checklist = 0, > 0, or missing).
Laplace regression was used to evaluate differences in DFS according to the HL index groups, by using attained age as the time scale.17 We focused our analysis on the 50th percentile of DFS (expressed in months), i.e., the median age at disability or death. Therefore, the measure of exposure-outcome association was defined as the 50th percentile difference (PD) in age. Laplace regression was adjusted for the same confounders as those in Cox plus age at the baseline (65–69, 70–74, 75–79, 80–84, or ≥ 85 years). Stratification analysis was then performed in relation to age (< 75 or ≥ 75 years), sex, and presence of chronic conditions (stroke, hypertension, myocardial infarction, diabetes, joint disease, and cancer; no chronic condition or ≥ 1 chronic condition) at the time of the baseline survey.
The analyses described above were applied for both primary and secondary composite outcomes. The Cox proportional hazards model was performed using SAS version 9.4 (SAS Inc., Cary, NC). Laplace regressions were performed by Stata/MP 14. All statistical tests described here were two-sided, and differences at P < 0.05 were accepted as significant.
RESULTS
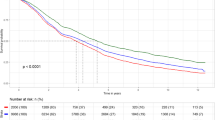
In this analysis, 9910 persons were included. Flow chart of participants is shown in Figure 1. During the 10-year period, only 141 persons were lost to follow-up because of migration from the study area, without developing incident functional disability, which provided a follow-up rate of 98.6%. Among 75,969 person-years, incident functional disability was determined for 3540 persons and the number of all-cause deaths without incident functional disability was 1022.
Baseline Characteristics
Among 9910 participants, 49.0% were men and 51.0% were women, and the mean (SD) age of the participants overall was 73.5 (6.0) years.
Healthy Lifestyle Index and Disability-Free Survival
After multivariate adjustment for potential confounders, a higher HL index score was associated with a lower risk of both primary and secondary composite outcomes and a longer DFS (Table 1). For primary composite outcome, the multivariate-adjusted 50th PD (95% CI) in age at incident disability or death for participants who had all three HL behaviors was 17.1 (12.7, 21.5) months older than those who had none or only one HL behavior. Each 1-point increase of the index score was associated with 8.8 additional months of life without disability (P trend < 0.001). For secondary composite outcome, the corresponding values were 23.3 (18.0, 28.6) and 12.6 (10.0, 15.3) (P trend < 0.001).
Healthy Lifestyle Index and Disability-Free Survival by Age, Sex, and Chronic Conditions
Stratified analyses of the association between HL index and composite outcomes were also conducted but the association did not differ according to age, sex, and presence of chronic conditions at the baseline (Figs. 2 and 3).
Multivariate-adjusted 50th percentile difference (PD) (95% CI) in age at incident disability (Support Level 1 or higher) or death stratified by age (< 75 or ≥ 75 years), sex, and presence of chronic conditions (stroke, hypertension, myocardial infarction, diabetes, joint disease, and cancer; no chronic condition or ≥ 1 chronic condition) at the time of the baseline survey.
Multivariate-adjusted 50th percentile difference (PD) (95% CI) in age at incident disability (Care Level 2 or higher, i.e., severer disability) or death stratified by age (< 75 or ≥ 75 years), sex, and presence of chronic conditions (stroke, hypertension, myocardial infarction, diabetes, joint disease, and cancer; no chronic condition or ≥ 1 chronic condition) at the time of the baseline survey.
DISCUSSION
In this prospective cohort study of 9910 elderly participants followed up for 10 years, an increase in the HL index score was associated with an increased number of years of disability-free life. In comparison with individuals who adhered to no HL behaviors or only one, those who adhered to all three HL behaviors lived an average of 17.1 months longer without disability. Each 1-point increase in the index score resulted in approximately 9 months of longer life without disability. This association did not differ after using greater disability and death as the composite outcome, according to age, sex, and presence of chronic conditions.
Our findings are consistent with a previous study that investigated the impact of HL on disability-adjusted life years.2 In that study, elderly persons (aged > 50 years) adhering to four HL characteristics enjoyed an average of 25 more months of improved health during their lifetime. Similar to our study, the exposure variable employed was a health behavior score obtained by summing points awarded for being a non-smoker, having a low BMI (< 25), being physically active, and adhering to a Mediterranean diet. However, in the present study, BMI was not chosen as a lifestyle factor because obese elderly accounted for a very low proportion of participants (only 2.7% had a BMI of > 30).
Our age-stratified results showed that an increased DFS period was still evident for late-elderly (≥ 75 years) participants with a higher HL index score. A previous study had reported a positive association between combined HL behaviors and longer survival in the late-elderly.1 However, the health status of long-lived individuals is an important issue. Our present findings could be considered as evidence that adherence to more HL behaviors would not only prolong life but also prolong healthy life, even in late old age.
It is also noteworthy that a similar relationship between the HL index score and DFS period was observed among participants with and without chronic conditions. Although the DFS period would differ according to baseline health conditions,18 our results demonstrated that the impact of combined HL behaviors on DFS is independent of health status. That is, even for elderly people with chronic conditions, adherence to more HL behaviors resulted in comparable benefits by preventing disability and premature death.
Our study had a number of strengths: (1) in the present study, differences in DFS were quantified by estimating the 50th PD of attained age.5, 19 Such quantitative measurements could help the general public to interpret the results and might also assist the implementation of public health policy encouraging the public to adhere to HL behaviors, (2) disability was defined as LTCI certification, and the time until disability onset was accurately known, and (3) the follow-up rate was almost 100%.
Several limitations should also be considered. First, because lifestyle behaviors were assessed at the baseline, we were unable to take into account changes during the follow-up period. Second, because not all candidates applied for LTCI certification, this study may not have been completely free from detection bias. Third, ignoring missing data in complete case analysis may have led to biased estimates. However, the small differences in the results for complete case and multiple imputation analyses suggested that missing data had little impact on our findings (Online Supplementary Table). Fourth, not all key lifestyle behaviors (such as a diet high in sodium20) accounting for differences in DFS were assessed in the present study, and further evaluation is therefore required. Finally, different cultural and biological backgrounds of individuals living in other areas may affect the extrapolation of our results. Further studies in different settings are expected in the future.
In conclusion, the present study has found an association between combined HL behaviors and increased DFS among elderly people. This association was consistently evident among both young-elderly (< 75 years) and late-elderly (≥ 75 years) people, men and women, and elderly with and without chronic conditions. Our findings suggest that encouraging HL behaviors even in old age may enhance health in later life by reducing the incidence of disability and premature death.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Rizzuto D, Orsini N, Qiu C, Wang H-X, Fratiglioni L. Lifestyle, social factors, and survival after age 75: population based study. BMJ. 2012;345. https://doi.org/10.1136/bmj.e5568.
BMC MedMay AM, Struijk EA, Fransen HP, Onland-Moret NC, de Wit GA, Boer JM, et al. The impact of a healthy lifestyle on Disability-Adjusted Life Years: a prospective cohort study. BMC Med. 2015;13:39. https://doi.org/10.1186/s12916-015-0287-6.
Organization WH. World report on ageing and health. Geneva: World Health Organization; 2015.
Zhang S, Tomata Y, Newson RB, Sugawara Y, Tsuji I. Combined healthy lifestyle behaviours and incident disability in an elderly population: the Ohsaki Cohort 2006 Study. J Epidemiol Community Health. 2018. https://doi.org/10.1136/jech-2018-210464.
Orsini N, Wolk A, Bottai M. Evaluating percentiles of survival. Epidemiology. 2012;23(5):770–1. https://doi.org/10.1097/EDE.0b013e3182625eff.
Kuriyama S, Nakaya N, Ohmori-Matsuda K, Shimazu T, Kikuchi N, Kakizaki M, et al. The Ohsaki Cohort 2006 Study: design of study and profile of participants at baseline. J Epidemiol. 2010;20(3):253–8. https://doi.org/10.2188/jea.JE20090093.
Imai H, Fujii Y, Fukuda Y, Nakao H, Yahata Y. Health-related quality of life and beneficiaries of long-term care insurance in Japan. Health Policy. 2008;85(3):349–55. https://doi.org/10.1016/j.healthpol.2007.08.008.
Ministry of Health LaW. Long-term care insurance in Japan. Ministry of Health, Labour and Welfare, Ministry of Health, Labour and Welfare. 2008. http://www.mhlw.go.jp/english/topics/elderly/care/index.html. Accessed 29 Mar. 2019.
Arai Y, Zarit SH, Kumamoto K, Takeda A. Are there inequities in the assessment of dementia under Japan’s LTC insurance system? Int J Geriatr Psychiatry. 2003;18:346–52.
Takeda S. Two-year survival and changes in the level of care for the elderly patients recognized as in need of long-term care in the public nursing-care insurance scheme. Nippon Koshu Eisei Zasshi. 2004;51:157–67.
Hozawa A, Sugawara Y, Tomata Y, Kakizaki M, Ohmori-Matsuda K, Nakaya N, et al. Relationships between N-terminal pro B-type natriuretic peptide and incident disability and mortality in older community-dwelling adults: the Tsurugaya study. J Am Geriatr Soc. 2010;58(12):2439–41. https://doi.org/10.1111/j.1532-5415.2010.03190.x.
Nitta A, Hozawa A, Kuriyama S, Nakaya N, Ohmori-Matsuda K, Sone T, et al. Relationship between peripheral arterial disease and incident disability among elderly Japanese: the Tsurugaya Project. J Atheroscler Thromb. 2010;17(12):1290–6.
Muraoka Y, Oiji A, Ihara K. The physical and psychological and social background factor of elderly depression in the community. Ronen Seishin Igaku Zasshi. 1996;7:397–407.
Kurimoto A, Awata S, Ohkubo T, Tsubota-Utsugi M, Asayama K, Takahashi K, et al. Reliability and validity of the Japanese version of the abbreviated Lubben Social Network Scale. Nihon Ronen Igakkai zasshi. Jpn J Geriatr. 2011;48(2):149–57.
Tomata Y, Hozawa A, Ohmori-Matsuda K, Nagai M, Sugawara Y, Nitta A, et al. [Validation of the Kihon Checklist for predicting the risk of 1-year incident long-term care insurance certification: the Ohsaki Cohort 2006 Study]. Nihon Koshu Eisei Zasshi. 2011;58(1):3–13.
Meguro K, Team. KP. The validity of the Basic Checklist in the old-old population: The Kurihara Project. Jpn J Geriatr Psychiatry. 2012:725–30.
Bellavia A, Discacciati A, Bottai M, Wolk A, Orsini N. Using laplace regression to model and predict percentiles of age at death when age is the primary time scale. Am J Epidemiol. 2015;182(3):271–7. https://doi.org/10.1093/aje/kwv033.
Crimmins EM, Hayward MD, Hagedorn A, Saito Y, Brouard N. Change in disability-free life expectancy for Americans 70-years-old and older. Demography. 2009;46(3):627–46.
Uno H, Claggett B, Tian L, Inoue E, Gallo P, Miyata T, et al. Moving beyond the hazard ratio in quantifying the between-group difference in survival analysis. J Clin Oncol. 2014;32(22):2380–5. https://doi.org/10.1200/JCO.2014.55.2208.
Network GBoDC. Global Burden of Disease Study 2017 (GBD 2017) Burden by Risk 1990-2017. In: (IHME) IfHMaE, editor. Seattle, United State; 2018.
Acknowledgments
We would like to thank Yoshitaka Murakami, Shuji Hashimoto, Toshiyuki Ojima, Jun Aida, Takahiro Tabuchi, Naoki Kondo, Tetsuji Yokoyama, and Kazuyo Tsushita for their valuable comments. We are also grateful to Yoshiko Nakata and Mami Takahashi for technical assistance.
Funding
This work was supported by Health Sciences Research grants (no. H28-Junkankitou-Ippan-008) from the Ministry of Health, Labour and Welfare of Japan.
Author information
Authors and Affiliations
Contributions
IT and SZ designed the research; IT and YT conducted the research; SZ and AD analyzed the data; SZ wrote the manuscript; YT, AD, TO, YS, FT, and IT gave constructive suggestions; SZ had primary responsibility for the final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The Ethics Committee of Tohoku University Graduate School of Medicine (Sendai, Japan) reviewed and approved the study protocol.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer
Sponsors play no role in the design, methods, subject recruitment, data collections, analysis, and preparation of the paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, S., Tomata, Y., Discacciati, A. et al. Combined Healthy Lifestyle Behaviors and Disability-Free Survival: the Ohsaki Cohort 2006 Study. J GEN INTERN MED 34, 1724–1729 (2019). https://doi.org/10.1007/s11606-019-05061-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05061-z