Abstract
Background
This study aimed to evaluate the perioperative outcomes of patients undergoing robot-assisted McKeown esophagectomy (RAME) and the learning curves of surgeons performing RAME at a single center.
Methods
Perioperative outcomes of RAME and video-assisted McKeown esophagectomy (VAME) were compared after eliminating confounding factors by propensity score matching (PSM). The cumulative sum (CUSUM) method was used to evaluate the learning curves of RAME for a single surgical team.
Results
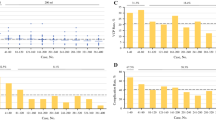
In general, a total of 198 patients with esophageal cancer (RAME: 45 patients, VAME: 153 patients) were included in this study, and 43 pairs of patients receiving RAME or VAME were matched using 1:1 PSM analysis. Those in the RAME group had more lymph nodes dissected in the total lymph nodes (median 29.0 vs. 26.0, P = 0.011) and the upper mediastinum (median 8.0 vs. 6.0, P < 0.001), especially the left recurrent laryngeal nerve (RLN) lymph node (median 4.0 vs. 2.0, P = 0.001). According to the trend of the CUSUM plot, the learning curve was divided into two stages at the 20th RAME procedure. After mastering the learning curve, RAME harvested a significantly higher number of upper mediastinal lymph nodes (median 9.0 vs. 6.0, P = 0.001), left RLN lymph nodes (median 5.0 vs. 3.5, P = 0.003), and right RLN lymph nodes (median 4.0 vs. 2.0, P = 0.002). Meanwhile, the incidence of postoperative pneumonia in the proficiency phase was significantly lower than that in the learning phase (4.0% vs. 25.0%, P = 0.04).
Conclusions
RAME improved left RLN lymph node dissection. Surgeons with extensive VAME experience need at least 20 cases to achieve early proficiency in RAME.


Similar content being viewed by others
References
Galldiks N, Niyazi M, Grosu AL, et al. Contribution of PET imaging to radiotherapy planning and monitoring in glioma patients - a report of the PET/RANO group. Neuro Oncol 2021;23:881-893.
Domper Arnal MJ, Ferrandez Arenas A, Lanas Arbeloa A. Esophageal cancer: Risk factors, screening and endoscopic treatment in Western and Eastern countries. World J Gastroenterol 2015;21:7933-43.
Grille VJ, Campbell S, Gibbs JF, et al. Esophageal cancer: the rise of adenocarcinoma over squamous cell carcinoma in the Asian belt. J Gastrointest Oncol 2021;12:S339-S349.
Pennathur A, Gibson MK, Jobe BA, et al. Oesophageal carcinoma. Lancet 2013;381:400-12.
Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92.
Haverkamp L, Seesing MF, Ruurda JP, et al. Worldwide trends in surgical techniques in the treatment of esophageal and gastroesophageal junction cancer. Dis Esophagus 2017;30:1-7.
Chen J, Liu Q, Zhang X, et al. Comparisons of short-term outcomes between robot-assisted and thoraco-laparoscopic esophagectomy with extended two-field lymph node dissection for resectable thoracic esophageal squamous cell carcinoma. J Thorac Dis 2019;11:3874-3880.
van der Sluis PC, van der Horst S, May AM, et al. Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer: a randomized controlled trial. Ann Surg 2019;269:621-630.
Deng HY, Luo J, Li SX, et al. Does robot-assisted minimally invasive esophagectomy really have the advantage of lymphadenectomy over video-assisted minimally invasive esophagectomy in treating esophageal squamous cell carcinoma? A propensity score-matched analysis based on short-term outcomes. Dis Esophagus 2019;32.
Hosoda K, Niihara M, Ushiku H, et al. Prevention of intra-thoracic recurrent laryngeal nerve injury with robot-assisted esophagectomy. Langenbecks Arch Surg 2020;405:533-540.
de Groot EM, van der Horst S, Kingma BF, et al. Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open esophagectomy: long-term follow-up of a randomized clinical trial. Dis Esophagus 2020;33.
van der Sluis PC, Ruurda JP, Verhage RJ, et al. Oncologic long-term results of robot-assisted minimally invasive thoraco-laparoscopic esophagectomy with two-field lymphadenectomy for esophageal cancer. Ann Surg Oncol 2015;22 Suppl 3:S1350-6.
D'Journo XB. Clinical implication of the innovations of the 8(th) edition of the TNM classification for esophageal and esophago-gastric cancer. J Thorac Dis 2018;10:S2671-S2681.
Sun HB, Li Y, Liu XB, et al. Early Oral Feeding Following McKeown Minimally Invasive Esophagectomy: An Open-label, Randomized, Controlled, Noninferiority Trial. Ann Surg 2018;267:435-442.
Sun HB, Li Y, Liu XB, et al. Embedded three-layer esophagogastric anastomosis reduces morbidity and improves short-term outcomes after esophagectomy for cancer. Ann Thorac Surg 2016;101:1131-8.
Low DE, Alderson D, Cecconello I, et al. International consensus on standardization of data collection for complications associated with esophagectomy: esophagectomy complications consensus group (ECCG). Ann Surg 2015;262:286-94.
Kubo Y, Tanaka K, Yamasaki M, et al. Influences of the Charlson Comorbidity Index and nutrition status on prognosis after esophageal cancer surgery. Ann Surg Oncol 2021;28:7173-7182.
He H, Wu Q, Wang Z, et al. Short-term outcomes of robot-assisted minimally invasive esophagectomy for esophageal cancer: a propensity score matched analysis. J Cardiothorac Surg 2018;13:52.
Chao YK, Hsieh MJ, Liu YH, et al. Lymph node evaluation in robot-assisted versus video-assisted thoracoscopic esophagectomy for esophageal squamous cell carcinoma: a propensity-matched analysis. World J Surg 2018;42:590-598.
Motoyama S, Sato Y, Wakita A, et al. Extensive lymph node dissection around the left laryngeal nerve achieved with robot-assisted thoracoscopic esophagectomy. Anticancer Res 2019;39:1337-1342.
Yang Y, Li B, Yi J, et al. Robot-assisted versus conventional minimally invasive esophagectomy for resectable esophageal squamous cell carcinoma: early results of a multicenter randomized controlled trial: the RAMIE Trial. Ann Surg 2022;275:646-653.
Xu ZJ, Zhuo ZG, Song TN, et al. Pretreatment-assisted robot intrathoracic layered anastomosis: our exploration in Ivor-Lewis esophagectomy. J Thorac Dis 2021;13:4349-4359.
van der Sluis PC, Tagkalos E, Hadzijusufovic E, et al. Robot-assisted minimally invasive esophagectomy with intrathoracic anastomosis (Ivor Lewis): promising results in 100 consecutive patients (the European Experience). J Gastrointest Surg 2021;25:1-8.
Thammineedi SR, Patnaik SC, Reddy P, et al. The emerging role of ICG fluorescence during minimally invasive esophagectomy. Indian J Surg Oncol 2021;12:635-636.
Zhang H, Chen L, Wang Z, et al. The learning curve for robotic McKeown Esophagectomy in Patients With Esophageal Cancer. Ann Thorac Surg 2018;105:1024-1030.
Han Y, Zhang Y, Zhang W, et al. Learning curve for robot-assisted Ivor Lewis esophagectomy. Dis Esophagus 2022;35.
Funding
This study was funded by the Province-Ministry Co-construction Project of Health Committee of Henan Province (SB201901108), Talent Youth Project of Henan Youth Health Science and Technology Innovation Foundation (YXKC2020022), and Henan Province Key Project of Science and Technology (222102310170).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare that no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, HB., Jiang, D., Liu, XB. et al. Perioperative Outcomes and Learning Curve of Robot-Assisted McKeown Esophagectomy. J Gastrointest Surg 27, 17–26 (2023). https://doi.org/10.1007/s11605-022-05484-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05484-w