Abstract
Introduction
Total neoadjuvant therapy (TNT) is a new therapeutic strategy in patients with rectal cancer. We examined the role of TNT, in addition to other pre-operative factors, as a predictor for pathologic complete response (pCR).
Methods
A retrospective analysis of all rectal cancer patients who underwent surgery between 2016 and 2021 was conducted. Patients were classified into two groups—pCR group and residual tumor group. Patient data were reviewed and entered into univariate and multivariate analyses to determine predictors of pCR.
Results
A total of 172 patients were treated with neoadjuvant therapy and underwent surgery during the study period. Sixty patients (34.9%) were treated with TNT while 112 (65.1%) were treated with traditional neoadjuvant chemoradiation. The overall pCR rate was 25.6% (44 patients), with 31.6% (19 patients) in patients who received TNT compared to 22.3% (25 patients) in patients who received neoadjuvant chemoradiation (NCRT). Univariate analysis of clinical and radiological factors correlated with pCR demonstrated no significant differences between the two groups in cT stage (p = 0.46), cN stage (p = 0.52), positive circumferential resection margin (CRM) (p = 0.72), tumor location (p = 0.35), symptomatic presentation (p = 0.09), and anal sphincter involvement (p = 0.68). Multivariate logistic analysis demonstrated that only pre-operative TNT (OR:2.35; 95% CI 1.06–5.25; p = 0.03) was predictive of pCR, while extramural vascular invasion (EMVI) was a predictor for lower rates of pCR (OR: 0.28; 95% CI 0.09–0.9; p = 0.03).
Conclusion
Rectal cancer patients undergoing TNT prior to surgery have a higher chance of developing a complete pathologic response. Evaluation of this therapy should be continued and extended to larger numbers of patients to see if the differences we observed are real.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the most common types of cancer throughout the world. Approximately one third of the 150,000 new colorectal cancer cases annually diagnosed in the USA are rectal cancers.1 Treatment for rectal cancer has evolved. The implementation of total mesorectal excision (TME), the introduction of neoadjuvant therapy, and the multidisciplinary team (MDT) management have improved the outcomes of rectal cancer patients.2,3 Furthermore, the clinical and radiological assessment of rectal cancer has changed. The widespread use of novel imaging modalities such as high resolution thin slice magnetic resonance imaging (MRI) and 3D transanal ultrasonography provide clinicians with additional tools for evaluation, thus allowing a more accurate and tailored treatment.4,5
Neoadjuvant therapy of rectal cancer, which includes pre-operative radiation therapy often combined with a single chemotherapeutic agent, has become the standard of care. Several studies have demonstrated that neoadjuvant chemoradiation therapy (NCRT) could significantly reduce the likelihood of local recurrence following TME.6,7 With the widespread implementation of NCRT as the standard of care, approximately 15–25% of patients who were treated with NCRT prior to surgery had no traces of neoplastic cells in the pathological specimen, a phenomenon widely known as pathological complete response (pCR).8,9 This finding has led to the introduction of a new therapeutic strategy of watch and wait that omits surgery, with its significant implication on patients’ quality of life. It includes close clinical, radiological, and endoscopic follow-up in patients who achieve a complete response.10,11,12
Recent studies showed that patients with locally advanced rectal cancer treated with total neoadjuvant chemotherapy (TNT) were more likely to complete the treatment protocol.13,14 The higher treatment response rates associated with TNT could also improve overall survival and reduce the likelihood of disease recurrence.15 Although TNT has been introduced as the preferred therapeutic option for patients with locally advanced rectal cancer and has been recommended by the clinical guidelines of many associations and cancer-focused organizations, including the National Accreditation Program for Rectal Cancer (NAPRC)16 and the National Comprehensive Cancer Network (NCCN),17 there are little data about the effect TNT has on the patient’s pathological response.
In this study, we aimed to assess possible factors associated with complete pathological response in patients with locally advanced rectal cancer treated with neoadjuvant therapy prior to surgery. Based on the recent changes in rectal cancer therapy, we presumed that TNT played a significant role in achieving complete pathological response following surgery. We analyzed the different therapeutic approaches in addition to other clinical and radiological pre-operative factors, to assess their role as predictors for pathologic complete response (pCR).
Methods
We retrospectively analyzed an Institutional Review Board (IRB)-approved (FLA 19–077) prospective database of patients with rectal cancer who underwent surgery of curative intent in the Department of Colorectal Surgery at Cleveland Clinic Florida. This study was approved by the IRB at Cleveland Clinic Florida. We included all adult patients who underwent surgical resection of the rectum for rectal cancer and were treated with neoadjuvant therapy prior to surgery over 6 years (October 2016 to October 2021). Patients treated with a watch and wait protocol following neoadjuvant therapy were excluded from the final analysis as we did not have their TME pathological results. Therefore, we excluded these patients from our final analysis. The cohort was divided into two groups, based on the pathological outcomes following surgery—the pathological non-complete response (pNCR) group and the pCR group. We excluded all patients with metastatic rectal cancer, patients with unknown stage, and those who underwent treatments other than TME, including watch and wait protocol. In addition, we excluded all patients who were treated with surgery alone, without pre-operative neoadjuvant therapy.
Study Outcomes
The primary outcome of the study was the rate of pCR in rectal cancer patients who were treated with neoadjuvant therapy. Secondary outcomes included the percentage of patients treated with standard NCRT compared to TNT and the effect on the pathological outcomes. Another secondary outcome was to perform a multivariate analysis to recognize predictive factors of pCR following neoadjuvant treatment. Unfortunately, oncological outcomes were not assessed in our study owning to short follow-up that may preclude accurate analysis.
Evaluation and Treatment of Rectal Cancer
The diagnostic process of patients who presented to our institute with rectal cancer included a complete physical examination with a digital rectal examination performed by a board-certified colorectal surgeon, and full colonoscopic evaluation with biopsies from suspected lesions to confirm the diagnosis of rectal cancer. If the diagnosis was made prior to referral to our institute, pathology reports and slides, endoscopy reports and photographic images, and imaging reports and radiologic images were obtained and reviewed. We defined low rectal cancer as lesions lower than 5 cm from the anal verge, middle location as within 5–10 cm, and high rectal cancer between 11 and 15 cm from the anal verge. All patients were both locally and systemically staged. Local staging was performed with MRI, using a standard protocol according to the NAPRC.16 Systemic staging was mainly performed with chest-abdominal-pelvic computerized tomography and positron emission tomography (PET-CT), if clinically required. All patients were discussed in the weekly NAPRC MDT meeting which includes colorectal surgeons, radiologists, pathologists, and medical and radiation oncologists. MDT discussions and decision-making in our institute follow the NCCN guidelines and the NAPRC recommendations. TNT has been adopted and increasingly employed at our institution in recent years. Furthermore, we recently published a study about the treatment of rectal cancer during the COVID-19 era, which demonstrated a significant increase in TNT during this time period. We noticed an increase in TNT as in the first phases of the pandemic, as patients were more often referred to TNT to preserve healthcare resources.18
Treatment of locally advanced rectal cancer (T3–4, N0, or node-positive) with NCRT consisted of long-course standard radiotherapy (54 Gy) and 5 weeks of concurrent 5 fluorouracil or capecitabine. TNT consisted of 6–8 cycles of modified FOLOFOX6 or 5–6 cycles of CAPOX. All patients included in the study were first given induction chemotherapy followed by long-course chemoradiation therapy. The elective nodal volumes received 45Gy and included the mesorectum, obturator, internal iliac, and presacral nodes. The external iliac nodes were included at the discretion of the treating radiation oncologist for T4 disease. The gross tumor volume received a boost dose of 50.4Gy–54Gy; no patients were treated with short course radiation. Following treatment, all patients were reassessed clinically and with a repeat pelvic MRI and were re-presented in MDT discussion for a concise decision based on the outcomes of the neoadjuvant treatment. Surgical treatment included open, laparoscopic, or transanal approaches including transanal TME (TaTME), with or without an anastomosis, based on tumor location and infiltration of the surrounding structures.
Statistical Analysis
Data were analyzed with SPSS™ (IBM Corp; v23). Continuous data were expressed as mean and standard deviation when normally distributed, otherwise as median and range. Categorical data were expressed as numbers and proportions. Continuous data analysis was undertaken by the Student t-test and analysis of categorical data by the Fisher exact test or chi-square test.
A univariate analysis identified the significant factors associated with pCR; factors with a p value of less than 0.25 were entered into a multivariable binary logistic regression analysis to determine the independent predictors of pCR. We considered p values less than 0.05 as significant.
Results
192 (78.7%) of 244 patients treated for rectal cancer, were treated with neoadjuvant therapy. Twenty patients were excluded from the study as they were followed by a watch and wait protocol and did not undergo TME surgery. A total of 172 patients (70.5%) who were treated with neoadjuvant therapy followed by TME surgery were included in our analysis. The study flowchart can be seen in Fig. 1. Sixty patients (34.9%) were treated with TNT, and 112 patients (65.1%) were treated with NCRT prior to surgery. The median interval of time from neoadjuvant therapy to surgery was 13.2 (range, 4–52) weeks.
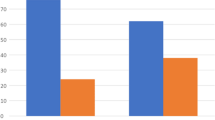
Overall, pCR was achieved in 44 patients (25.6%), whereas 128 patients (74.4%) had a residual tumor in the pathologic specimens. There were no significant differences between the two groups in terms of demographics such as age (58.3 vs. 59.3 years, p = 0.64), sex (p = 0.99), American Society of Anesthesiologist (ASA) score (p = 0.78), and mean body mass index (BMI) (26.5 vs 26.8, p = 0.69). The rate of pCR was 31.6% in the TNT group and 22.3% in the standard NCRT group (p = 0.2).
Univariate analysis of pre-operative clinical and radiological parameters demonstrated no significant differences between the two groups. Pre-operative clinical factors including cT stage (p = 0.46), cN stage (p = 0.52), and positive circumferential resection margin (CRM) (p = 0.72) were all comparable between the groups. Although non-significant, we noticed that the rate of positive extramural vascular invasion (EMVI) was higher in the non-complete response group (22.6% vs 9.1%; p = 0.07). Sphincter involvement was also similar between the groups, when the external sphincter (2.2% vs. 5.4%; p = 0.68) and the internal sphincter (15.9% vs 21%; p = 0.51) were involved. A comparison of patients’ demographic and pre-operative data can be seen in Table 1.
The majority of patients in both groups underwent sphincter-preserving low anterior resection or coloanal anastomosis (84.1% vs 75.8%; p = 0.29) using a laparoscopic approach (86.3% vs. 81.2%; p = 0.49). TME specimen completeness (88.6% vs. 80.4%; p = 0.25) and number of harvested lymph nodes (23.2 vs 25.1; p = 0.46) were comparable between the groups. The surgical outcomes are detailed in Table 2.
Multivariate logistic analysis demonstrated that only pre-operative TNT (OR:2.35; 95% CI 1.06–5.25; p = 0.03) was predictive of pCR, while extramural vascular invasion (EMVI) was a predictor for lower rates of pCR (OR: 0.28; 95% CI 0.09–0.9; p = 0.03). The multivariate analysis can be seen in Table 3.
Discussion
Modern rectal cancer treatment includes three primary treatment modalities—radiotherapy, chemotherapy, and surgical resection. Combining these three modalities has led to increased survival and higher rates of curative resection.7 Chemotherapy, which was given following surgery in the pre-TNT protocols, was often delayed or not administered at all in certain patients, especially those who suffered from significant surgical complications.19,20,21 Pre-operative consolidation and induction chemotherapy, as part of the TNT protocol, increases the likelihood of treatment completion, translating into overall improved oncological outcomes.2
Furthermore, in some cases, non-operative treatment is so efficient that some patients can defer the surgical resection and avoid surgical morbidity, thereby improving their quality of life.10 As a result, many studies in recent years started focusing on this group of patients to try and stratify possible predictive factors that will enable a complete response to pre-operative therapy. Assessment of these factors could hopefully help clinicians to identify potential candidates for a watch and wait management.22,23,24
In this study, we analyzed factors associated with a complete pathological response to pre-operative neoadjuvant treatment in patients with locally advanced rectal cancer. Despite the limited cohort of patients, we found that pre-operative TNT increased the likelihood of patients to achieve a complete pathological response, compared to standard NCRT. Furthermore, we performed a logistic regression analysis that demonstrated that TNT was the only predictor of higher rates of pCR. At the same time, positive EMVI in the staging MRI was a predictor of lower probability of complete pathological response. Unfortunately, perhaps due to the relatively small sample size, none of these differences achieved statistical significance.
None of the other factors we investigated showed a similar correlation with pCR. Tumor size,25 clinical T and N stage,26 tumor grade,27 circumferential involvement, and tumor shape28 were all equivocal in patients who achieved pCR and those who did not, despite previous descriptions in the literature regarding their possible predictive role for pCR. However, it is plausible that a small sample size did not allow enough power to detect significant associations between these factors and pCR. Moreover, all of these factors are already determined prior to presenting with rectal cancer, highlighting the importance of TNT as the main interventional factor associated with an increased response to therapy.
Our study has several limitations, including its retrospective single-center nature, lack of long-term oncological outcomes, and sample size. In addition, we excluded patients followed up with a watch and wait protocol to minimize possible bias associated with the lack of pathological assessment in these patients. However, despite these limitations, our study suggests potential advantages for implementing TNT as the primary therapeutic strategy in patients with locally advanced rectal cancer. Surgeons and other caregivers treating these patients must be aware that TNT improves the probability for a complete response, and be meticulous in the post-TNT follow-up, given the increased likelihood of a pCR and the chance to avoid surgery.
Conclusion
Patients with rectal cancer undergoing TNT prior to surgery have a higher chance of developing complete pathologic response. Evaluation of this therapy should be continued and extended to validate these observations.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA: a Cancer Journal for Clinicians. 2020;70(1):70:7–30.
Cercek A, Roxburgh CSD, Strombom P, et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncology. 2018;4: e180071.
Riesco-Martinez MC, Fernandez-Martos C, et al. Impact of total neoadjuvant therapy vs. Standard chemoradiotherapy in locally advanced rectal cancer: A systematic review and meta-analysis of randomized trials. Cancers. 2020;12:3655
Coppola F, Giannini V, Gabelloni M, et al. Radiomics and magnetic resonance imaging of rectal cancer: From engineering to clinical practice. Diagnostics. 2021;11:756.
Reginelli A, Clemente A, Sangiovanni A, et al. Endorectal ultrasound and magnetic resonance imaging for rectal cancer staging: A modern multimodality approach. J Clin Med. 2021;10:641.
Folkesson J, Birgisson H, Pahlman L, Cedermark B, Glimelius B, Gunnarsson U. Swedish rectal cancer trial: Long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol. 2005;23:5644-5650.
Keller DS, Berho M, Perez RO, Wexner SD, Chand M. The multidisciplinary management of rectal cancer. Nature Rev Gastroenterol Hepatol. 2020;17:414-429.
Naiken SP, Toso C, Rubbia-Brandt L, et al. Complete pathological response (ypT0N0M0) after pre-operative chemotherapy alone for stage IV rectal cancer. BMC Surgery. 2014;14:4.
Wilson K, Flood M, Narasimhan V, et al. Complete pathological response in rectal cancer utilising novel treatment strategies for neo-adjuvant therapy: A systematic review. Eur J Surg Oncol. 2021;47:1862-1874.
Dattani M, Heald RJ, Goussous G, et al. Oncological and survival outcomes in Watch and Wait patients with a clinical complete response after neoadjuvant chemoradiotherapy for rectal cancer a systematic review and pooled analysis. Ann Surg. 2018;268:955-967.
São Julião GP, Habr-Gama A, Vailati BB, Araujo SEA, Fernandez LM, Perez RO. New Strategies in Rectal Cancer. Surg Clin North Am. 2017;97:587-604.
Habr-Gama A, Lynn PB, Jorge JMNJ, et al. Impact of Organ-Preserving Strategies on Anorectal Function in Patients with Distal Rectal Cancer Following Neoadjuvant Chemoradiation. Dis Colon Rectum. 2016;59:264-269.
Ludmir EB, Palta M, Willett CG, Czito BG. Total neoadjuvant therapy for rectal cancer: An emerging option. Cancer. 2017;123:1497-1506.
Shiao JC, Fakhoury KR, Olsen J. Total Neoadjuvant Therapy for Rectal Cancer: Current Status and Future Directions. Current Colorectal Cancer Reports. 2020;16:125-134.
Thompson H, Kim JK, Yuval JB, et al. Survival and organ preservation according to clinical response after total neoadjuvant therapy in locally advanced rectal cancer patients: A secondary analysis from the organ preservation in rectal adenocarcinoma (OPRA) trial. Journal of Clinical Oncology. 2021;39:3509.
Commission on Cancer National Accreditation Program for Rectal cancer 2020 Standards and Resources. https://www.facs.org/quality-programs/cancer/naprc/standards/2020. Accessed 16 Jul 2021
Benson AB, Venook AP, Al-Hawary MM, et al. Rectal Cancer, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2018;16:874-901.
Freund MR, Kent I, Horesh N, et al. The effect of the first year of the COVID-19 pandemic on sphincter preserving surgery for rectal cancer: A single referral center experience. Surgery. 2022171:1209-1214.
Nachiappan S, Askari A, Mamidanna R, et al. Initiation of adjuvant chemotherapy within 8 weeks of elective colorectal resection improves overall survival regardless of reoperation. Colorectal Dis. 2016;18:1041-1049.
Thong DW, Kim J, Naik A, Lu CT, Nolan GJ, von Papen M. Delay to Adjuvant Chemotherapy: Survival and Recurrence in Patients of Rectal Cancer Treated with Neo-adjuvant Chemoradiotherapy and Surgery. Journal of Gastrointestinal Cancer. 2020;51:877-886.
Cheung WY, Neville BA, Earle CC. Etiology of delays in the initiation of adjuvant chemotherapy and their impact on outcomes for stage II and III rectal cancer. Dis Colon Rectum. 2009;52:1054-1063.
Sanghera P, Wong DWY, McConkey CC, Geh JI, Hartley A. Chemoradiotherapy for Rectal Cancer: An Updated Analysis of Factors Affecting Pathological Response. Clin Oncol. 2008;20:176-183.
Maas M, Nelemans PJ, Valentini V, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: A pooled analysis of individual patient data. Lancet Oncol. 2010;11:834-844.
Hajer J, Rim A, Ghorbel A, et al. Predictive factors associated with complete pathological response after neoadjuvant treatment for rectal cancer. Cancer/Radiotherapie. 2021;25:259-267.
Huang Y, Lee D, Young C. Predictors for complete pathological response for stage II and III rectal cancer following neoadjuvant therapy - A systematic review and meta-analysis. Am J Surg. 2020;220:300-308.
Hammarström K, Imam I, Mezheyeuski A, Ekström J, Sjöblom T, Glimelius B. A comprehensive evaluation of associations between routinely collected staging information and the response to (Chemo)radiotherapy in rectal cancer. Cancers. 2021;13:16.
Jang JK, Choi SH, Park SH, et al. MR tumor regression grade for pathological complete response in rectal cancer post neoadjuvant chemoradiotherapy: a systematic review and meta-analysis for accuracy. Eur Radiol. 2020;30:2312-2323.
Jayanand SB, Seshadri RA, Tapkire R. Signet ring cell histology and non-circumferential tumors predict pathological complete response following neoadjuvant chemoradiation in rectal cancers. Int J Colorectal Dis. 2011;26:23-27.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
SDW is a consultant for ICON Language Services, Intuitive Surgical, Stryker, Medtronic, Takeda, ARC/Corvus, Baxter, LivsMed, GI Supply, and Leading BioSciences/PalisadeBio; and receives royalties from Medtronic, Intuitive Surgical, Karl Storz Endoscopy America Inc., and Unique Surgical Innovations LLC. All other authors have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Horesh, N., Freund, M.R., Garoufalia, Z. et al. Total Neoadjuvant Therapy Is a Predictor for Complete Pathological Response in Patients Undergoing Surgery for Rectal Cancer. J Gastrointest Surg 26, 2579–2584 (2022). https://doi.org/10.1007/s11605-022-05463-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05463-1