Abstract
Background
Obesity is epidemic in the USA. Limited data exist examining obesity’s influence on necrotizing pancreatitis (NP) disease course.
Methods
Retrospective review of prospectively maintained database of 571 adult necrotizing pancreatitis patients treated between 2007 and 2018. Patients were grouped according to body mass index (BMI) at disease onset. Patient characteristics, necrotizing pancreatitis course, and outcomes were compared between non-obese (BMI < 30) and obese (BMI > 30) patients.
Results
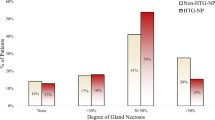
Among 536 patients with BMI data available, 304 (57%) were obese (BMI > 30), and 232 (43%) were non-obese (BMI < 30). NP etiology in the obese group was more commonly biliary (55% versus 46%, p = 0.04) or secondary to hypertriglyceridemia (10% versus 2%, p < 0.001) and less commonly alcohol (17% versus 26%, p = 0.01). Obese patients had a higher incidence of baseline comorbid disease. The CT severity index was similar between groups though obese patients had a higher rate of > 50% pancreatic gland necrosis (27% versus 19%, p = 0.02). The rates of infected necrosis and organ failure were higher among obese patients. Percutaneous drainage was more common in obese patients. Time to first necrosis intervention was earlier with increasing BMI. NP disease duration was longer in obese patients. The overall mortality rate of non-obese and obese patients did not differ. However, mortality rate increased with increasing BMI.
Conclusion
Necrotizing pancreatitis in obese patients is characterized by a prolonged disease course, a higher risk of organ failure, infected necrosis, and the need for early necrosis-related intervention. Mortality increases with increasing BMI.




Similar content being viewed by others
References
Ogden CL, C.M., Fryar CD, Flegal KM, Prevalence of Obesity Among Adults and Youth: United States, 2011-2014. NCHS Data Brief 2015. 219: p. 1-8.
Khatua, B., B. El-Kurdi, and V.P. Singh, Obesity and pancreatitis. Curr Opin Gastroenterol, 2017. 33(5): p. 374-382.
Maatman TK, R.A., Ceppa EP, Easler JJ, Gromski MA, House MG, Nakeeb A, Schmidt CM, Sherman S, Zyromski NJ. , The continuum of complications in survivors of necrotizing pancreatitis. Surgery, 2020. 168(6): p. 1032-1040.
Roch, A.M., et al., Percutaneous Gastrostomy in Necrotizing Pancreatitis: Friend or Foe? J Gastrointest Surg 24(12) 2800-2806.
Roch, A.M., et al., Venous Thromboembolism in Necrotizing Pancreatitis: an Underappreciated Risk. J Gastrointest Surg, 2019. 23(12): p. 2430-2438.
Maatman, T.K., et al., Prospective Analysis of the Mechanisms Underlying Ineffective Deep Vein Thrombosis Prophylaxis in Necrotizing Pancreatitis. J Am Coll Surg., 2021. 232(1): p. 91-100.
Balthazar, E., et al., Acute Pancreatitis: Value of CT in Establishing Prognosis. Radiology, 1990. 174(2): p. 331-6.
Gürleyik, G., et al., Computed tomography severity index, APACHE II score, and serum CRP concentration for predicting the severity of acute pancreatitis. Jop, 2005. 6(6): p. 562-7.
Banks, P.A., et al., Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut, 2013. 62(1): p. 102-11.
Working Group IAP/APA Acute Pancreatitis Guidelines, IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology, 2013. 13(4 Suppl 2): p. e1-15.
Mortele, K.J., et al., A Modified CT Severity Index for Evaluating Acute Pancreatitis: Improved Correlation with Patient Outcome. AJR Am J Roentgenol, 2004. 183(5): p. 1261-5.
Marshall, J., et al., Multiple Organ Dysfunction Score: A Reliable Descriptor of a Complex Clinical Outcome. Critical Care Medicine, 1995. 23(10): p. 1638-52.
Kozarek, R. and L. Traverso, Pancreatic fistulas: etiology, consequences, and treatment. Gastroenterologist, 1996. 4(4): p. 239-44.
Sandrasegaran, K., et al., Disconnection of the Pancreatic Duct: An Important But Overlooked Complication of Severe Acute Pancreatitis. Radiographics, 2007. 27(5): p. 1389-400.
Prevention, C.f.D.C.a. Overweight and Obesity 2019 [cited 2021 May 3 ]; Available from: https://www.cdc.gov/obesity/index.html.
Papachristou, G.I., et al., Obesity increases the severity of acute pancreatitis: performance of APACHE-O score and correlation with the inflammatory response. Pancreatology, 2006. 6(4): p. 279-85.
Johnson, C.D., S.K. Toh, and M.J. Campbell, Combination of APACHE-II score and an obesity score (APACHE-O) for the prediction of severe acute pancreatitis. Pancreatology, 2004. 4(1): p. 1-6.
Chen, S.M., G.S. Xiong, and S.M. Wu, Is obesity an indicator of complications and mortality in acute pancreatitis? An updated meta-analysis. J Dig Dis, 2012. 13(5): p. 244-51.
Premkumar, R., et al., The clinical relevance of obesity in acute pancreatitis: targeted systematic reviews. Pancreatology, 2015. 15(1): p. 25-33.
Choi, J., L. Joseph, and L. Pilote, Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev, 2013. 14(3): p. 232-44.
Marques-Vidal, P., et al., Association between inflammatory and obesity markers in a Swiss population-based sample (CoLaus Study). Obes Facts, 2012. 5(5): p. 734-44.
Zyromski, N.J., et al., A murine model of obesity implicates the adipokine milieu in the pathogenesis of severe acute pancreatitis. Am J Physiol Gastrointest Liver Physiol, 2008. 295(3): p. G552-8.
Navina, S., et al., Lipotoxicity causes multisystem organ failure and exacerbates acute pancreatitis in obesity. Sci Transl Med, 2011. 3(107): p. 107ra110.
Yashima, Y., et al., A large volume of visceral adipose tissue leads to severe acute pancreatitis. J Gastroenterol, 2011. 46(10): p. 1213-8.
Mullen, J.T., D.W. Moorman, and D.L. Davenport, The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg, 2009. 250(1): p. 166-72.
Patel, J.J., et al., The Critical Care Obesity Paradox and Implications for Nutrition Support. Curr Gastroenterol Rep, 2016. 18(9): p. 45.
Rossi, A.P., et al., Predictors of ectopic fat accumulation in liver and pancreas in obese men and women. Obesity (Silver Spring), 2011. 19(9): p. 1747-54.
Nguyen, N.H., et al., Annual Burden and Costs of Hospitalization for High-Need, High-Cost Patients With Chronic Gastrointestinal and Liver Diseases. Clin Gastroenterol Hepatol, 2018. 16(8): p. 1284-1292.e30.
Meng, L., et al., Comprehensive Guidance for Antibiotic Dosing in Obese Adults. Pharmacotherapy, 2017. 37(11): p. 1415-1431.
Zhang, T., et al., Gut Dysbiosis in Pancreatic Diseases: A Causative Factor and a Novel Therapeutic Target. Front Nutr, 2022. 9: p. 814269.
Wu, L.M., et al., Meta-analysis of gut barrier dysfunction in patients with acute pancreatitis. Br J Surg, 2014. 101(13): p. 1644-56.
Thomas, R.M. and C. Jobin, Microbiota in pancreatic health and disease: the next frontier in microbiome research. Nat Rev Gastroenterol Hepatol, 2020. 17(1): p. 53-64.
Author information
Authors and Affiliations
Contributions
SP McGuire, SL Keller, TK Maatman, and KA Lewellen were involved in acquisition, analysis, and interpretation of data. SP McGuire and NJ Zyromski drafted and revised the manuscript. SP McGuire, TK Maatman, EP Ceppa, MG House, A Nakeeb, TK Nguyen, SN Quigley, CM Schmidt, and NJ Zyromski were involved in the conception of the project, interpretation of the data, and revision of work. All authors were involved in the final approval. NJ Zyromski serves as the mentor and corresponding author and agrees to be accountable for the work.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was presented at the Digestive Disease Week in May 2021.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McGuire, S.P., Keller, S.L., Maatman, T.K. et al. Obesity Worsens Local and Systemic Complications of Necrotizing Pancreatitis and Prolongs Disease Course. J Gastrointest Surg 26, 2128–2135 (2022). https://doi.org/10.1007/s11605-022-05383-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05383-0