Abstract
Background
Prior studies assessing colorectal cancer survival have reported better outcomes when operations are performed at high-volume centers. These studies have largely been cross-sectional, making it difficult to interpret their estimates. We aimed to assess the effect of facility volume on survival following proctectomy for rectal cancer.
Methods
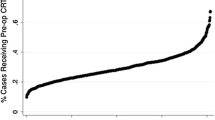
Using data from the National Cancer Database, we included all patients with complete baseline information who underwent proctectomy for non-metastatic rectal cancer between 2004 and 2016. Facility volume was defined as the number of rectal cancer cases managed at the treating center in the calendar year prior to the patient’s surgery. Overall survival estimates were obtained for facility volumes ranging from 10 to 100 cases/year. Follow-up began on the day of surgery and continued until loss to follow-up or death.
Results
A total of 52,822 patients were eligible. Patients operated on at hospitals with volumes of 10, 30, and 50 cases/year had similar distributions of grade, clinical stage, and neoadjuvant therapies. 1-, 3-, and 5-year survival all improved with increasing facility volume. One-year survival was 94.0% (95% CI: 93.7, 94.3) for hospitals that performed 10 cases/year, 94.5% (95% CI: 94.2, 94.7) for 30 cases/year, and 94.8% (95% CI: 94.5, 95.0) for 50 cases/year. Five-year survival was 68.9% (95% CI: 68.0, 69.7) for hospitals that performed 10 cases/year, 70.8% (95% CI: 70.1, 71.5) for 30 cases/year, and 72.0% (95% CI: 71.2, 72.8) for 50 cases/year.
Conclusions
Treatment at a higher volume facility results in improved survival following proctectomy for rectal cancer, though the small benefits are less profound than previously reported.






Similar content being viewed by others
References
NCCN. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Rectal Cancer June 2020.
Archampong D, Borowski D, Wille-Jørgensen P, Iversen LH. Workload and surgeon´s specialty for outcome after colorectal cancer surgery. Cochrane Database of Systematic Reviews. 2012(3). doi:https://doi.org/10.1002/14651858.CD005391.pub3.
Vonlanthen R, Lodge P, Barkun JS, Farges O, Rogiers X, Soreide K et al. Toward a Consensus on Centralization in Surgery. Ann Surg. 2018;268(5):712-24. doi:https://doi.org/10.1097/sla.0000000000002965.
Huo YR, Phan K, Morris DL, Liauw W. Systematic review and a meta-analysis of hospital and surgeon volume/outcome relationships in colorectal cancer surgery. Journal of Gastrointestinal Oncology. 2017;8(3):534-46.
Sheetz KH, Dimick JB, Nathan H. Centralization of High-Risk Cancer Surgery Within Existing Hospital Systems. Journal of Clinical Oncology. 2019;37(34):3234-42. doi:https://doi.org/10.1200/jco.18.02035.
Hamidi M, Hanna K, Omesiete P, Cruz A, Ewongwo A, Pandit V et al. Does it matter where you get your surgery for colorectal cancer? International Journal of Colorectal Disease. 2019;34(12):2121-7. doi:https://doi.org/10.1007/s00384-019-03436-6.
Borowski DW, Bradburn DM, Mills SJ, Bharathan B, Wilson RG, Ratcliffe AA et al. Volume-outcome analysis of colorectal cancer-related outcomes. Br J Surg. 2010;97(9):1416-30. doi:https://doi.org/10.1002/bjs.7111.
van Gijn W, Gooiker GA, Wouters MW, Post PN, Tollenaar RA, van de Velde CJ. Volume and outcome in colorectal cancer surgery. Eur J Surg Oncol. 2010;36 Suppl 1:S55-63. doi:https://doi.org/10.1016/j.ejso.2010.06.027.
ACS. National Cancer Database. American College of Surgeons. https://www.facs.org/quality-programs/cancer/ncdb. Accessed November 17 2020.
Leapfrog Ratings: Complex Adult Surgery. The Leapfrog Group. 2020. https://ratings.leapfroggroup.org/measure/hospital/complex-adult-surgery. Accessed February 21 2021.
Urbach DR. Pledging to Eliminate Low-Volume Surgery. N Engl J Med. 2015;373(15):1388-90. doi:https://doi.org/10.1056/NEJMp1508472.
Bilimoria KY, Bentrem DJ, Feinglass JM, Stewart AK, Winchester DP, Talamonti MS et al. Directing Surgical Quality Improvement Initiatives: Comparison of Perioperative Mortality and Long-Term Survival for Cancer Surgery. Journal of Clinical Oncology. 2008;26(28):4626-33. doi:https://doi.org/10.1200/jco.2007.15.6356.
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R et al. Preoperative versus Postoperative Chemoradiotherapy for Rectal Cancer. New England Journal of Medicine. 2004;351(17):1731-40. doi:https://doi.org/10.1056/NEJMoa040694.
Habr-Gama A, Gama-Rodrigues J, São Julião GP, Proscurshim I, Sabbagh C, Lynn PB et al. Local recurrence after complete clinical response and watch and wait in rectal cancer after neoadjuvant chemoradiation: impact of salvage therapy on local disease control. Int J Radiat Oncol Biol Phys. 2014;88(4):822-8. doi:https://doi.org/10.1016/j.ijrobp.2013.12.012.
Appelt AL, Pløen J, Harling H, Jensen FS, Jensen LH, Jørgensen JC et al. High-dose chemoradiotherapy and watchful waiting for distal rectal cancer: a prospective observational study. Lancet Oncol. 2015;16(8):919-27. doi:https://doi.org/10.1016/s1470-2045(15)00120-5.
Lee JK, Doumouras AG, Springer JE, Eskicioglu C, Amin N, Cadeddu M et al. Examining the transferability of colon and rectal operative experience on outcomes following laparoscopic rectal surgery. Surgical Endoscopy. 2020;34(3):1231-6. doi:https://doi.org/10.1007/s00464-019-06885-w.
NCI. NCI-Designated Cancer Centers. In: Cancer Research Infrastructure. National Cancer Institute. 2019. https://www.cancer.gov/research/infrastructure/cancer-centers. Accessed January 31 2021.
Hernán MA, Robins JM. Using Big Data to Emulate a Target Trial When a Randomized Trial Is Not Available. Am J Epidemiol. 2016;183(8):758-64. doi:https://doi.org/10.1093/aje/kwv254.
García-Albéniz X, Hsu J, Hernán MA. The value of explicitly emulating a target trial when using real world evidence: an application to colorectal cancer screening. Eur J Epidemiol. 2017;32(6):495-500. doi:https://doi.org/10.1007/s10654-017-0287-2.
Lodi S, Phillips A, Lundgren J, Logan R, Sharma S, Cole SR et al. Effect Estimates in Randomized Trials and Observational Studies: Comparing Apples With Apples. Am J Epidemiol. 2019;188(8):1569-77. doi:https://doi.org/10.1093/aje/kwz100.
Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615-25. doi:https://doi.org/10.1097/01.ede.0000135174.63482.43.
Reames BN, Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and operative mortality in the modern era. Ann Surg. 2014;260(2):244-51. doi:https://doi.org/10.1097/sla.0000000000000375.
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I et al. Hospital Volume and Surgical Mortality in the United States. New England Journal of Medicine. 2002;346(15):1128-37. doi:https://doi.org/10.1056/NEJMsa012337.
Author information
Authors and Affiliations
Contributions
All authors had substantial contributions to the conception or design of the work; or to acquisition, analysis, or interpretation of data; and to drafting or revision of the work. All authors made final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An earlier version of this work was presented as a display e-poster at the Massachusetts Chapter of the American College of Surgeons (MCACS) 67th Annual Meeting (held virtually December 5, 2020), and as a Virtual Quickshot Presentation at the 16th Annual Academic Surgical Congress (ASC) (held virtually February 2–4, 2021).
Rights and permissions
About this article
Cite this article
Welten, .M., Wanis, K.N., Madenci, A.L. et al. The Effect of Facility Volume on Survival Following Proctectomy for Rectal Cancer. J Gastrointest Surg 26, 150–160 (2022). https://doi.org/10.1007/s11605-021-05092-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05092-0