Abstract
Background
Inter-hospital transfer (IHT) may help reduce failure-to-rescue (FTR) by transferring patients to centers with a higher level of expertise than the index hospital. We sought to identify factors associated with an IHT and examine if IHT was associated with improved outcomes after complex gastrointestinal cancer surgery.
Methods
Medicare Inpatient Standard Analytic Files were utilized to identify patients with >1 postoperative complication following resection for esophageal, pancreatic, liver, or colorectal cancer between 2013 and 2017. Multivariable logistic regression was used to examine the association of different factors with the chance of IHT, as well as the impact of IHT on failure-to-rescue (FTR) and expenditures.
Results
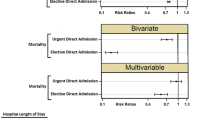
Among 39,973 patients with >1 postoperative complications, 3090 (7.7%) patients were transferred to a secondary hospital. The median LOS at the index hospital prior to IHT was 10 days (IQR, 6–17 days). Patients who underwent IHT more often had experienced multiple complications at the index hospital compared with non-IHT patients (57.7% vs. 38.9%) (p<0.001). Transferred patients more commonly had undergone surgery at a low-volume index hospital (n=218, 60.2%) compared with non-IHT (n=10,351, 25.9%) patients (p<0.001). On multivariate analysis, hospital volume remained strongly associated with transfer to an acute care hospital (ACH) (OR 5.53; 95% CI 3.91–7.84; p<0.001), as did multiple complications (OR 2.01, 95% CI 1.56–2.57). The incidence of FTR was much higher among IHT-ACH patients (20.2%) versus non-IHT patients (11.5%) (OR 1.51, 95% CI 1.11–2.05) (p<0.001). Medicare expenditures were higher among patients who had IHT-ACH ($72.1k USD; IQR, $48.1k–$116.7k) versus non-IHT ($38.5k USD; IQR, $28.1k–$59.2k USD) (p<0.001).
Conclusion
Approximately 1 in 13 patients had an IHT after complex gastrointestinal cancer surgery. IHT was associated with high rates of FTR, which was more pronounced among patients who underwent surgery at an index low-volume hospital. IHT was associated with higher overall CMS expenditures.


Similar content being viewed by others
References
Finks JF, Osborne NH, Birkmeyer JD. Trends in Hospital Volume and Operative Mortality for High-Risk Surgery. New England Journal of Medicine. New England Journal of Medicine; 2011;364(22):2128–37.
Sheetz KH, Massarweh NN. Centralization of High-risk Surgery in the US. JAMA. JAMA; 2020;324(4):339.
Jacobs RC, Groth S, Farjah F, Wilson MA, Petersen LA, Massarweh NN. Potential impact of “take the volume pledge” on access and outcomes for gastrointestinal cancer surgery. Annals of Surgery. Annals of Surgery; 2019.
Sheetz KH, Chhabra KR, Smith ME, Dimick JB, Nathan H. Association of Discretionary Hospital Volume Standards for High-risk Cancer Surgery With Patient Outcomes and Access, 2005-2016. JAMA Surgery. JAMA Surgery; 2019;154(11):1005.
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, et al.. Hospital Volume and Surgical Mortality in the United States. New England Journal of Medicine. New England Journal of Medicine; 2002;346(15):1128–37.
Gottlieb-Vedi E, Mattsson F, Lagergren P, Lagergren J. Annual hospital volume of surgery for gastrointestinal cancer in relation to prognosis. European Journal of Surgical Oncology. European Journal of Surgical Oncology; 2019;45(10):1839–46.
Begg CB. Impact of Hospital Volume on Operative Mortality for Major Cancer Surgery. JAMA. JAMA; 1998;280(20):1747.
El Amrani M, Clement G, Lenne X, et al. Failure-to-rescue in patients undergoing pancreatectomy: Is hospital volume a standard for quality improvement programs? nationwide analysis of 12,333 patients. Annals of Surgery. Annals of Surgery; 2018;268(5):799-807.
O’Connor SC, Mogal H, Russell G, Ethun C, Fields RC, Jin L, et al.. The Effects of Travel Burden on Outcomes After Resection of Extrahepatic Biliary Malignancies: Results from the US Extrahepatic Biliary Consortium. Journal of Gastrointestinal Surgery. Journal of Gastrointestinal Surgery; 2017;21(12):2016–24.
Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB, Meropol NJ. Centralization of Cancer Surgery: Implications for Patient Access to Optimal Care. Journal of Clinical Oncology. Journal of Clinical Oncology; 2009;27(28):4671–8.
El Amrani M, Lenne X, Clément G, et al. Referring patients to expert centers after pancreatectomy is too late to improve outcome. inter-hospital transfer analysis in nationwide study of 19,938 patients. Annals of Surgery. Annals of Surgery; 2020;272(5):723 730.
Mueller SK, Zheng J, Orav EJ, Schnipper JL. Rates, Predictors and Variability of Interhospital Transfers: A National Evaluation. Journal of Hospital Medicine [Internet]. Journal of Hospital Medicine; 2017;12(6):435–42. Available from: https://doi.org/10.12788/jhm.2747
Mueller SK, Zheng J, Orav J, Schnipper JL. Interhospital Transfer and Receipt of Specialty Procedures. Journal of Hospital Medicine [Internet]. Journal of Hospital Medicine; 2017;. Available from: https://doi.org/10.12788/jhm.2875
Emergency Medical Treatment & Labor Act (EMTALA). CMS.gov. Published on March 2012. https://www.cms.gov/Regulations-and-Guidance/Legislation/EMTALA. Accessed on December 15, 2020.
Gupta K, Mueller SK. Interhospital transfers: The need for standards. Journal of Hospital Medicine [Internet]. Journal of Hospital Medicine; 2015;10(6):415–7. Available from: https://doi.org/10.1002/jhm.2320
Reimer AP, Schiltz NK, Ho VP, Madigan EA, Koroukian SM. Applying Supervised Machine Learning to Identify Which Patient Characteristics Identify the Highest Rates of Mortality Post-Interhospital Transfer. Biomedical Informatics Insights [Internet]. Biomedical Informatics Insights; 2019;11:117822261983554. Available from: https://doi.org/10.1177/1178222619835548
Mueller SK, Fiskio J, Schnipper J. Interhospital Transfer: Transfer Processes and Patient Outcomes. Journal of Hospital Medicine [Internet]. Journal of Hospital Medicine; 2019;14(8):486–91. Available from: https://doi.org/10.12788/jhm.3192
Silber JH, Romano PS, Rosen AK, Wang Y, Even-Shoshan O, Volpp KG. Failure-to-rescue: comparing definitions to measure quality of care. Medical Care. Medical Care; 2007 Oct;45(10):918-25.
Spolverato G, Ejaz A, Hyder O, Kim Y, Pawlik TM. Failure to rescue as a source of variation in hospital mortality after hepatic surgery. British Journal of Surgery. British Journal of Surgery; 2014;101(7):836–46.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al.. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. American Journal of Epidemiology [Internet]. American Journal of Epidemiology; 2011;173(6):676–82. Available from: https://doi.org/10.1093/aje/kwq433
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care. Medical Care; 2005 Nov;43(11):1130-9.
Merath K, Chen Q, Bagante F, Akgul O, Idrees JJ, Dillhoff M, et al.. Synergistic Effects of Perioperative Complications on 30-Day Mortality Following Hepatopancreatic Surgery. Journal of Gastrointestinal Surgery. Journal of Gastrointestinal Surgery; 2018;22(10):1715–23
Mavros MN, De Jong M, Dogeas E, Hyder O, Pawlik TM. Impact of complications on long-term survival after resection of colorectal liver metastases. British Journal of Surgery. British Journal of Surgery; 2013;100(5):711–8.
Ghaferi, Amir, Birkmeyer, John, Dimick, Justin, MD, MPH. Complications, Failure to Rescue, and Mortality with Major Inpatient Surgery in Medicare Patients. Annals of Surgery. Annals of Surgery; 2009;250(6):1029-1034.
Amini N, Spolverato G, Kim Y, Pawlik TM. Trends in Hospital Volume and Failure to Rescue for Pancreatic Surgery. Journal of Gastrointestinal Surgery. Journal of Gastrointestinal Surgery; 2015;19(9):1581–92.
Chen Q, Beal EW, Kimbrough CW, Bagante F, Merath K, Dillhoff M, et al.. Perioperative complications and the cost of rescue or failure to rescue in hepato-pancreato-biliary surgery. HPB [Internet]. HPB; 2018;20(9):854–64. Available from: https://doi.org/10.1016/j.hpb.2018.03.010
Lucas DJ, Ejaz A, Haut ER, Spolverato G, Haider AH, Pawlik TM. Interhospital Transfer and Adverse Outcomes after General Surgery: Implications for Pay for Performance. Journal of the American College of Surgeons. Journal of the American College of Surgeons; 2014;218(3):393–400.
Mackenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al.. A National Evaluation of the Effect of Trauma-Center Care on Mortality. New England Journal of Medicine. New England Journal of Medicine; 2006;354(4):366–78.
Ingraham A, Reinke CE. Optimizing Safety for Surgical Patients Undergoing Interhospital Transfer. Surgical Clinics of North America. Surgical Clinics of North America; 2021;101(1):57–69.
Sharp SP, Ata A, Valerian BT, Canete JJ, Chismark AD, Lee EC. Complications and surgical outcomes after interhospital transfer vs direct admission in colorectal surgery: A National Surgical Quality Improvement Program analysis. The American Journal of Surgery. The American Journal of Surgery; 2017;213(6):1031–7.
Chen Q, Olsen G, Bagante F, Merath K, Idrees JJ, Akgul O, et al.. Procedure-Specific Volume and Nurse-to-Patient Ratio: Implications for Failure to Rescue Patients Following Liver Surgery. World Journal of Surgery. World Journal of Surgery; 2019;43(3):910–9.
Hyer, J. M., Paredes, A. Z., Tsilimigras, D., & Pawlik, T. M. Is Hospital Occupancy Rate Associated with Postoperative Outcomes Among Patients Undergoing Hepatopancreatic Surgery? Annals of surgery. Annals of surgery, 2020. 10.1097/SLA.0000000000004418. Advance online publication. https://doi.org/10.1097/SLA.0000000000004418
Diaz A, Chavarin D, Paredes AZ, Pawlik TM. Utilization of High-Volume Hospitals for High-Risk Cancer Surgery in California Following Medicaid Expansion. Journal of Gastrointestinal Surgery. Journal of Gastrointestinal Surgery; 2020;.
Golestanian E, Scruggs JE, Gangnon RE, et al. Effect of interhospitaltransfer on resource utilization and outcomes at a tertiary care referralcenter. Crit Care Med 2007;35:1470–6
Huntington CR, Cox TC, Blair LJ, Prasad T, Lincourt AE, Matthews BD, et al.. Acuity, outcomes, and trends in the transfer of surgical patients: a national study. Surgical Endoscopy. Surgical Endoscopy; 2016;30(4):1301–9.
Santry HP, Janjua S, Chang Y, Petrovick L, Velmahos GC. Interhospital Transfers of Acute Care Surgery Patients: Should Care for Nontraumatic Surgical Emergencies be Regionalized?. World Journal of Surgery. World Journal of Surgery; 2011;35(12):2660–7.
Outcome measures. CMS.gov. Published on February 2020. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures. Accessed on Decemeber 16, 2020.
PSI #4 Death among Surgical Inpatients with Serious Treatable Complications. AHRQ Quality Indicators Web Site: https://qualityindicators.ahrq.gov/Downloads/Modules/PSI/V41/TechSpecs/PSI%2004%20Death%20among%20Surgical%20Inpatients.pdf. Accessed on December 18, 2020.
Leeds IL, Kachalia A, Haut ER. Rescuing Failure to Rescue—Patient Safety Indicator 04 on the Brink of Obsolescence. JAMA Surgery. JAMA Surgery; 2020;.
NQF-endorsed measures for surgical procedures, 2015-2017 National Quality Forum. Published April 20, 2017. http://www.qualityforum.org/WorkArea/linkit.aspx? Accessed December 18, 2020.
Mohr NM, Harland KK, Shane DM, Ahmed A, Fuller BM, Torner JC. Inter-hospital transfer is associated with increased mortality and costs in severe sepsis and septic shock: An instrumental variables approach. Journal of Critical Care [Internet]. Journal of Critical Care; 2016;36:187–94. Available from: https://doi.org/10.1016/j.jcrc.2016.07.016
Aguayo E, Kwon OJ, Dobaria V, Sanaiha Y, Hadaya J, Sareh S, et al.. Impact of interhospital transfer on clinical outcomes and costs of extracorporeal life support. Surgery. Surgery; 2020;168(1):193–7.
Schlesinger-Raab A, Werner J, Friess H, Hölzel D, Engel J. Age and Outcome in Gastrointestinal Cancers: A Population-Based Evaluation of Oesophageal, Gastric and Colorectal Cancer. Visceral Medicine. Visceral Medicine; 2017;33(4):245–53.
Rawla P, Sunkara T, Gaduputi V. Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. World Journal of Oncology [Internet]. World Journal of Oncology; 2019;10(1):10–27. Available from: https://doi.org/10.14740/wjon1166
Altekruse SF, Henley JS, Cucinelli JE, Mcglynn KA. Changing Hepatocellular Carcinoma Incidence and Liver Cancer Mortality Rates in the United States. American Journal of Gastroenterology [Internet]. American Journal of Gastroenterology; 2014;109(4):542–53. Available from: https://doi.org/10.1038/ajg.2014.11
Author information
Authors and Affiliations
Contributions
PP, DD, and TMP conceived of and designed this work. DD performed data analysis. PP, DIT, and TMP drafted the manuscript. PP, JMH, DIT, AD, and TMP critically revised the manuscript, provided approval of the final version, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 32 kb)
Rights and permissions
About this article
Cite this article
Pathak, P., Dalmacy, D., Tsilimigras, D.I. et al. Complications After Complex Gastrointestinal Cancer Surgery: Benefits and Costs Associated with Inter-hospital Transfer Among Medicare Beneficiaries. J Gastrointest Surg 25, 1370–1379 (2021). https://doi.org/10.1007/s11605-021-05011-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05011-3