Abstract
Background
Post-acute care (PAC) services can include home healthcare, long-term care hospitals, and skilled nursing facilities. We sought to define factors associated with PAC discharge disposition among Medicare beneficiaries who underwent hepatectomy for hepatocellular carcinoma (HCC).
Methods
Data for Medicare beneficiaries with a diagnosis of HCC and who underwent a hepatectomy between 2004 and 2015 were retrieved from the SEER-Medicare database. Discharge disposition was defined as routine (HSC: discharged to home) or non-routine (SNF/ICF, discharged to skilled nursing/intermediate care facilities, or HHA, discharge to home with home health agency). The Cochran-Mantel-Haenszel test and multivariable logistic regression were used to assess trends in discharge disposition.
Results
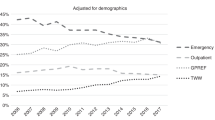
Among 1305 patients, the median patient age at diagnosis was 72 years (IQR: 68–76). Approximately 4 in 5 patients were discharged to HSC (77.4%; n = 1010). The odds of a non-routine discharge decreased by 7.0% annually from 2004 to 2015 (ORtrend, 0.93; 95%CI, 0.89–0.97; ptrend = 0.001). Several factors were associated with non-routine discharge, including patient age (OR 1.06, 95%CI 1.04–1.09) and longer LOS (OR 1.07, 95%CI 1.05–1.10). In contrast, patients who had a minor hepatectomy (OR 0.69, 95%CI 0.52–0.93) at a teaching hospital (OR 0.63, 95%CI 0.45–0.89) had lower odds of a non-routine discharge (all P < 0.05). HSC discharge increased over time (2004–2007 (n = 205, 68.1%) vs. 2008–2011 (n = 330, 77.8%) vs. 2012–2015 (n = 475, 81.9%); ptrend < 0.001). Over the same time period, there was a decreasing trend in 90-day readmission (2004–2007 (n = 91, 30.2%) vs. 2008–2011 (n = 107, 25.2%) vs. 2012–2015 (n = 129, 22.2%); ptrend = 0.03).
Conclusion
Utilization of PAC services following hepatic resection of HCC decreased by 57.0% between 2004 and 2015. These data highlight that decreased PAC utilization was not generally associated with higher readmission rates following resection of HCC.


Similar content being viewed by others
References
Paredes AZ, Hyer JM, Tsilimigras DI, Bagante F, Beal EW, Merath K et al. Predictors and outcomes of nonroutine discharge after hepatopancreatic surgery. Surgery. 2019; 165(6):1128-35.
Shah BC, Ullrich F, Smith L, Leiphrakpam P, Ly Q, Sasson A et al. National trends in discharge disposition after hepatic resection for malignancy. HPB (Oxford) 2011; 13(2):96-102.
Tsilimigras DI, Sahara K, Moris D, Mehta R, Paredes AZ, Ratti F et al. Assessing Textbook Outcomes Following Liver Surgery for Primary Liver Cancer Over a 12-Year Time Period at Major Hepatobiliary Centers. Ann Surg Oncol 2020; 27(9):3318-27.
Merath K, Chen Q, Bagante F, Beal E, Akgul O, Dillhoff M et al. Textbook Outcomes Among Medicare Patients Undergoing Hepatopancreatic Surgery. Ann Surg 2020; 271(6):1116-23.
Idrees JJ, Johnston FM, Canner JK, Dillhoff M, Schmidt C, Haut ER et al. Cost of Major Complications After Liver Resection in the United States: Are High-volume Centers Cost-effective? Ann Surg 2019; 269(3):503-10.
Idrees JJ, Kimbrough CW, Rosinski BF, Schmidt C, Dillhoff ME, Beal EW et al. The Cost of Failure: Assessing the Cost-Effectiveness of Rescuing Patients from Major Complications After Liver Resection Using the National Inpatient Sample. J Gastrointest Surg 2018; 22(10):1688-96.
Spolverato G, Ejaz A, Kim Y, Weiss M, Wolfgang CL, Hirose K et al. Readmission incidence and associated factors after a hepatic resection at a major hepato-pancreatico-biliary academic centre. HPB 2014; 16(11):972-8.
Kane RL. Finding the Right Level of Posthospital Care: “We Didn't Realize There Was Any Other Option for Him”. JAMA. 2011; 305(3):284-93.
Chen LM, Norton EC, Banerjee M, Regenbogen SE, Cain-Nielsen AH, Birkmeyer JD. Spending On Care After Surgery Driven By Choice Of Care Settings Instead Of Intensity Of Services. Health Aff (Millwood) 2017; 36(1):83-90.
Jarman B, Aylin P, Bottle A. Discharge destination and length of stay: differences between US and English hospitals for people aged 65 and over. BMJ. 2004; 328(7440):605-.
Werner RM, Konetzka RT. Trends in Post-Acute Care Use Among Medicare Beneficiaries: 2000 to 2015. JAMA. 2018; 319(15):1616-7.
McWilliams JM, Gilstrap LG, Stevenson DG, Chernew ME, Huskamp HA, Grabowski DC. Changes in Postacute Care in the Medicare Shared Savings Program. JAMA Intern Med 2017; 177(4):518-26.
Diaz A, Nuliyalu U, Dimick JB, Nathan H. Variation in Surgical Spending Among the Highest Quality Hospitals for Cancer Surgery. Ann Surg. 2020.
Balentine CJ, Leverson G, Vanness DJ, Knight S, Turan J, Brown CJ et al. Selecting post-acute care settings after abdominal surgery: Are we getting it right? Am J Surg 2018; 216(2):260-6.
Paredes AZ, Hyer JM, Tsilimigras DI, Merath K, Mehta R, Sahara K et al. Skilled nursing facility (SNF) utilization and impact of SNF star-quality ratings on outcomes following hepatectomy among Medicare beneficiaries. HPB (Oxford) 2020; 22(1):109-15.
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002; 40(8 Suppl):IV-3-18.
Nathan H, Pawlik TM. Limitations of Claims and Registry Data in Surgical Oncology Research. Ann Surg Oncol 2008; 15(2):415-23.
Paredes AZ, Hyer JM, Tsilimigras DI, Palmer E, Lustberg MB, Dillhoff ME et al. Association of pre-existing mental illness with all-cause and cancer-specific mortality among Medicare beneficiaries with pancreatic cancer. HPB. 2020.
Iezzoni LI, Daley J, Heeren T, Foley SM, Fisher ES, Duncan C et al. Identifying complications of care using administrative data. Med Care 1994; 32(7):700-15.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P et al. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am J Epidemiol 2011; 173(6):676-82.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43(11):1130-9.
Diaz A, Barmash E, Azap R, Paredes AZ, Hyer JM, Pawlik TM. Association of County-Level Social Vulnerability with Elective Versus Non-elective Colorectal Surgery. J Gastrointest Surg. 2020.
Azap RA, Paredes AZ, Diaz A, Hyer JM, Pawlik TM. The association of neighborhood social vulnerability with surgical textbook outcomes among patients undergoing hepatopancreatic surgery. Surgery. 2020; 168(5):868-75.
Parkin DM, Bray F, Ferlay J, Pisani P. Global Cancer Statistics, 2002. CA Cancer J Clin 2005; 55(2):74-108.
Grandhi MS, Kim AK, Ronnekleiv-Kelly SM, Kamel IR, Ghasebeh MA, Pawlik TM. Hepatocellular carcinoma: From diagnosis to treatment. Surg Oncol 2016; 25(2):74-85.
Bugianesi E. Non-alcoholic Steatohepatitis and Cancer. Clin Liver Dis 2007; 11(1):191-207.
Nomura F, Ohnishi K, Honda M, Satomura Y, Nakai T, Okuda K. Clinical features of hepatocellular carcinoma in the elderly: a study of 91 patients older than 70 years. Br J Cancer 1994; 70(4):690-3.
Mirici-Cappa F, Gramenzi A, Santi V, Zambruni A, Di Micoli A, Frigerio M et al. Treatments for hepatocellular carcinoma in elderly patients are as effective as in younger patients: a 20-year multicentre experience. Gut. 2010; 59(3):387-96.
Michielsen PP, Francque SM, van Dongen JL. Viral hepatitis and hepatocellular carcinoma. World J Surg Oncol 2005; 3(1):27.
Nathan H, Segev DL, Mayo SC, Choti MA, Cameron AM, Wolfgang CL et al. National trends in surgical procedures for hepatocellular carcinoma: 1998-2008. Cancer. 2012; 118(7):1838-44.
Cloyd JM, Mizuno T, Kawaguchi Y, Lillemoe HA, Karagkounis G, Omichi K et al. Comprehensive Complication Index Validates Improved Outcomes Over Time Despite Increased Complexity in 3707 Consecutive Hepatectomies. Ann Surg 2020; 271(4):724-31.
Vitale A, Spolverato G, Bagante F, Gani F, Popescu I, Marques HP et al. A multi-institutional analysis of elderly patients undergoing a liver resection for intrahepatic cholangiocarcinoma. J Surg Oncol 2016; 113(4):420-6.
Wagner D, Büttner S, Kim Y, Gani F, Xu L, Margonis GA et al. Clinical and morphometric parameters of frailty for prediction of mortality following hepatopancreaticobiliary surgery in the elderly. BJS (Br J Surg) 2016; 103(2):e83-e92.
Adam R, Frilling A, Elias D, Laurent C, Ramos E, Capussotti L et al. Liver resection of colorectal metastases in elderly patients. BJS (Br J Surg) 2010; 97(3):366-76.
Chen Q, Merath K, Olsen G, Bagante F, Idrees JJ, Akgul O et al. Impact of Post-Discharge Disposition on Risk and Causes of Readmission Following Liver and Pancreas Surgery. J Gastrointest Surg 2018; 22(7):1221-9.
Hyer JM, Paredes AZ, Cerullo M, Tsilimigras DI, White S, Ejaz A et al. Assessing post-discharge costs of hepatopancreatic surgery: an evaluation of Medicare expenditure. Surgery. 2020; 167(6):978-84.
Diaz A, Chhabra KR, Dimick JB, Nathan H. Variations in surgical spending within hospital systems for complex cancer surgery. Cancer. 2020.
Ackerly DC, Grabowski DC. Post-acute care reform--beyond the ACA. N Engl J Med 2014; 370(8):689-91.
Tsai TC, Joynt KE, Wild RC, Orav EJ, Jha AK. Medicare's Bundled Payment initiative: most hospitals are focused on a few high-volume conditions. Health Aff (Millwood) 2015; 34(3):371-80.
Rolnick JA, Liao JM, Emanuel EJ, Huang Q, Ma X, Shan EZ et al. Spending and quality after three years of Medicare's bundled payments for medical conditions: quasi-experimental difference-in-differences study. BMJ. 2020; 369:m1780.
Navathe AS, Troxel AB, Liao JM, Nan N, Zhu J, Zhong W et al. Cost of Joint Replacement Using Bundled Payment Models. JAMA Intern Med 2017; 177(2):214-22.
Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Post-Acute Care After Joint Replacement in Medicare's Bundled Payments for Care Improvement Initiative. J Am Geriatr Soc 2019; 67(5):1027-35.
Ethun CG, Bilen MA, Jani AB, Maithel SK, Ogan K, Master VA. Frailty and cancer: Implications for oncology surgery, medical oncology, and radiation oncology. CA Cancer J Clin 2017; 67(5):362-77.
Author information
Authors and Affiliations
Contributions
DMD, JMH, AD, and TMP conceived of and designed this work. DMD and JMH performed data analysis. DMD and JMH drafted the manuscript. JMH, AD, AP, DMD, DIT, and TMP critically revised the manuscript, provided approval of the final version, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Dalmacy, D.M., Hyer, J.M., Diaz, A. et al. Trends in Discharge Disposition Following Hepatectomy for Hepatocellular Carcinoma Among Medicare Beneficiaries. J Gastrointest Surg 25, 2842–2850 (2021). https://doi.org/10.1007/s11605-021-05000-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05000-6