Abstract
Purpose
Assessment of treating metastatic ileal neuroendocrine tumors (NETs) with complete resection of primary tumor, nodal and liver metastases, plus administration of long-acting somatostatin analogues (SSAs).
Methods
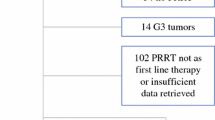
A prospective database was queried for patients with ileal or pancreatic NETs with pathology-confirmed liver metastases and tumor somatostatin receptors. Patients did not have MEN-1 and had no previous treatment. The impacts of SSA treatment on the primary outcome of survival and secondary outcome of progression-free survival were assessed with Kaplan–Meier analysis. Log rank test was used to compare overall and progression-free survival among groups.
Results
Seventeen ileal NET patients and 36 pancreatic NET patients who underwent surgical resection between 2001 and 2018, who had pathology-confirmed liver metastases and confirmed tumor somatostatin receptors, did not have MEN-1, and had no previous treatment were identified. Median follow-up for patients with ileal NETs was 80 months (range 0–197 months) and 32 months (range 1–182 months) for pancreatic NETs. Five-year survival was 93% and 72% for ileal and pancreatic NET, respectively. Progression-free 5-year survival was 70% and 36% for ileal and pancreatic NET, respectively. Overall 5-year survival for pNETs was greater in those patients treated with SSA (79%) compared to those who underwent surgery alone (34%, p < 0.01). The average ECOG score was low for surviving patients with ileal (0.15) and pancreatic NET (0.73) indicating a good quality of life.
Conclusions
Resection of primary lymph node and liver metastatic ileal or pancreatic NETs followed with continued SSAs is associated with an excellent progression-free and overall survival and minimal side effects.




Similar content being viewed by others
References
Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker R V., et al. Gastroenteropancreatic neuroendocrine tumours. The Lancet Oncology. 2008. p. 61–72.
Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934–59.
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, et al. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26(18):3063–72.
Frilling A, Sotiropoulos GC, Li J, Kornasiewicz O, Plöckinger U. Multimodal management of neuroendocrine liver metastases. HPB (Oxford) [Internet]. 2010;12(6):361–79.
Fraenkel M, Kim MK, Faggiano A, Valk GD. Epidemiology of gastroenteropancreatic neuroendocrine tumours. Best Pract Res Clin Gastroenterol. 2012;26(6):691–703.
Ito T, Lee L, Jensenc RT. Carcinoid-syndrome: Recent advances, current status and controversies. Curr Opin Endocrinol Diabetes Obes. 2018;25(1):22–35.
Halperin DM, Shen C, Dasari A, Xu Y, Chu Y, Zhou S, et al. Frequency of carcinoid syndrome at neuroendocrine tumour diagnosis: a population-based study. Lancet Oncol. 2017;18(4):525–34.
Weber HC, Venzon DJ, Lin JT, et al. Determinants of metastatic rate and survival in patients with Zollinger-Ellison syndrome: a prospective long-term study. Gastroenterology 1995;108:1637–49.
Frilling A, Modlin IM, Kidd M, Russell C, Breitenstein S, Salem R, et al. Recommendations for management of patients with neuroendocrine liver metastases. The Lancet Oncology. 2014. p. E8–21.
Mayo SC, De Jong MC, Pulitano C, Clary BM, Reddy SK, Gamblin TC, et al. Surgical management of hepatic neuroendocrine tumor metastasis: Results from an international multi-institutional analysis. Ann Surg Oncol. 2010;17(12):3129–36.
Glazer ES, Tseng JF, Al-Refaie W, Solorzano CC, Liu P, Willborn KA, et al. Long-term survival after surgical management of neuroendocrine hepatic metastases. HPB. 2010;12(6):427–33.
Sarmiento JM, Heywood G, Rubin J, Ilstrup DM, Nagorney DM, Que FG. Surgical treatment of neuroendocrine metastases to the liver: A plea for resection to increase survival. J Am Coll Surg. 2003;197(1):29–37.
Harris AG. Future medical prospects for Sandostatin. Metabolism. 1990;39((9 Suppl 2)):180–5.
Rinke A, Müller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: A report from the PROMID study group. J Clin Oncol. 2009;27(28):4656–63.
Caplin ME, Pavel M, Ćwikła JB, Phan AT, Raderer M, Sedláčková E, et al. Lanreotide in Metastatic Enteropancreatic Neuroendocrine Tumors. N Engl J Med. 2014;371:224–33.
Kos-Kudła B. Treatment of neuroendocrine tumors: New recommendations based on the CLARINET study. Wspolczesna Onkol. 2015;19(5):345–9.
Ahrendt SA, McGuire GE, Pitt HA, Lillemoe KD. Why does somatostatin cause gallstones? Am J Surg. 1991;161(1):177–82.
Norton JA, Warren RS, Kelly MG, Zuraek MB, Jensen RT, Fahey TJ, et al. Aggressive surgery for metastatic liver neuroendocrine tumors. Surgery. 2003. p. 1057–63.
Rindi G, Klöppel G, Alhman H, Caplin M, Couvelard A, De Herder WW, et al. TNM staging of foregut (neuro)endocrine tumors: A consensus proposal including a grading system. Virchows Arch. 2006;449(4):395–401.
Elias D, Lasser P, Ducreux M, Duvillard P, Ouellet JF, Dromain C, et al. Liver resection (and associated extrahepatic resections) for metastatic well-differentiated endocrine tumors: A 15-year single center prospective study. Surgery. 2003;
Sowa-Staszczak A, Pach D, Chrzan R, Trofimiuk M, Stefanska A, Tomaszuk M, et al. Peptide receptor radionuclide therapy as a potential tool for neoadjuvant therapy in patients with inoperable neuroendocrine tumours (NETs). Eur J Nucl Med Mol Imaging. 2011;38(9):1669–74.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 Trial of 177Lu-Dotatate for Midgut Neuroendocrine Tumors. N Engl J Med [Internet]. 2017 Jan 11;376(2):125–35. Available from: https://doi.org/10.1056/NEJMoa1607427
Fiore F, Del Prete M, Franco R, Marotta V, Ramundo V, Marciello F, et al. Transarterial embolization (TAE) is equally effective and slightly safer than transarterial chemoembolization (TACE) to manage liver metastases in neuroendocrine tumors. Endocrine. 2014;47(1):177–182.
Gupta S, Johnson MM, Murthy R, Ahrar K, Wallace MJ, Madoff DC, et al. Hepatic arterial embolization and chemoembolization for the treatment of patients with metastatic neuroendocrine tumors: Variables affecting response rates and survival. Cancer. 2005;104(8):1590–602.
Facciorusso A, Muscatiello N, Serviddio G. Transarterial radioembolization vs chemoembolization for hepatocarcinoma patients: A systematic review and metaanalysis. World J Hepatol. 2016;8(18):770–778.
Yang TX, Chua TC, Morris DL. Radioembolization and chemoembolization for unresectable neuroendocrine liver metastases - A systematic review. Surgical Oncology. 2012. p. 299–308.
Pusceddu S, Verzoni E, Prinzi N, Mennitto A, Femia D, Grassi P, et al. Everolimus treatment for neuroendocrine tumors: Latest results and clinical potential. Therapeutic Advances in Medical Oncology. 2017. p. 183–188.
Yao JC, Fazio N, Singh S, Buzzoni R, Carnaghi C, Wolin E, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): A randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968–77.
Boudreaux JP, Klimstra DS, Hassan MM, Woltering EA, Jensen RT, Goldsmith SJ, et al. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: Well-differentiated neuroendocrine tumors of the jejunum, ileum, appendix, and cecum. Pancreas. 2010. p. 753–66.
Solorzano CC, Lee JE, Pisters PWT, Vauthey JN, Ayers GD, Jean ME, et al. Nonfunctioning islet cell carcinoma of the pancreas: Survival results in a contemporary series of 163 patients. Surgery. 2001;130:1078–85.
Khan MS, Caplin ME. Therapeutic management of patients with gastroenteropancreatic neuroendocrine tumours. Endocr Relat Cancer. 2011;18(S1):S53–S74.
Author information
Authors and Affiliations
Contributions
Dr. Jeffrey Norton surgically treated the participants, devised the research plan, and revised the manuscript.
Andrea Fisher collected data from ileal patient records, performed analysis, developed figures for ileal patients, and drafted the manuscript.
Dr. Ashley Titan performed analysis of patient records, developed figures for pancreatic patients, and revised the manuscript.
Dr. Deshka Foster facilitated data analysis and figure creation for the ileal patients.
Dr. Patrick Worth collected data from pancreatic patient records.
Dr. George Poultsides surgically treated the participants, facilitated with devising the research plan, and revised the manuscript.
Dr. Brendan Visser surgically treated the participants and revised the manuscript.
Dr. Monica Dua surgically treated the participants and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper was presented as a poster at the SSAT meeting, Digestive Disease week, San Diego, CA. May 19, 2019.
Rights and permissions
About this article
Cite this article
Fisher, A.T., Titan, A.L., Foster, D.S. et al. Management of Ileal Neuroendocrine Tumors with Liver Metastases. J Gastrointest Surg 24, 1530–1539 (2020). https://doi.org/10.1007/s11605-019-04309-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04309-7