Abstract
Background
Obesity may impact surgical outcomes of gastrectomy. Whether visceral fat area (VFA) is a better obesity parameter than body mass index (BMI) is still controversial. The aim of this study is to compare the accuracy and effectiveness of VFA and BMI in predicting the short-term surgical outcomes of gastrectomy.
Methods
Patients who were diagnosed with gastric cancer were measured for BMI and VFA preoperatively and then divided into a VFA-H (VFA-high) group and VFA-L (VFA-low) group, at the cutoff point of 100 cm2, and a BMI-H (BMI-high) group and BMI-L (BMI-low) group, at the cutoff point of 25 kg/m2. The short-term surgical outcomes were compared between the different groups.
Results
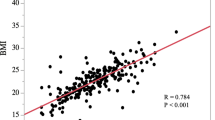
In total, 276 patients were enrolled in this study; 55 (19.9%) patients were classified into the BMI-H group, and 122 (44.2%) patients were classified into the VFA-H group. There was a significant correlation between BMI and VFA (r = 0.652, p < 0.001). Compared with the VFA-L group, the VFA-H group had a higher incidence of postoperative complications (31.1% vs. 13.0%; p < 0.001), longer operation duration (270.0 (235.0–305.0) vs. 255.0 (223.8–295.0), p = 0.046), and more blood loss (100.0 (100.0–150.0) vs. 80.0 (80.0–100.0), p < 0.001), while the BMI-H group had more blood loss than the BMI-L group (100.0 (100.0–120.0) vs. 100.0(80.0–100.0), p = 0.006). Logistic regression showed that VFA was an independent risk factor for postoperative complications (odds ratio 2.813, 95% CI 1.523–5.194; p = 0.001).
Conclusion
For gastric cancer patients, VFA is superior to BMI in accurately and effectively illuminating the impact of obesity on short-term surgical outcomes.
Trial Registration
Clinicaltrials.gov: NCT02800005.


Similar content being viewed by others
References
Van Cutsem, E., X. Sagaert, B. Topal, et al., Gastric cancer. Lancet, 2016. 388(10060): p. 2654–2664.
Chen, W., R. Zheng, P.D. Baade, et al., Cancer statistics in China, 2015. CA Cancer J Clin, 2016. 66(2): p. 115–32.
Torre, L.A., F. Bray, R.L. Siegel, et al., Global cancer statistics, 2012. CA Cancer J Clin, 2015. 65(2): p. 87–108.
Songun, I., H. Putter, E.M. Kranenbarg, et al., Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol, 2010. 11(5): p. 439–49.
Degiuli, M., M. Sasako, A. Ponti, et al., Survival results of a multicentre phase II study to evaluate D2 gastrectomy for gastric cancer. Br J Cancer, 2004. 90(9): p. 1727–32.
Sasako, M., T. Sano, S. Yamamoto, et al., D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med, 2008. 359(5): p. 453–62.
Perez Rodrigo, C., Current mapping of obesity. Nutr Hosp, 2013. 28 Suppl 5: p. 21–31.
Ogden, C.L., M.D. Carroll, B.K. Kit, et al., Prevalence of childhood and adult obesity in the United States, 2011-2012. Jama, 2014. 311(8): p. 806–14.
The Chinese National Health and Family Planning Commission. The Nutrition and Health Status of the Chinese People (2015 Report). Available at http://mp.weixin.qq.com/s?__biz=MjM5OTIyODc1NA==&mid=205782183&idx=1&sn=12d59495ff4866ffa0d92023e4efc40e&scene=1#rd (accessed on 23 July, 2016). 401(6): p. 823–8.
Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. The Lancet, 2016. 387(10026): p. 1377–1396.
Kim, J.H., H.M. Chin, S.S. Hwang, et al., Impact of intra-abdominal fat on surgical outcome and overall survival of patients with gastric cancer. Int J Surg, 2014. 12(4): p. 346–52.
Sugisawa, N., M. Tokunaga, Y. Tanizawa, et al., Intra-abdominal infectious complications following gastrectomy in patients with excessive visceral fat. Gastric Cancer, 2012. 15(2): p. 206–12.
Takeuchi, M., K. Ishii, H. Seki, et al., Excessive visceral fat area as a risk factor for early postoperative complications of total gastrectomy for gastric cancer: a retrospective cohort study. BMC Surg, 2016. 16(1): p. 54.
Yoshikawa, K., M. Shimada, N. Kurita, et al., Visceral fat area is superior to body mass index as a predictive factor for risk with laparoscopy-assisted gastrectomy for gastric cancer. Surg Endosc, 2011. 25(12): p. 3825–30.
Watanabe, J., K. Tatsumi, M. Ota, et al., The impact of visceral obesity on surgical outcomes of laparoscopic surgery for colon cancer. Int J Colorectal Dis, 2014. 29(3): p. 343–51.
Go, J.E., M.C. Kim, K.H. Kim, et al., Effect of visceral fat area on outcomes of laparoscopyassisted distal gastrectomy for gastric cancer: subgroup analysis by gender and parameters of obesity. Ann Surg Treat Res, 2015. 88(6): p. 318–24.
Effect of Obesity on Surgical Outcomes and Survival for Gastric Cancer;https://clinicaltrials.gov/ct2/show/NCT02800005?cond=gastric+cancer&cntry=CN&city=Chengdu&rank=2. 10 Jul 2018
Clark, W., E.M. Siegel, Y.A. Chen, et al., Quantitative measures of visceral adiposity and body mass index in predicting rectal cancer outcomes after neoadjuvant chemoradiation. J Am Coll Surg, 2013. 216(6): p. 1070–81.
New criteria for 'obesity disease' in Japan. Circ J, 2002. 66(11): p. 987–92.
The Asia Pacific Perspective: Redefining Obesity and its Treatment. Melbourne [Internet], International Diabetes Institute, 2000.
Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer, 2017. 20(1): p. 1–19.
Dindo, D., N. Demartines, and P.A. Clavien, Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg, 2004. 240(2): p. 205–13.
Karastergiou, K., The Interplay Between Sex, Ethnicity, and Adipose Tissue Characteristics. Curr Obes Rep, 2015. 4(2): p. 269–78.
Bouchi, R., T. Takeuchi, M. Akihisa, et al., High visceral fat with low subcutaneous fat accumulation as a determinant of atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol, 2015. 14: p. 136.
S, G., M. D, R. D, et al., International consensus on a complications list after gastrectomy for cancer.%A Baiocchi GL. Gastric cancer : official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association, 2018. undefined(undefined): p. undefined.
Ajani, J.A., T.A. D'Amico, K. Almhanna, et al., Gastric Cancer, Version 3.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw, 2016. 14(10): p. 1286–1312.
Yang, K., Y.Y. Choi, W.H. Zhang, et al., Strategies to improve treatment outcome in gastric cancer: a retrospective analysis of patients from two high-volume hospitals in Korea and China. Oncotarget, 2016. 7(28): p. 44660–44675.
HJ, L., H. WJ, Y. HK, et al., Short-term Outcomes of a Multicenter Randomized Controlled Trial Comparing Laparoscopic Distal Gastrectomy With D2 Lymphadenectomy to Open Distal Gastrectomy for Locally Advanced Gastric Cancer (KLASS-02-RCT). Annals of surgery, 2019. undefined(undefined): p. undefined.
Kim W, K.H., Han SU, et al; Korean Laparo―endoscopic and G.S.S.K. Group., Decreased Morbidity of Laparoscopic Distal Gastrectomy Compared With Open Distal Gastrectomy for Stage I Gastric Cancer: Short-term Outcomes From a Multicenter Randomized Controlled Trial (KLASS―01)[J]. Ann Surg 2016. 263(1):28―35. https://doi.org/10.1097/SLA.0000000000001346.
Sano, T., M. Sasako, S. Yamamoto, et al., Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol, 2004. 22(14): p. 2767–73.
Sasako, M., T. Sano, S. Yamamoto, et al., Left thoracoabdominal approach versus abdominal-transhiatal approach for gastric cancer of the cardia or subcardia: a randomised controlled trial. Lancet Oncol, 2006. 7(8): p. 644–51.
Katai, H., J. Mizusawa, H. Katayama, et al., Short-term surgical outcomes from a phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric cancer: Japan Clinical Oncology Group Study JCOG0912. Gastric Cancer, 2017. 20(4): p. 699–708.
Kataoka, K., H. Katai, J. Mizusawa, et al., Non-Randomized Confirmatory Trial of Laparoscopy-Assisted Total Gastrectomy and Proximal Gastrectomy with Nodal Dissection for Clinical Stage I Gastric Cancer: Japan Clinical Oncology Group Study JCOG1401. J Gastric Cancer, 2016. 16(2): p. 93–7.
Hu, Y., C. Huang, Y. Sun, et al., Morbidity and Mortality of Laparoscopic Versus Open D2 Distal Gastrectomy for Advanced Gastric Cancer: A Randomized Controlled Trial. J Clin Oncol, 2016. 34(12): p. 1350–7.
Hur, H., H.Y. Lee, H.J. Lee, et al., Efficacy of laparoscopic subtotal gastrectomy with D2 lymphadenectomy for locally advanced gastric cancer: the protocol of the KLASS-02 multicenter randomized controlled clinical trial. BMC Cancer, 2015. 15: p. 355.
Acknowledgments
The authors thank the valuable work of the Volunteer Team of Gastric Cancer Surgery (VOLTGA) West China Hospital, Sichuan University, China, for the establishment and updating of the gastric cancer database.
Funding
This study is supported by grants of National Natural Science Foundation of China, No.81301866; Sichuan Province Youth Science Technology Innovative Research Team, No.2015TD0009; 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZY2017304); Fund for Fostering Academic and Technical Leaders of Sichuan Province, No. [2017]919; and Foundation of Science & Technology Department of Sichuan Province (No. 2018SZ0147).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Supplementary Table 1
(DOCX 16 kb)
Supplementary Table 2
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Yang, Sj., Li, Hr., Zhang, Wh. et al. Visceral Fat Area (VFA) Superior to BMI for Predicting Postoperative Complications After Radical Gastrectomy: a Prospective Cohort Study. J Gastrointest Surg 24, 1298–1306 (2020). https://doi.org/10.1007/s11605-019-04259-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04259-0