Abstract
Aim
The aim of this study is to compare the effects of extended lymphadenectomy (E-LD) and regional lymphadenectomy (R-LD) on outcome after radical resection of hilar cholangiocarcinoma (HCCA).
Methods
Data of 290 patients who underwent radical resection of HCCA were retrospectively analyzed. Demographic characteristics, surgical variables, and tumor and LN characteristics were evaluated for association with survival.
Results
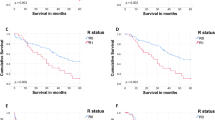
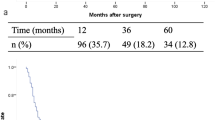
A total of 63 patients underwent E-LD. Patients who underwent E-LD were more likely to have portal vein embolization (14.3% vs. 5.7%), radical hepatectomy (36.2% vs. 26.0%), higher proportion of M1 patients (22.2% vs. 5.3%), more lymph nodes (LNs) retrieved (17 vs. 7), and positive common hepatic artery lymph nodes (21.4% vs. 12.6%) when compared with R-LD (all P < 0.05). The Kaplan–Meier curve of overall survival for patients who underwent E-LD indicated improvement over patients who underwent R-LD in M0 (33.39 vs. 21.31 months; P = 0.032) and R0 resection (32.97 vs. 21.02 months; P = 0.044) disease, but not observed in M1 disease (P > 0.05). After propensity score matching, E-LD was not associated with a significant improvement in overall survival (OS) even in all subgroup analysis (all P > 0.05). On multivariable analysis, E-LD was associated with improved overall survival, but not after propensity score matching.
Conclusion
E-LD is more likely to be performed in higher stage tumors. E-LD significantly increases LN retrieval, thereby preventing under-staging and improving survival prediction. E-LD should not be adopted for HCCA patients with intraoperatively confirmed distant LN metastases. Future studies are required to further assess whether E-LD should be performed in negative celiac, superior mesenteric, and para-aortic lymph node in HCCA patients.


Similar content being viewed by others
References
Giuliante F, Ardito F, Guglielmi A, Aldrighetti L, Ferrero A, Calise F et al. Association of Lymph Node Status With Survival in Patients After Liver Resection for Hilar Cholangiocarcinoma in an Italian Multicenter Analysis. JAMA Surgery. 2016;151(10):916–22. doi: https://doi.org/10.1001/jamasurg.2016.1769.
Conci S, Ruzzenente A, Sandri M, Bertuzzo F, Campagnaro T, Bagante F et al. What is the most accurate lymph node staging method for perihilar cholangiocarcinoma? Comparison of UICC/AJCC pN stage, number of metastatic lymph nodes, lymph node ratio, and log odds of metastatic lymph nodes. European Journal of Surgical Oncology (EJSO). 2017;43(4):743–50. doi:https://doi.org/10.1016/j.ejso.2016.12.007.
Mao K, Liu J, Sun J, Zhang J, Chen J, Pawlik TM et al. Patterns and prognostic value of lymph node dissection for resected perihilar cholangiocarcinoma. J Gastroenterol Hepatol. 2016;31(2):417–26. doi:https://doi.org/10.1111/jgh.13072.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Hepatobiliary Cancers, V.2.2018. Available at http://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf. 2018. Accessed 30 Sep 2018
Miyazaki M, Yoshitomi H, Miyakawa S, Uesaka K, Unno M, Endo I et al. Clinical practice guidelines for the management of biliary tract cancers 2015: the 2nd English edition. Journal of Hepato-Biliary-Pancreatic Sciences. 2015;22(4):249–73. doi:https://doi.org/10.1002/jhbp.233.
Kitagawa Y, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H et al. Lymph Node Metastasis from Hilar Cholangiocarcinoma: Audit of 110 Patients Who Underwent Regional and Paraaortic Node Dissection. Annals of Surgery. 2001;233(3):385–92.
Murakami Y, Uemura K, Sudo T, Hashimoto Y, Nakashima A, Kondo N et al. Is Para-aortic Lymph Node Metastasis a Contraindication for Radical Resection in Biliary Carcinoma? World Journal of Surgery. 2011;35(5):1085–93. doi:https://doi.org/10.1007/s00268-011-1036-4.
Aoba T, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y et al. Assessment of Nodal Status for Perihilar Cholangiocarcinoma: Location, Number, or Ratio of Involved Nodes. Annals of Surgery. 2013;257(4):718–25. doi:https://doi.org/10.1097/SLA.0b013e3182822277.
Schwarz RE, Smith DD. Lymph Node Dissection Impact on Staging and Survival of Extrahepatic Cholangiocarcinomas, Based on U.S. Population Data. Journal of Gastrointestinal Surgery. 2007;11(2):158. doi:https://doi.org/10.1007/s11605-006-0018-6.
Mantel HTJ, Wiggers JK, Verheij J, Doff JJ, Sieders E, van Gulik TM et al. Lymph Node Micrometastases are Associated with Worse Survival in Patients with Otherwise Node-Negative Hilar Cholangiocarcinoma. Annals of Surgical Oncology. 2015;22(3):1107–15. doi:https://doi.org/10.1245/s10434-015-4723-9.
Guglielmi A, Ruzzenente A, Campagnaro T, Valdegamberi A, Bagante F, Bertuzzo F et al. Patterns and Prognostic Significance of Lymph Node Dissection for Surgical Treatment of Perihilar and Intrahepatic Cholangiocarcinoma. Journal of Gastrointestinal Surgery. 2013;17(11):1917–28. doi:https://doi.org/10.1007/s11605-013-2331-1.
Xiang S, Lau WY, Chen XP. Hilar cholangiocarcinoma: controversies on the extent of surgical resection aiming at cure. Int J Colorectal Dis. 2015;30(2):159–71. doi:https://doi.org/10.1007/s00384-014-2063-z.
Xiong J, Nunes QM, Huang W, Wei A, Ke N, Mai G et al. Major hepatectomy in Bismuth types I and II hilar cholangiocarcinoma. Journal of Surgical Research. 2015;194(1):194–201. doi:https://doi.org/10.1016/j.jss.2014.10.029.
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK et al. American Joint Committee on Cancer (AJCC) Cancer Staging Manual. 8th ed. New York: Springer; 2017.
Oguro S, Esaki M, Kishi Y, Nara S, Shimada K, Ojima H et al. Optimal indications for additional resection of the invasive cancer-positive proximal bile duct margin in cases of advanced perihilar cholangiocarcinoma. Annals of Surgical Oncology. 2015;22(6):1915–24. doi:https://doi.org/10.1245/s10434-014-4232-2.
Ito M, Mishima Y, Sato T. An anatomical study of the lymphatic drainage of the gallbladder. Surgical and radiologic anatomy : SRA. 1991;13(2):89–104.
Shirai Y, Yoshida K, Tsukada K, Ohtani T, Muto T. Identification of the regional lymphatic system of the gallbladder by vital staining. British Journal of Surgery. 1992;79(7):659–62. doi:https://doi.org/10.1002/bjs.1800790721.
Sato T, Ito M, Sakamoto H. Pictorial dissection review of the lymphatic pathways from the gallbladder to the abdominal para-aortic lymph nodes and their relationships to the surrounding structures. Surgical and Radiologic Anatomy. 2013;35(7):615–21. doi:https://doi.org/10.1007/s00276-013-1088-2.
Kayahara M, Nagakawa T, Ohta T, Kitagawa H, Tajima H, Miwa K. Role of Nodal Involvement and the Periductal Soft-Tissue Margin in Middle and Distal Bile Duct Cancer. Annals of Surgery. 1999;229(1):76–83.
Bagante F, Tran T, Spolverato G, Ruzzenente A, Buttner S, Ethun CG et al. Perihilar Cholangiocarcinoma: Number of Nodes Examined and Optimal Lymph Node Prognostic Scheme. Journal of the American College of Surgeons. 2016;222(5):750–9.e2. doi:https://doi.org/10.1016/j.jamcollsurg.2016.02.012.
Guglielmi A, Ruzzenente A, Campagnaro T, Pachera S, Conci S, Valdegamberi A et al. Prognostic significance of lymph node ratio after resection of peri-hilar cholangiocarcinoma. HPB. 2010;13(4):240–5. doi:https://doi.org/10.1111/j.1477-2574.2010.00277.x.
Ito K, Ito H, Allen PJ, Gonen M, Klimstra D, D’Angelica MI et al. Adequate lymph node assessment for extrahepatic bile duct adenocarcinoma. Annals of Surgery. 2010;251(4):675–81. doi: https://doi.org/10.1097/SLA.0b013e3181d3d2b2.
Hakeem AR, Marangoni G, Chapman SJ, Young RS, Nair A, Hidalgo EL et al. Does the extent of lymphadenectomy, number of lymph nodes, positive lymph node ratio and neutrophil-lymphocyte ratio impact surgical outcome of perihilar cholangiocarcinoma? Eur J Gastroenterol Hepatol. 2014;26(9):1047–54. doi:https://doi.org/10.1097/meg.0000000000000162.
Kambakamba P, Linecker M, Slankamenac K, DeOliveira ML. Lymph node dissection in resectable perihilar cholangiocarcinoma: a systematic review. The American Journal of Surgery. 2015;210(4):694–701. doi:https://doi.org/10.1016/j.amjsurg.2015.05.015.
Tojima Y, Nagino M, Ebata T, Uesaka K, Kamiya J, Nimura Y. Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with otherwise node-negative hilar cholangiocarcinoma. Annals of Surgery. 2003;237(2):201–7. doi:https://doi.org/10.1097/01.Sla.0000048446.18118.Fc.
Krasnick BA, Jin LX, Davidson JT, Sanford DE, Ethun CG, Pawlik TM et al. Adjuvant therapy is associated with improved survival after curative resection for hilar cholangiocarcinoma: A multi-institution analysis from the U.S. extrahepatic biliary malignancy consortium. Journal of Surgical Oncology. 2018;117(3):363–71. doi:https://doi.org/10.1002/jso.24836.
Funding
We acknowledge the Sichuan Science and Technology Program (2018JY0019) and Wu Jieping Medical Foundation for Clinical Research (No. 320.2710.1825).
Author information
Authors and Affiliations
Contributions
Wen-jie Ma performed the majority of the manuscript; Zheng-Ru Wu, Hai-Jie Hu, Jun-Ke Wang, and Chang-Hao Yin provided the collection of all the materials and were also involved in editing the manuscript; Nan-Sheng Cheng, Yu-Jun Shi, and Fu-Yu Li revised the manuscript critically and gave the final approval of the version to be published.
Corresponding authors
Ethics declarations
The study was approved by the institutional review committee of West China Hospital, Sichuan University.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Foundation item: Sichuan Science and Technology Program (2018JY0019)
Rights and permissions
About this article
Cite this article
Ma, WJ., Wu, ZR., Hu, HJ. et al. Extended Lymphadenectomy Versus Regional Lymphadenectomy in Resectable Hilar Cholangiocarcinoma. J Gastrointest Surg 24, 1619–1629 (2020). https://doi.org/10.1007/s11605-019-04244-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04244-7