Abstract
Background
The neutrophil to lymphocyte ratio (NLR) is a marker of inflammation and is associated with poor outcomes. We aimed to evaluate the role of the pretreatment NLR in predicting the outcomes after preoperative chemotherapy in patients with colorectal liver metastases (CRLM).
Methods
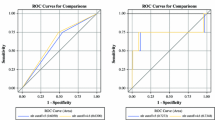
A retrospective review was performed for 183 patients with CRLM. The NLR was measured before chemotherapy, and a receiver operating characteristic (ROC) curve was used to estimate the cutoff value. Logistic regressions were applied to analyze potential predictors of the pathological response. The Cox proportional hazard method was used to analyze survival.
Results
The pre-chemotherapy NLR was 2.4 ± 1.1, whereas the post-chemotherapy NLR was 2.1 ± 1.6 (p < 0.001). The pretreatment NLR of 2.3 was a significant predictive marker for the pathological response. The pathological response rates were 67.1% in the patients with an NLR ≤ 2.3 and 48.1% in patients with an NLR > 2.3 (p = 0.01). Multivariate analysis revealed that the factors independently associated with pathological responses were a low pretreatment NLR (p = 0.043), radiological response to chemotherapy (p < 0.001), first-line chemotherapy (p = 0.001), and targeted therapy (p = 0.002). The median overall survival (OS) and recurrence-free survival (RFS) were worse in the increased NLR cohort than in the low NLR cohort (OS: 31.1 vs. 43.1 months, p = 0.012; RFS: 6.5 vs. 9.4 months, p = 0.06). According to multivariate analyses, a high pretreatment NLR was a significant predictor for both worse OS (HR = 2.43, 95%CI = 1.49–3.94, p < 0.001) and RFS (HR = 1.53, 95%CI = 1.08–2.18, p = 0.017).
Conclusions
An increased pretreatment NLR was a significant predictor of a poor pathological response and worse prognosis after preoperative chemotherapy. The NLR is a simple biomarker for assessing chemotherapy efficacy.


Similar content being viewed by others
References
Van Cutsem E, Nordlinger B, Adam R, et al. Towards a pan-European consensus on the treatment of patients with colorectal liver metastases. Eur J Cancer. 2006;42 (22):12–2221.
Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27(22):3677–83.
Cucchetti A, Ferrero A, Cescon M, et al. Cure model survival analysis after hepatic resection for colorectal liver metastases. Ann Surg Oncol. 2015;22 (6):1908–1914.
Nordlinger B, Sorbye H, Glimelius B, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371(9617):1007.
Rubbia-Brandt L, Giostra E, Brezault C, et al. Importance of histological tumor response assessment in predicting the outcome in patients with colorectal liver metastases treated with neo-adjuvant chemotherapy followed by liver surgery. Ann Oncol. 2007;18(2):299–304.
Stremitzer S, Stift J, Singh J, et al. Histological response, pattern of tumor destruction and clinical outcome after neoadjuvant chemotherapy including bevacizumab or cetuximab in patients undergoing liver resection for colorectal liver metastases. Eur J Surg Oncol. 2015;41(7):868–74.
Kishi Y, Zorzi D, Contreras C M, et al. Extended Preoperative Chemotherapy Does Not Improve Pathologic Response and Increases Postoperative Liver Insufficiency After Hepatic Resection for Colorectal Liver Metastases. Ann Surg Oncol. 2010;17(11):2870–2876.
Blazer DG 3rd, Kishi Y, Maru DM, et al. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol. 2008; 26(33):5344–5351.
Carrasco J, Gizzi M, Pairet G, et al. Pathological responses after angiogenesis or EGFR inhibitors in metastatic colorectal cancer depend on the chemotherapy backbone. Br J Cancer. 2015; 113(9):1298–304.
Vigano L, Capussotti L, De Rosa G, et al. Liver resection for colorectal metastases after chemotherapy: impact of chemotherapy-related liver injuries, pathological tumor response, and micrometastases on long-term survival. Ann Surg. 2013;258(5):731–740..
Zheng J, Seier K, Gonen M, et al. Utility of Serum Inflammatory Markers for Predicting Microvascular Invasion and Survival for Patients with Hepatocellular Carcinoma. Ann Surg Oncol. 2017;24(12):3706–3714.
Yoh T, Seo S, Hatano E, et al. A Novel Biomarker-Based Preoperative Prognostic Grading System for Predicting Survival After Surgery for Intrahepatic Cholangiocarcinoma. Ann Surg Oncol. 2017;24(5):1351–1357.
Proctor MJ, Morrison DS, Talwar D, et al. A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer. 2011;47(17):2633–41.
Neofytou K, Smyth EC, Giakoustidis A, Khan AZ, Cunningham D, Mudan S. Elevated platelet to lymphocyte ratio predicts poor prognosis after hepatectomy for liver-only colorectal metastases, and it is superior to neutrophil to lymphocyte ratio as an adverse prognostic factor. Med Oncol. 2014;31(10):239.
Kishi Y, Kopetz S, Chun YS, Palavecino M, Abdalla EK, Vauthey JN. Blood neutrophil-to-lymphocyte ratio predicts survival in patients with colorectal liver metastases treated with systemic chemotherapy. Ann Surg Oncol. 2009;16(3):614–22.
Halazun KJ, Aldoori A, Malik HZ, et al. Elevated preoperative neutrophil to lymphocyte ratio predicts survival following hepatic resection for colorectal liver metastases. Eur J Surg Oncol. 2008;34(1):55–60.
Malik HZ, Prasad KR, Halazun KJ, et al. Preoperative prognostic score for predicting survival after hepatic resection for colorectal liver metastases.Ann Surg. 2007;246(5):806–14.
Neal CP, Cairns V, Jones MJ, et al. Prognostic performance of inflammation-based prognostic indices in patients with resectable colorectal liver metastases. Med Oncol. 2015;32(5):144.
Giakoustidis A, Neofytou K, Khan AZ, Mudan S. Neutrophil to lymphocyte ratio predicts pattern of recurrence in patients undergoing liver resection for colorectal liver metastasis and thus the overall survival. J Surg Oncol. 2015;111(4):445–50.
Chua W, Charles KA, Baracos VE, Clarke SJ. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer. 2011;104(8):1288–95.
Kim IH, Lee JE, Yang JH, Jeong JW, Ro S, Lee MA. Clinical significance of changes in systemic inflammatory markers and carcinoembryonic antigen levels in predicting metastatic colorectal cancer prognosis and chemotherapy response. Asia Pac J Clin Oncol. 2017.
Mao R, Zhao JJ, Bi XY, et al. Interaction of margin status and tumour burden determines survival after resection of colorectal liver metastases: A retrospective cohort study. Int J Surg. 2017.
Asano Y, Kashiwagi S, Onoda N, et al. Predictive Value of Neutrophil/Lymphocyte Ratio for Efficacy of Preoperative Chemotherapy in Triple-Negative Breast Cancer. Ann Surg Oncol. 2016;23(4):1104–10.
Chen Y, Chen K, Xiao X, et al. Pretreatment neutrophil-to-lymphocyte ratio is correlated with response to neoadjuvant chemotherapy as an independent prognostic indicator in breast cancer patients: a retrospective study. BMC Cancer. 2016;16:320.
Sato H, Tsubosa Y, Kawano T. Correlation between the pretherapeutic neutrophil to lymphocyte ratio and the pathologic response to neoadjuvant chemotherapy in patients with advanced esophageal cancer. World J Surg. 2012;36(3):617–22.
Buisan O, Orsola A, Areal J, et al. Low Pretreatment Neutrophil-to-Lymphocyte Ratio Predicts for Good Outcomes in Patients Receiving Neoadjuvant Chemotherapy Before Radical Cystectomy for Muscle Invasive Bladder Cancer. Clin Genitourin Cancer. 2017;15(1):145–151.
Hasegawa S, Eguchi H, Tomokuni A, et al. Pre-treatment neutrophil to lymphocyte ratio as a predictive marker for pathological response to preoperative chemoradiotherapy in pancreatic cancer. Oncol Lett. 2016;11(2):1560–1566.
Sabanathan D, Eslick GD, Shannon J. Use of Neoadjuvant Chemotherapy Plus Molecular Targeted Therapy in Colorectal Liver Metastases: A Systematic Review and Meta-analysis. Clin Colorectal Cancer. 2016;15(4):e141-e147.
Okuno M, Hatano E, Nishino H, Seo S, Taura K, Uemoto S. Does response rate of chemotherapy with molecular target agents correlate with the conversion rate and survival in patients with unresectable colorectal liver metastases?: A systematic review. Eur J Surg Oncol. 2017;43(6):1003–1012.
Beckers RCJ, Lambregts DMJ, Lahaye MJ, et al. Advanced imaging to predict response to chemotherapy in colorectal liver metastases - a systematic review. HPB (Oxford). 2018; 20(2):120–127.
Brouquet A, Overman MJ, Kopetz S, et al. Is resection of colorectal liver metastases after a second-line chemotherapy regimen justified? Cancer. 2011;117(19):4484–92.
Azab B, Shah N, Radbel J, et al. Pretreatment neutrophil/lymphocyte ratio is superior to platelet/lymphocyte ratio as a predictor of long-term mortality in breast cancer patients. Med Oncol. 2013;30(1):432.
Dirican N, Karakaya YA, Gunes S, Daloglu FT, Dirican A. Association of intra-tumoral tumour-infiltrating lymphocytes and neutrophil-to-lymphocyte ratio is an independent prognostic factor in non-small cell lung cancer. Clin Respir J. 2017;11(6):789–796.
Mlecnik B, Van den Eynde M, Bindea G, et al. Comprehensive Intrametastatic Immune Quantification and Major Impact of Immunoscore on Survival. J Natl Cancer Inst. 2018;110(1).
Chen ZY, Raghav K, Lieu CH, et al. Cytokine profile and prognostic significance of high neutrophil-lymphocyte ratio in colorectal cancer. Br J Cancer. 2015;112(6):1088–97.
Funding
This study was supported by National Natural Science Foundation of China (81672461), The capital health research and development of special (2018-1-4021), CAMS Innovation Fund for Medical Sciences (CIFMS) (Grant no. 2016-12M-1-001, no. 2017-12M-4-002), the State Key Project on Infection Diseases of China (Grant no. 2012ZX10002016).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content. All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors approved the final version to be published.
Corresponding authors
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mao, R., Zhao, JJ., Bi, XY. et al. A Low Neutrophil to Lymphocyte Ratio Before Preoperative Chemotherapy Predicts Good Outcomes After the Resection of Colorectal Liver Metastases. J Gastrointest Surg 23, 563–570 (2019). https://doi.org/10.1007/s11605-018-3796-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3796-8