Abstract
Background
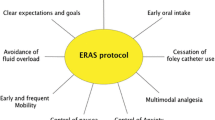
Enhanced recovery after surgery (ERAS) protocols have improved patient experience and outcomes in a variety of fields, including bariatric surgery. Given the increasing opioid epidemic in the USA, we sought to determine the impact of our own ERAS protocol on narcotic usage following laparoscopic sleeve gastrectomy.
Methods
Retrospective chart review was performed on patients undergoing primary laparoscopic sleeve gastrectomy for 6 months before and after implementation of an ERAS protocol. Our protocol strongly discouraged the use of narcotics in the postoperative period. Specific outcomes of interest were postoperative narcotic usage, length of stay, complications, and readmissions.
Results
Patient characteristics were similar in the two groups. ERAS implementation did not correlate with changes in length of stay, complications, or readmissions. However, ERAS implementation was associated with dramatic reductions in the use of intravenous narcotics (100% vs 47%, p < 0.01) and oral schedule 2 narcotics (56% vs 6%, p < 0.01), with an increase in the usage of tramadol (0% vs 36%, p < 0.01). After ERAS implementation, 52% of patients were managed without the use of schedule 2 narcotics (0% pre-ERAS, p < 0.01) and 33% received no narcotics of any kind (0% pre-ERAS, p < 0.01).
Conclusion
Implementation of an ERAS protocol for laparoscopic sleeve gastrectomy is associated with a dramatic reduction in the use of narcotics in the postoperative period. This has implementation for the usage of narcotics for laparoscopic surgery and potential elimination of narcotics for certain patients and procedures.
Similar content being viewed by others
References
Małczak P, Pisarska M, Piotr M, Wysocki M, Budzyński A, Pędziwiatr M. Enhanced Recovery after Bariatric Surgery: Systematic Review and Meta-Analysis. Obes Surg. 2017;27(1):226–35. doi:https://doi.org/10.1007/s11695-016-2438-z.
Egli F, Hofer S, Greminger P, Rhyner K. [Combined GM-CSF and erythropoietin therapy in myelodysplastic syndrome]. Schweiz Med Wochenschr. 1989;119(49):1777–80.
Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606–17.
King AB, Spann MD, Jablonski P, Wanderer JP, Sandberg WS, McEvoy MD. An enhanced recovery program for bariatric surgical patients significantly reduces perioperative opioid consumption and postoperative nausea. Surg Obes Relat Dis. 2018;14(6):849–56. doi:https://doi.org/10.1016/j.soard.2018.02.010.
Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg. 2013;37(2):259–84. doi:https://doi.org/10.1007/s00268-012-1772-0.
Gerrish AW, Fogel S, Lockhart ER, Nussbaum M, Adkins F. Opioid prescribing practices during implementation of an enhanced recovery program at a tertiary care hospital. Surgery. 2018;164(4):674–9. doi:https://doi.org/10.1016/j.surg.2018.06.034.
Cavallaro PM, Milch H, Savitt L, Hodin RA, Rattner DW, Berger DL et al. Addition of a scripted pre-operative patient education module to an existing ERAS pathway further reduces length of stay. Am J Surg. 2018;216(4):652–7. doi:https://doi.org/10.1016/j.amjsurg.2018.07.016.
Varadhan KK, Lobo DN, Ljungqvist O. Enhanced recovery after surgery: the future of improving surgical care. Crit Care Clin. 2010;26(3):527–47, x. doi:https://doi.org/10.1016/j.ccc.2010.04.003.
Bakker N, Cakir H, Doodeman HJ, Houdijk AP. Eight years of experience with Enhanced Recovery After Surgery in patients with colon cancer: Impact of measures to improve adherence. Surgery. 2015;157(6):1130–6. doi:https://doi.org/10.1016/j.surg.2015.01.016.
Singh PM, Panwar R, Borle A, Goudra B, Trikha A, van Wagensveld BA et al. Efficiency and Safety Effects of Applying ERAS Protocols to Bariatric Surgery: a Systematic Review with Meta-Analysis and Trial Sequential Analysis of Evidence. Obes Surg. 2017;27(2):489–501. doi:https://doi.org/10.1007/s11695-016-2442-3.
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–30. doi:https://doi.org/10.1001/archinternmed.2011.1827.
Kelly MA. Current Postoperative Pain Management Protocols Contribute to the Opioid Epidemic in the United States. Am J Orthop (Belle Mead NJ). 2015;44(10 Suppl):S5–8.
Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251.
Li L, Wu LT. Substance use after bariatric surgery: A review. J Psychiatr Res. 2016;76:16–29. doi:https://doi.org/10.1016/j.jpsychires.2016.01.009.
Mohanty S, Lee JS, Ross RA, Stricklen A, Carlin AM, Ghaferi AA. New Persistent Opioid Use after Bariatric Surgery. American College of Surgeons Clinical Congress. 2017. https://www.facs.org/media/press-releases/2017/ghaferi. Accessed August 15 2018.
Awad S, Carter S, Purkayastha S, Hakky S, Moorthy K, Cousins J et al. Enhanced recovery after bariatric surgery (ERABS): clinical outcomes from a tertiary referral bariatric centre. Obes Surg. 2014;24(5):753–8. doi:https://doi.org/10.1007/s11695-013-1151-4.
Lemanu DP, Singh PP, Berridge K, Burr M, Birch C, Babor R et al. Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg. 2013;100(4):482–9. doi:https://doi.org/10.1002/bjs.9026.
Barreca M, Renzi C, Tankel J, Shalhoub J, Sengupta N. Is there a role for enhanced recovery after laparoscopic bariatric surgery? Preliminary results from a specialist obesity treatment center. Surg Obes Relat Dis. 2016;12(1):119–26. doi:https://doi.org/10.1016/j.soard.2015.03.008.
Mannaerts GH, van Mil SR, Stepaniak PS, Dunkelgrün M, de Quelerij M, Verbrugge SJ et al. Results of Implementing an Enhanced Recovery After Bariatric Surgery (ERABS) Protocol. Obes Surg. 2016;26(2):303–12. doi:https://doi.org/10.1007/s11695-015-1742-3.
Matłok M, Pędziwiatr M, Major P, Kłęk S, Budzyński P, Małczak P. One hundred seventy-nine consecutive bariatric operations after introduction of protocol inspired by the principles of enhanced recovery after surgery (ERAS®) in bariatric surgery. Med Sci Monit. 2015;21:791–7. doi:https://doi.org/10.12659/MSM.893297.
Pimenta GP, Capellan DA, de Aguilar-Nascimento JE. Sleeve Gastrectomy With or Without a Multimodal Perioperative Care. A Randomized Pilot Study. Obes Surg. 2015;25(9):1639–46. doi:https://doi.org/10.1007/s11695-015-1573-2.
Klotz U. Tramadol--the impact of its pharmacokinetic and pharmacodynamic properties on the clinical management of pain. Arzneimittelforschung. 2003;53(10):681–7. doi:https://doi.org/10.1055/s-0031-1299812.
DEA. Drug Scheduling. https://www.dea.gov/druginfo/ds.shtml. Accessed July 25 2018.
Guy GP, Zhang K, Bohm MK, Losby J, Lewis B, Young R et al. Vital Signs: Changes in Opioid Prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697–704. doi:https://doi.org/10.15585/mmwr.mm6626a4.
Shafi S, Collinsworth AW, Copeland LA, Ogola GO, Qiu T, Kouznetsova M et al. Association of Opioid-Related Adverse Drug Events With Clinical and Cost Outcomes Among Surgical Patients in a Large Integrated Health Care Delivery System. JAMA Surg. 2018;153(8):757–63. doi:https://doi.org/10.1001/jamasurg.2018.1039.
O'Connor EC, Mead AN. Tramadol acts as a weak reinforcer in the rat self-administration model, consistent with its low abuse liability in humans. Pharmacol Biochem Behav. 2010;96(3):279–86. doi:https://doi.org/10.1016/j.pbb.2010.05.018.
Preston KL, Jasinski DR, Testa M. Abuse potential and pharmacological comparison of tramadol and morphine. Drug Alcohol Depend. 1991;27(1):7–17.
Wick EC, Grant MC, Wu CL. Postoperative Multimodal Analgesia Pain Management With Nonopioid Analgesics and Techniques: A Review. JAMA Surg. 2017;152(7):691–7. doi:https://doi.org/10.1001/jamasurg.2017.0898.
Acknowledgements
The authors would like to acknowledge Kristina Arnold for her assistance with data acquisition and Koffi Wima for his assistance with data analysis.
Author information
Authors and Affiliations
Contributions
RH designed the study and drafted the manuscript; RH, AS, and KS acquired the data; all authors interpreted the data, revised the manuscript, gave final approval of the manuscript, and are accountable for the work and its integrity.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoehn, R.S., Seitz, A.P., Singer, K.E. et al. Enhanced Recovery Protocol for Laparoscopic Sleeve Gastrectomy: Are Narcotics Necessary?. J Gastrointest Surg 23, 1541–1546 (2019). https://doi.org/10.1007/s11605-018-04091-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-04091-y