Abstract
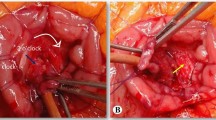
Extension of ampulloma into the lower common bile duct (CBD) is observed in up to 30% of cases. This biliary extension can prevent complete tumor resection thus is considered as a contraindication for endoscopic and even surgical ampullectomy. For ampullomas associated with a prolonged biliary extension, a pancreaticoduodenectomy is associated with a high morbidity and can be considered as an overtreatment for a benign neoplasm. The present study describes a new surgical approach including ampullectomy with complete resection of the intrapancreatic CBD and restoration of both biliary and pancreatic flow by two separate anastomoses. This procedure was performed in seven patients for a non-invasive ampulloma with a 25- to 70-mm CBD involvement. No patients died and three developed postoperative complications. Resection was R0 in all patients but one. With a 24-month median follow-up (range = 3–84), no patients developed pancreatic insufficiency or tumor recurrence.







Similar content being viewed by others
References
Napoleon B, Gincul R, Ponchon T, Berthiller J et al. Endoscopic papillectomy for early ampullary tumors: long-term results from a large multicenter prospective study. Endoscopy 2014; 46: 127–34.
Scheider L, Contin P, Fritz S, Strobel O et al. Surgical ampullectomy: an underestimated operation in the era of endoscopy. HPB (Oxford) 2016; 18: 65–71.
Bonhacker S, Seitz U, Nguyen D, Thonke F et al. Endoscopic resection of benign tumors of the duodenal papilla without and with intraductal growth. Gastrointest Endosc 2005; 62: 551–6.
Ceppa EP, Burbridge RA, Rialon KL, Omotosho PA et al. Endoscopic versus surgical ampullectomy: an algorithm to treat disease of the ampulla of Vater. Ann Surg 2013; 257: 315–22.
Ridtitid W, Tan D, Schmidt SE, Fogel EL, McHenry L, Watkins JL, Lehman GA et al, Endoscopic papillectomy: risk factors for incomplete resection and recurrence during long-term follow-up. Gastrointest Endosc 2014; 79: 289–96.
Yoon YS, Kim SW, Park SJ, Lee HS, et al. Clinicopathologic analysis of early ampullary cancers with a focus on the feasibility of ampullectomy. Ann Surg 2005; 242: 92–100.
Adsay V, Ohike N, Tajiri T, Kim GE et al. Ampullary region carcinomas definition and site specific classification with delineation of four clinicopathologically and prognostically distinct subsets in an analysis of 249 cases. Am J Surg Pathol 2012; 36: 1592–1608.
Ohike N, Kim GE, Tajiri T, Krasinskas A et al. Intra-ampullary papillary-tubular neoplasm (IAPN): characterization of tumoral intraepithelial neoplasia occurring within the ampulla: a clinicopathologic analysis of 82 cases. Am J Surg Pathol 2010; 34: 1731–1748.
Mathur A, Paul H, Ross S, Luberice K et al. Transduodenal ampullectomy for ampullary adenomas: a safe and effective procedure with long-term salutary outcomes. Am Surg 2014; 80: 185–90.
Rocha FG, Lee H, Katabi N, De Matteo RP et al. Intraductal papillary neoplasm of the bile duct: A biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology 2012;56:1352–1360.
Ragot E, Mabrut JY, Ouaissi M, Sauvanet A et al. Pancreaticobiliary maljunctions in European patients with bile duct cysts: Results of the multicenter study of the French Surgical Association. World J Surg 2017; 41: 538–545.
Burkhart RA, Gerber SM, Tholey RM, Lamb KM et al. Incidence and severity of pancreatogenic diabetes after pancreatic resection. J Gastrointest Surg 2015 19:217–225.
Falconi M, Mantovani W, Crippa S, Mascetta G et al. Pancreatic insufficiency after different resections for benign tumours. Br J Surg 2008; 95: 85–91.
Keck T, Wellner UF, Bahra M, Klein F et al. Pancreatogastrostomy versus pancreatojejunostomy for reconstruction after pancreatoduodenectomy (RECOPANC): perioperative and long-term results of a multicenter randomized controlled trial. Ann Surg 2016; 263 :440–9.
Panis Y, Fagniez PL, Brisset D, Lacaine F et al. Long term results of choledocho-duodenostomy versus choledocho-jejunostomy for choledocholithiasis. The French Association for Surgical Research. Surg Gynecol Obstet. 1993; 177: 33–7.
Luu C, Lee B, Stabile BE. Choledochoduodenostomy as the biliary-enteric bypass of choice for benign and malignant distal common bile duct strictures Am Surg. 2013; 79: 1054–7.
Alessandrino F, Ivanovic AM, Yee EU, Radulovic D et al. MDCT and MRI of the ampulla of Vater. Part I: technique optimization, normal anatomy, and epithelial neoplasms. Abdom Imaging 2015; 40: 3274–91.
Clary BM, Tyler DS, Dematos P, Gottfried M, et al. Local ampullary resection with careful intraoperative frozen section evaluation for presumed benign ampullary neoplasms. Surgery 2000; 127: 628–33.
Roggin KK, Yeh JJ, Ferrone CR, Riedel E et al. Limitations of ampullectomy in the treatment of nonfamilial ampullary neoplasms. Ann Surg Oncol 2005;12: 971–8.
Grobmyer SR, Stasik CN, Draganov P, Hemming AW, et al. Contemporary results with ampullectomy for 29 “benign” neoplasms of the ampulla. J Am Coll Surg 2008; 206: 466–71.
Kim J, Choi SH, Choi DW, Heo JS, et al. Role of transduodenal ampullectomy for tumors of the ampulla of Vater. J Korean Surg Soc. 2011; 81: 250–6.
Author Contribution
Alain Sauvanet: conception of the work; acquisition, analysis, and interpretation of data; drafting the work; final approval of the version to be published; and agreement to be accountable for all aspects of the work.
Safi Dokmak: acquisition and interpretation of data; revising the work critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work.
Jérome Cros: acquisition and interpretation of data; revising the work critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work.
Dominique Cazals-Hatem: acquisition and interpretation of data; revising the work critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work.
Philippe Ponsot: conception or design of the work; revising the work critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work.
Maxime Palazzo: acquisition and interpretation of data; revising the work critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Previous Presentation
No.
Conflict of Interest
All six authors have no financial disclosure or conflict of interest in relation to this work.
Rights and permissions
About this article
Cite this article
Sauvanet, A., Dokmak, S., Cros, J. et al. Surgical Ampullectomy with Complete Resection of the Common Bile Duct: a New Procedure for Radical Resection of Non-invasive Ampulloma with Biliary Extension. J Gastrointest Surg 21, 1533–1539 (2017). https://doi.org/10.1007/s11605-017-3457-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3457-3