Abstract
Background
The health benefits of probiotics and synbiotics are well established in healthy adults, but their role in preventing postoperative sepsis remains controversial. This meta-analysis assesses the impact of probiotics and synbiotics on the incidence of postoperative sepsis in gastrointestinal (GI) surgical patients.
Methods
A comprehensive literature search of all published randomized control trials (RCTs) was conducted using PubMed, Cochrane Central Registry of Controlled Trials, and Google Scholar (1966–2015). Inclusion criteria included RCTs comparing the use of any strain or dose of a specified probiotic/synbiotic with placebo or a “no treatment” control group. The incidence of postoperative sepsis (within 1 month of surgery) and postoperative mortality were analyzed.
Results
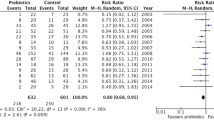
Fifteen RCTs involving 1201 patients (192 receiving probiotics, 413 receiving synbiotics, and 596 receiving placebo) were analyzed. Overall, probiotic and synbiotic uses significantly reduced the risk of developing postoperative sepsis by 38 % (relative risk (RR) = 0.62, 95 % confidence interval (CI) 0.52–0.74, p < 0.001).
Conclusions
The use of probiotic/synbiotic supplementation is associated with a significant reduction in the risk of developing postoperative sepsis in patients undergoing elective GI surgery. Probiotic/synbiotic supplementation is a valuable adjunct in the care of patients undergoing GI surgery. Additional studies are required to determine the optimal dose and strain of probiotic/synbiotic.






Similar content being viewed by others
References
Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003;348(16):1546-1554.
Martin CM, Priestap F, Fisher H et al. A prospective, observational registry of patients with severe sepsis: the Canadian Sepsis Treatment and Response Registry. Crit Care Med 2009;37(1):81-88.
Bone RC, Balk RA, Cerra FB et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992;101(6):1644-1655.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001;29(7):1303-1310.
Levy MM, Dellinger RP, Townsend SR et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med 2010;36(2):222-231.
Moore LJ, Moore FA, Jones SL, Xu J, Bass BL. Sepsis in general surgery: a deadly complication. Am J Surg 2009;198(6):868-874.
Wang XD, Soltesz V, Andersson R, Bengmark S. Bacterial translocation in acute liver failure induced by 90 percent hepatectomy in the rat. Br J Surg 1993;80(1):66-71.
MacFie J. Current status of bacterial translocation as a cause of surgical sepsis. Br Med Bull 2004;71:1-11.
MacFie J, O’Boyle C, Mitchell CJ, Buckley PM, Johnstone D, Sudworth P. Gut origin of sepsis: a prospective study investigating associations between bacterial translocation, gastric microflora, and septic morbidity. Gut 1999;45(2):223-228.
Bengmark S. Pre-, pro- and synbiotics. Curr Opin Clin Nutr Metab Care 2001;4(6):571-579.
Deitch EA. The role of intestinal barrier failure and bacterial translocation in the development of systemic infection and multiple organ failure. Arch Surg 1990;125(3):403-404.
Rayes N, Seehofer D, Theruvath T et al. Effect of enteral nutrition and synbiotics on bacterial infection rates after pylorus-preserving pancreatoduodenectomy: a randomized, double-blind trial. Ann Surg 2007;246(1):36-41.
de Vrese M, Schrezenmeir J. Probiotics, prebiotics, and synbiotics. Adv Biochem Eng Biotechnol 2008;111:1-66.
Shanahan F. Probiotics in perspective. Gastroenterology 2010;139(6):1808-1812.
Schrezenmeir J, de VM. Probiotics, prebiotics, and synbiotics—approaching a definition. Am J Clin Nutr 2001;73(2 Suppl):361S-364S.
Kinross JM, Markar S, Karthikesalingam A et al. A meta-analysis of probiotic and synbiotic use in elective surgery: does nutrition modulation of the gut microbiome improve clinical outcome? JPEN J Parenter Enteral Nutr 2013;37(2):243-253.
Liu Z, Li C, Huang M et al. Positive regulatory effects of perioperative probiotic treatment on postoperative liver complications after colorectal liver metastases surgery: a double-center and double-blind randomized clinical trial. BMC Gastroenterol 2015;15(1):34.
Okazaki M, Matsukuma S, Suto R et al. Perioperative synbiotic therapy in elderly patients undergoing gastroenterological surgery: a prospective, randomized control trial. Nutrition 2013;29(10):1224-1230.
Rayes N, Hansen S, Seehofer D et al. Early enteral supply of fiber and Lactobacilli versus conventional nutrition: a controlled trial in patients with major abdominal surgery. Nutrition 2002;18(7-8):609-615.
Rayes N, Seehofer D, Hansen S et al. Early enteral supply of lactobacillus and fiber versus selective bowel decontamination: a controlled trial in liver transplant recipients. Transplantation 2002;74(1):123-127.
Anderson AD, McNaught CE, Jain PK, MacFie J. Randomised clinical trial of synbiotic therapy in elective surgical patients. Gut 2004;53(2):241-245.
Kanazawa H, Nagino M, Kamiya S et al. Synbiotics reduce postoperative infectious complications: a randomized controlled trial in biliary cancer patients undergoing hepatectomy. Langenbecks Arch Surg 2005;390(2):104-113.
Rayes N, Seehofer D, Theruvath T et al. Supply of pre- and probiotics reduces bacterial infection rates after liver transplantation—a randomized, double-blind trial. Am J Transplant 2005;5(1):125-130.
Reddy BS, MacFie J, Gatt M, Larsen CN, Jensen SS, Leser TD. Randomized clinical trial of effect of synbiotics, neomycin and mechanical bowel preparation on intestinal barrier function in patients undergoing colectomy. Br J Surg 2007;94(5):546-554.
Usami M, Miyoshi M, Kanbara Y et al. Effects of perioperative synbiotic treatment on infectious complications, intestinal integrity, and fecal flora and organic acids in hepatic surgery with or without cirrhosis. JPEN J Parenter Enteral Nutr 2011;35(3):317-328.
Eguchi S, Takatsuki M, Hidaka M, Soyama A, Ichikawa T, Kanematsu T. Perioperative synbiotic treatment to prevent infectious complications in patients after elective living donor liver transplantation: a prospective randomized study. Am J Surg 2011;201(4):498-502.
Liu Z, Qin H, Yang Z et al. Randomised clinical trial: the effects of perioperative probiotic treatment on barrier function and post-operative infectious complications in colorectal cancer surgery—a double-blind study. Aliment Pharmacol Ther 2011;33(1):50-63.
Yokoyama Y, Nishigaki E, Abe T et al. Randomized clinical trial of the effect of perioperative synbiotics versus no synbiotics on bacterial translocation after oesophagectomy. Br J Surg 2014;101(3):189-199.
Kotzampassi K, Stavrou G, Damoraki G et al. A four-probiotics regimen reduces postoperative complications after colorectal surgery: a randomized, double-blind, placebo-controlled study. World J Surg 2015;39(11):2776-2783.
Sommacal HM, Bersch VP, Vitola SP, Osvaldt AB. Perioperative synbiotics decrease postoperative complications in periampullary neoplasms: a randomized, double-blind clinical trial. Nutr Cancer 2015;67(3):457-462.
Parrillo JE, Parker MM, Natanson C et al. Septic shock in humans. Advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy. Ann Intern Med 1990;113(3):227-242.
Hoyert DL, Arias E, Smith BL, Murphy SL, Kochanek KD. Deaths: final data for 1999. Natl Vital Stat Rep 2001;49(8):1-113.
Vogel TR, Dombrovskiy VY, Carson JL, Graham AM, Lowry SF. Postoperative sepsis in the United States. Ann Surg 2010;252(6):1065-1071.
Perl TM, Dvorak L, Hwang T, Wenzel RP. Long-term survival and function after suspected gram-negative sepsis. JAMA 1995;274(4):338-345.
Depeint F, Tzortzis G, Vulevic J, I’anson K, Gibson GR. Prebiotic evaluation of a novel galactooligosaccharide mixture produced by the enzymatic activity of Bifidobacterium bifidum NCIMB 41171, in healthy humans: a randomized, double-blind, crossover, placebo-controlled intervention study. Am J Clin Nutr 2008;87(3):785-791.
Vulevic J, Drakoularakou A, Yaqoob P, Tzortzis G, Gibson GR. Modulation of the fecal microflora profile and immune function by a novel trans-galactooligosaccharide mixture (B-GOS) in healthy elderly volunteers. Am J Clin Nutr 2008;88(5):1438-1446.
Drakoularakou A, Tzortzis G, Rastall RA, Gibson GR. A double-blind, placebo-controlled, randomized human study assessing the capacity of a novel galacto-oligosaccharide mixture in reducing travellers’ diarrhoea. Eur J Clin Nutr 2010;64(2):146-152.
Lau CS, Chamberlain RS. Probiotics are effective at preventing clostridium difficile-associated diarrhea: a systematic review and meta-analysis. Int J Gen Med 2016;9:27-37.
Salminen MK, Tynkkynen S, Rautelin H et al. Lactobacillus bacteremia during a rapid increase in probiotic use of Lactobacillus rhamnosus GG in Finland. Clin Infect Dis 2002;35(10):1155-1160.
Besselink MG, van Santvoort HC, Buskens E et al. [Probiotic prophylaxis in patients with predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial]. Ned Tijdschr Geneeskd 2008;152(12):685-696.
Van den Nieuwboer M, Brummer RJ, Guarner F, Morelli L, Cabana M, Claasen E. The administration of probiotics and synbiotics in immune compromised adults: is it safe? Benef Microbes 2015;6(1):3-17.
Liu ZH, Huang MJ, Zhang XW et al. The effects of perioperative probiotic treatment on serum zonulin concentration and subsequent postoperative infectious complications after colorectal cancer surgery: a double-center and double-blind randomized clinical trial. Am J Clin Nutr 2013;97(1):117-126.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arumugam, S., Lau, C.S.M. & Chamberlain, R.S. Probiotics and Synbiotics Decrease Postoperative Sepsis in Elective Gastrointestinal Surgical Patients: a Meta-Analysis. J Gastrointest Surg 20, 1123–1131 (2016). https://doi.org/10.1007/s11605-016-3142-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3142-y