Abstract
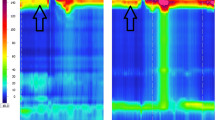
The motility of the pharynx and upper esophageal sphincter (UES) is still poorly understood. It is also unclear if the motility of this area may be compromised in patients with achalasia. This study aims to evaluate the motility of the pharynx, UES, and proximal esophagus in patients with esophageal achalasia. Sixty patients with achalasia underwent high-resolution manometry (HRM) (52 % females, mean age 54 years). Esophageal dilatation was classified according to the radiologic diameter in Type I (<4 cm): 6 %; Type II (4–7 cm): 36 %; Type III (7–10 cm): 34 %; and Type IV (>10 cm): 24 %. HRM classified 43 % of the patients as Chicago Type I and 57 % as Type II. Manometric parameters were compared to normal values obtained from a previous study in volunteers. The motility of the velopharynx showed short, premature, and hypertonic contraction. The epiglottis also showed hypertonic contraction. The UES had increased residual pressure. Chicago classification Type II patients had higher UES residual pressure (p = 0.03). The degree of esophageal dilatation did not correlate with manometric parameters. Achalasia may affect the motility of the pharyngo-upper esophageal area. The changes observed may represent functional alterations to prevent aspiration, especially in patients with Chicago classification Type II achalasia.


Similar content being viewed by others
References
Silva LC, Herbella FAM, Neves LR, Vicentine FPP, Neto SP, Patti MG. Anatomophysiology of the pharyngo-upper esophageal area in light of high-resolution manometry. J Gastrointest Surg 2013; 17:2033–2038.
Takasaki K, Umeki H, Enatsu K, Tanaka F, Sakihama N, Kumagami H, Takahashi H. Investigation of pharyngeal swallowing function using high-resolution manometry. Laryngoscope 2008; 118:1729–1732.
Weijenborg PW, Kessing BF, Smout AJPM, Bredenoord AJ. Normal values for solid-state esophageal high-resolution manometry in a European population; an overview of all current metrics. Neurogastroentero Motil 2014; 26:654–659.
Mittal RL. Motor function of the pharynx, esophagus and its sphincters. San Rafael (CA): Morgan & Claypoll Life Sciences; 2011.
Ayazi S, Crookes PF. High-resolution esophageal manometry: using technical advances for clinical advantages. J Gastrointest Surh 2010; 14 Suppl 1: S24-32.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, Pandolfino JE, International High Resolution Manometry Working Group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015; 27:160–174.
Dantas RO. Upper esophageal sphincter pressure in patients with Chagas’ disease and primary achalasia. Brazil J Med Biol Res 2000; 33:545–551.
Yoneyama F, Miyachi M, Nimura Y. Manometric findings of the upper esophageal sphincter in esophageal achalasia. World J Surg 1998; 22:1043–1047.
Dudnick RS, Castell JA, Castell DO. Abnormal upper esophageal sphincter function in achalasia. Am J Gastroenterol 1992; 87(12):1712–1715.
Ali GN, Hunt DR, Jorgensen JO, de Carle DJ, Cook IJ. Esophageal achalasia and coexistent upper esophageal sphincter relaxation disorder presenting with airway obstruction. Gastroenterology 1995; 109:1328–1332.
Becker DJ, Castell DO. Acute airway obstruction in achalasia: possible role of defective belch reflex. Gastroenterology 1989; 97:1323–1326.
Chavez YH, Ciarleglio MM, Clarke JO, Nandwani M, Stein E, Roland BC. Upper esophageal sphincter abnormalities: Frequent finding on high-resolution esophageal manometry and association with poorer treatment response in achalasia. J Clin Gastroenterol 2015; 49:17–23.
Jee SR, Pimentel M, Soffer E, Conklin JL. A high-resolution view of achalasia. J Clin Gastroenterol 2009; 43:644–651.
Mathews SC, Ciarleglio M, Chavez YH, Clarke JO, Stein E, Roland BC. Upper esophageal sphincter abnormalities are strongly predictive of treatment response in patients with achalasia. World J Clin Cases 2014; 2:448–454.
Rezende DT, Herbella FAM, Silva LC, Panocchia Neto S, Patti MG. Upper esophageal sphincter resting pressure varies during esophageal manometry. Arq Bras Cir Dig 2014; 27:182–183.
Tokashiki R, Funato N, Suzuki M. Globus sensation and increased upper esophageal sphincter pressure with distal esophageal acid perfusion. Eur Arch Otorhinolaryngol 2010; 267:737–741.
Vicentine FP, Herbella FA, Allaix ME, Silva LC, Patti MG. High-resolution manometry classifications for idiopathic achalasia in patients with Chagas’ disease esophagopathy. J Gastrointest Surg. 2014 Feb;18(2):221–4; discussion 224–5. doi: 10.1007/s11605-013-2376-1. Epub 2013 Oct 16.
Wauters L, Van Oudenhove L, Selleslagh M, Vanuytsel T, Boeckxstaens G, Tack J, Omari T, Rommel N. Balloon dilation of the esophago-gastric junction affects lower and upper esophageal sphincter function in achalasia. Neurogastroenterol Motil 2014; 26:69–76.
Takasaki K, Umeki H, Hara M, Kumagami H, Takahashi H. Influence of effortful swallow on pharyngeal pressure: evaluation using a high-resolution manometry. Otolaryngol Head Neck Surg 2011; 144:16–20.
Herbella FAM, Oliveira DRCF, Del Grande JC. Are idiophatic and chagasic achalasia two different disease. Dig Dis Scien 2004; 3:353–360.
Vicentine FPP, Herbella FAM, Allaix ME, Silva LC, Patti MG. Comparison of idiopathic achalasia and Chagas’ disease esophagopathy at of high-resolution manometry. Dis Esophagus 2014; 27:128–133.
Conflict of Interest
Authors declare that they have no competing interests.
Author’s Contribution
MAM and FAMH did the conception and design, acquisition of data, analysis and interpretation of data, drafting the article, and final approval of the version to be published. MGP did the review for intellectual content and final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menezes, M.A., Herbella, F.A.M. & Patti, M.G. High-Resolution Manometry Evaluation of the Pharynx and Upper Esophageal Sphincter Motility in Patients with Achalasia. J Gastrointest Surg 19, 1753–1757 (2015). https://doi.org/10.1007/s11605-015-2901-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2901-5