Abstract
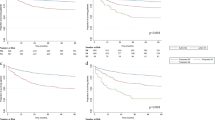
The objective of this study was to analyze the prognostic significance of metastatic lymph node status in gastric neuroendocrine carcinoma (GNEC) patients following radical gastrectomy. A consecutive series of 73 patients who underwent gastrectomy between 1999 and 2011 for GNEC was retrospectively reviewed. Indexes of lymph node involvement (the pN classification, metastatic lymph node number [MLNn], ratio [MLNr], and station [MLNs]) and other clinicopathological data were analyzed. Fifty-four patients met the inclusion criteria and were enrolled in the study. Among them, 44 patients (81 %) were found to have lymph node metastases. The median survival time of the entire cohort was 63.2 (range, 14–153) months with 3- and 5-year survival rates of 88.9 and 47.9 %, respectively. The median total number of lymph nodes, MLNn, and MLNr were 19 (range, 10–56), 5 (range, 1–21), and 25 % (6–100 %), respectively. Cox regression analysis revealed pN classification = 1, MLNn >2, MLNr >0.1, and MLNs = 2, and distant metastases influenced prognosis independently (P = 0.0266, 0.0091, 0.0031, 0.0119, and 0.0021, respectively). In addition to the pN classification, indexes of metastatic lymph node involvement, including MLNn, MLNr, and MLNs, were all significant predictors of survival in GNEC patients. Distant metastasis was also a significant prognostic factor. These indexes proved to be accurate and important supplements to survival factors, which may improve risk classification of GNEC patients.



Similar content being viewed by others
References
Modlin IM, Moss SF, Oberg K, Padbury R, Hicks RJ, Gustafsson BI, Wright NA, Kidd M. Gastrointestinal neuroendocrine (carcinoid) tumours: current diagnosis and management. The Medical journal of Australia 2010, 193:46–52.
Bosman FT CF, Hruban RH & Theise ND (Eds). WHO Classification of Tumors of the Digestive System, 4th ed. Geneva, Switzerland: World Health Organization Press; 2010.
Modlin IM, Moss SF, Chung DC, Jensen RT, Snyderwine E. Priorities for improving the management of gastroenteropancreatic neuroendocrine tumors. Journal of the National Cancer Institute 2008, 100:1282–1289.
Borch K, Ahren B, Ahlman H, Falkmer S, Granerus G, Grimelius L. Gastric carcinoids: biologic behavior and prognosis after differentiated treatment in relation to type. Annals of surgery 2005, 242:64–73.
Saito H, Fukumoto Y, Osaki T, Fukuda K, Tatebe S, Tsujitani S, Ikeguchi M. Prognostic significance of level and number of lymph node metastases in patients with gastric cancer. Annals of surgical oncology 2007, 14:1688–1693.
Japanese Gastric Cancer A. Japanese Classification of Gastric Carcinoma—2nd English Edition. Gastric cancer : official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 1998, 1:10–24.
Tsikitis VL, Wertheim BC, Guerrero MA. Trends of incidence and survival of gastrointestinal neuroendocrine tumors in the United States: a seer analysis. Journal of Cancer 2012, 3:292–302.
Sobin LH GM, Wittekind C. TNM classification of malignant tumors, 7th ed., 7 edn: Oxford: Wiley-Blackwell; 2009.
Crosby DA, Donohoe CL, Fitzgerald L, Muldoon C, Hayes B, O’Toole D, Reynolds JV. Gastric neuroendocrine tumours. Digestive surgery 2012, 29:331–348.
Frilling A, Li J, Malamutmann E, Schmid KW, Bockisch A, Broelsch CE. Treatment of liver metastases from neuroendocrine tumours in relation to the extent of hepatic disease. The British journal of surgery 2009, 96:175–184.
Sasako M, Saka M, Fukagawa T, Katai H, Sano T. Surgical treatment of advanced gastric cancer: Japanese perspective. Digestive surgery 2007, 24:101–107.
Massucco P, Ribero D, Sgotto E, Mellano A, Muratore A, Capussotti L. Prognostic significance of lymph node metastases in pancreatic head cancer treated with extended lymphadenectomy: not just a matter of numbers. Annals of surgical oncology 2009, 16:3323–3332.
Pape UF, Berndt U, Muller-Nordhorn J, Bohmig M, Roll S, Koch M, Willich SN, Wiedenmann B. Prognostic factors of long-term outcome in gastroenteropancreatic neuroendocrine tumours. Endocrine-related cancer 2008, 15:1083–1097.
Kapoor NS, Shamonki J, Sim MS, Chung CT, Giuliano AE. Impact of multifocality and lymph node metastasis on the prognosis and management of microinvasive breast cancer. Annals of surgical oncology 2013, 20:2576–2581.
Kitagawa M, Ichikawa D, Komatsu S, Okamoto K, Shiozaki A, Fujiwara H, Murayama Y, Kuriu Y, Ikoma H, Nakanishi M. Evaluation of lymph node metastasis in patients with gastric cancer: a comparison of the directionality of lymph node metastasis and the total number of metastatic lymph nodes. Surgery today 2013, 43:130–135.
Karpeh MS, Leon L, Klimstra D, Brennan MF. Lymph node staging in gastric cancer: is location more important than Number? An analysis of 1,038 patients. Annals of surgery 2000, 232:362–371.
Espin F, Bianchi A, Llorca S, Feliu J, Palomera E, Garcia O, Remon J, Sunol X. Metastatic lymph node ratio versus number of metastatic lymph nodes as a prognostic factor in gastric cancer. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 2012, 38:497–502.
Yu JX, Li Y. The staging system of metastatic lymph node ratio in gastric cancer. Clinical oncology 2007, 19:269–270.
Yamashita K, Sakuramoto S, Kikuchi S, Katada N, Kobayashi N, Watanabe M. Surgical resection of stage IV gastric cancer and prognosis. Anticancer research 2007, 27:4381–4386.
Marchet A, Mocellin S, Ambrosi A, Morgagni P, Garcea D, Marrelli D, Roviello F, de Manzoni G, Minicozzi A, Natalini G. The ratio between metastatic and examined lymph nodes (N ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an Italian multicentric study in 1853 patients. Annals of surgery 2007, 245:543–552.
Liu C, Lu P, Lu Y, Xu H, Wang S, Chen J. Clinical implications of metastatic lymph node ratio in gastric cancer. BMC cancer 2007, 7:200.
Xiao LB, Yu JX, Wu WH, Xu FF, Yang SB. Superiority of metastatic lymph node ratio to the 7th edition UICC N staging in gastric cancer. World journal of gastroenterology : WJG 2011, 17:5123–5130.
Zhang M, Zhu G, Ma Y, Xue Y. Comparison of four staging systems of lymph node metastasis in gastric cancer. World journal of surgery 2009, 33:2383–2388.
Kunisaki C, Shimada H, Nomura M, Matsuda G, Otsuka Y, Ono H, Akiyama H. Distribution of lymph node metastasis in gastric carcinoma. Hepato-gastroenterology 2006, 53:468–472.
Glazer ES, Tseng JF, Al-Refaie W, Solorzano CC, Liu P, Willborn KA, Abdalla EK, Vauthey JN, Curley SA. Long-term survival after surgical management of neuroendocrine hepatic metastases. HPB : the official journal of the International Hepato Pancreato Biliary Association 2010, 12:427–433.
Mayo SC, de Jong MC, Pulitano C, Clary BM, Reddy SK, Gamblin TC, Celinksi SA, Kooby DA, Staley CA, Stokes JB. Surgical management of hepatic neuroendocrine tumor metastasis: results from an international multi-institutional analysis. Annals of surgical oncology 2010, 17:3129–3136.
Elias D, Lasser P, Ducreux M, Duvillard P, Ouellet JF, Dromain C, Schlumberger M, Pocard M, Boige V, Miquel C. Liver resection (and associated extrahepatic resections) for metastatic well-differentiated endocrine tumors: a 15-year single center prospective study. Surgery 2003, 133:375–382.
Sarmiento JM, Heywood G, Rubin J, Ilstrup DM, Nagorney DM, Que FG. Surgical treatment of neuroendocrine metastases to the liver: a plea for resection to increase survival. Journal of the American College of Surgeons 2003, 197:29–37.
Yao JC. Neuroendocrine tumors. Molecular targeted therapy for carcinoid and islet-cell carcinoma. Best practice & research Clinical endocrinology & metabolism 2007, 21:163–172.
McStay MK, Maudgil D, Williams M, Tibballs JM, Watkinson AF, Caplin ME, Buscombe JR. Large-volume liver metastases from neuroendocrine tumors: hepatic intraarterial 90Y-DOTA-lanreotide as effective palliative therapy. Radiology 2005, 237:718–726.
Gut P, Fischbach J, Kaminski G, Ruchala M. Contemporary methods of therapy and follow-up of neuroendocrine tumours of the gastrointestinal tract and the pancreas. Contemporary oncology 2012, 16:371–375.
Kulke MH, Stuart K, Enzinger PC, Ryan DP, Clark JW, Muzikansky A, Vincitore M, Michelini A, Fuchs CS. Phase II study of temozolomide and thalidomide in patients with metastatic neuroendocrine tumors. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 2006, 24:401–406.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, X., Chen, Y., Guo, L. et al. Prognostic Significance of Metastatic Lymph Node Number, Ratio and Station in Gastric Neuroendocrine Carcinoma. J Gastrointest Surg 19, 234–241 (2015). https://doi.org/10.1007/s11605-014-2691-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2691-1