Abstract
Purpose
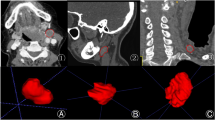
To investigate the ability of deep learning (DL) using convolutional neural networks (CNNs) for distinguishing between normal and metastatic axillary lymph nodes on ultrasound images by comparing the diagnostic performance of radiologists.
Materials and methods
We retrospectively gathered 300 images of normal and 328 images of axillary lymph nodes with breast cancer metastases for training. A DL model using the CNN architecture Xception was developed to analyze test data of 50 normal and 50 metastatic lymph nodes. A board-certified radiologist with 12 years’ experience.
(Reader 1) and two residents with 3- and 1-year experience (Readers 2, 3), respectively, scored these test data with and without the assistance of the DL system for the possibility of metastasis. The sensitivity, specificity, and area under the receiver operating characteristic curve (AUC) were calculated.
Results
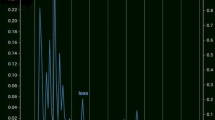
Our DL model had a sensitivity of 94%, a specificity of 88%, and an AUC of 0.966. The AUC of the DL model was not significantly different from that of Reader 1 (0.969; p = 0.881) and higher than that of Reader 2 (0.913; p = 0.101) and Reader 3 (0.810; p < 0.001). With the DL support, the AUCs of Readers 2 and 3 increased to 0.960 and 0.937, respectively, which were comparable to those of Reader 1 (p = 0.138 and 0.700, respectively).
Conclusion
Our DL model demonstrated great diagnostic performance for differentiating benign from malignant axillary lymph nodes on breast ultrasound and for potentially providing effective diagnostic support to residents.




Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569–75.
Fujioka T, Mori M, Kubota K, et al. Clinical usefulness of ultrasound-guided fine needle aspiration and core needle biopsy for patients with axillary lymphadenopathy. Medicina (Kaunas). 2021;57:722.
Kikuchi Y, Mori M, Fujioka T, et al. Feasibility of ultrafast dynamic magnetic resonance imaging for the diagnosis of axillary lymph node metastasis: a case report. Eur J Radiol Open. 2020;7:100261.
Mori M, Fujioka T, Katsuta L, et al. Diagnostic performance of time-of-flight PET/CT for evaluating nodal metastasis of the axilla in breast cancer. Nucl Med Commun. 2019;40:958–64.
Kornecki A. Current status of breast ultrasound. Can Assoc Radiol J. 2011;62:31–40.
Newell MS, Mahoney MC. Ultrasound-guided percutaneous breast biopsy. Tech Vasc Interv Radiol. 2014;17:23–31.
Youk JH, Son EJ, Gweon HM, Kim H, Park YJ, Kim JA. Comparison of strain and shear wave elastography for the differentiation of benign from malignant breast lesions, combined with B-mode ultrasonography: qualitative and quantitative assessments. Ultrasound Med Biol. 2014;40:2336–44.
Yasaka K, Akai H, Kunimatsu A, Kiryu S, Abe O. Deep learning with convolutional neural network in radiology. Jpn J Radiol. 2018;36:257–72.
Fujioka T, Mori M, Kubota K, et al. The utility of deep learning in breast ultrasonic imaging: a review. Diagnostics (Basel). 2020;10:1055.
Chartrand G, Cheng PM, Vorontsov E, Drozdzal M, Turcotte S, Pal CJ, et al. Deep learning: a primer for radiologists. Radiographics. 2017;37:2113–31.
Han S, Kang HK, Jeong JY, Park MH, Kim W, Bang WC, et al. A deep learning framework for supporting the classification of breast lesions in ultrasound images. Phys Med Biol. 2017;62:7714–28.
Huang Q, Zhang F, Li X. Machine learning in ultrasound computer-aided diagnostic systems: a survey. Biomed Res Int. 2018;4:5137904.
Szegedy C, Liu W, Jia Y, Sermanet P, Reed S, Anguelov D, et al. Going deeper with convolutions. In: Proceedings of the IEEE conference on computer vision and pattern recognition. 2015. p. 1–9. https://arxiv.org/abs/1409.4842.
D’Orsi C, Sickles E, Mendelson E, Morris E. Breast imaging reporting and data system. In: ACR BI-RADS® Atlas. 5th ed. Reston, VA: American College of Radiology 2013.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
McKinney SM, Sieniek M, Godbole V, Godwin J, Antropova N, Ashrafian H, et al. International evaluation of an AI system for breast cancer screening. Nature. 2020;577:89–94.
Fujioka T, Kubota K, Mori M, et al. Distinction between benign and malignant breast masses at breast ultrasound using deep learning method with convolutional neural network. Jpn J Radiol. 2019;37:466–72.
Adachi M, Fujioka T, Mori M, et al. Detection and diagnosis of breast cancer using artificial intelligence based assessment of maximum intensity projection dynamic contrast-enhanced magnetic resonance images. Diagnostics (Basel). 2020;10:330.
Fujioka T, Katsuta L, Kubota K, et al. Classification of breast masses on ultrasound shear wave elastography using convolutional neural networks. Ultrason Imaging. 2020;42:213–20.
Tahmasebi A, Qu E, Sevrukov A, et al. Assessment of axillary lymph nodes for metastasis on ultrasound using artificial intelligence. Ultrason Imaging. 2021;43:329–36.
Bae MS. Using deep learning to predict axillary lymph node metastasis from US images of breast cancer. Radiology. 2020;294:29–30.
Zhou LQ, Wu XL, Huang SY, et al. Lymph node metastasis prediction from primary breast cancer US images using deep learning. Radiology. 2020;294:19–28.
Sun Q, Lin X, Zhao Y, Learning D, vs., et al. Radiomics for predicting axillary lymph node metastasis of breast cancer using ultrasound images: don’t forget the peritumoral region. Front Oncol. 2020;10:53.
M Claesen, B De Moor. Hyperparameter search in machine learning. arXiv: 1502.02127 [Preprint].2015. Available from: https://arXiv.org/abs/1502.02127. Accessed 8 Jan 2022.
Demircioğlu O, Uluer M, Arıbal E. How many of the biopsy decisions taken at inexperienced breast radiology units were correct? J Breast Health. 2017;13:23–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures used in this research were approved by the Ethics Committee of Tokyo Medical and Dental University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ozaki, J., Fujioka, T., Yamaga, E. et al. Deep learning method with a convolutional neural network for image classification of normal and metastatic axillary lymph nodes on breast ultrasonography. Jpn J Radiol 40, 814–822 (2022). https://doi.org/10.1007/s11604-022-01261-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-022-01261-6