Abstract
Objectives
The purpose of this study was to evaluate the diagnostic value of multimodal ultrasonography, including SWE and CEUS, for the differentiation of benign and malignant cervical lymphadenopathy.
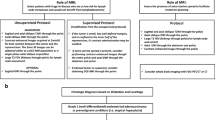
Methods
A total of 103 patients with 109 enlarged neck lymph nodes underwent SWE and CEUS. There were 25 hyperplastic lymph nodes, 66 metastatic lymph nodes, and 18 cases of lymphoma.
Results
Using 31.6 kPa as the Emax cutoff, the sensitivity, specificity and accuracy of measurements on both benign and malignant cervical lymph nodes were 55.95%, 96%, and 65.2%, respectively. CEUS showed that lymph nodes with reactive hyperplasia mainly exhibited uniform perfusion via the lymphatic hilum (18/25; 72%; P < 0.01). The main manifestation of lymphoma was uniform perfusion through the lymphatic hila (10/18; 55.6%; P < 0.01). Metastatic lymph nodes mainly exhibited uneven perfusion (57/66; 86.4%; P < 0.01). The sensitivity, specificity, and accuracy of multimodal ultrasonography for the diagnosis of benign and malignant cervical lymphadenopathies were 90.5%, 72%, and 86.2%, respectively.
Conclusions
Our findings suggest that multimodal ultrasonography can detect the stiffness (elasticity), perfusion pattern, and characteristics of lymph nodes and is a valuable tool for differentiating between benign and malignant lymphadenopathies.






Similar content being viewed by others
References
Gyorki DE, Boyle JO, Ganly I, Morris L, Shaha AR, Singh B, et al. Incidence and location of positive nonsentinel lymph nodes in head and neck melanoma. Eur J Surg Oncol. 2014;40:305–10.
Ying M, Ahuja A, Brook F. Accuracy of sonographic vascular features in differentiating causes of cervical lymphadenopathy. Ultrasound Med Biol. 2004;3:441–7.
Esen G. Ultrasound of superficial lymph nodes. Eur J Radiol. 2006;58:345–59.
Taylor K, O’Keeffe S, Britton PD, Wallis MG, Treece GM, Housden J, et al. Ultrasound elastography as an adjuvant to conventional ultrasound in the preoperative assessment of axillary lymph nodes in suspected breast cancer: a pilot study. Clin Radiol. 2011;66:1064–71.
Ahuja AT, Ying M, King A, Yuen HY. Lymph node hilus: gray scale and power Doppler sonography of cervical nodes. J Ultrasound Med. 2001;20:987–92.
Tschammler A, Ott G, Schang T, Seelbach-Goebel B, Schwager K, Hahn D. Lymphadenopathy: differentiation of benign from malignant disease—color Doppler ultrasound assessment of intranodal angioarchitecture. Radiology. 1998;208:117–23.
Kwak JY, Han KH, Yoon JH, Moon HJ, Son EJ, Park SH, et al. Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology. 2011;260:892–9.
Dudea SM, Lenghel M, Botar-Jid C, Vasilescu D, Duma M. Ultrasonography of superficial lymph nodes: benign vs. malignant. Med Ultrason. 2012;14:294–306.
Cui XW, Jenssen C, Saftoiu A, Ignee A, Dietrich CF. New ultrasound techniques for lymph node evaluation. World J Gastroenterol. 2013;19:4850–60.
Park CH, Song CM, Ji YB, Pyo JY, Yi KJ, Song YS, et al. Significance of the extracapsular spread of metastatic lymph nodes in papillary thyroid carcinoma. Clin Exp Otorhinolaryngol. 2015;8:289–94.
Ahuja AT, Ying M. Sonographic evaluation of cervical lymph nodes. Am J Roentgenol. 2005;184:1691–9.
Moritz JD, Ludwig A, Oestmann JW. Contrast-enhanced color Doppler sonography for evaluation of enlarged cervical lymph nodes in head and neck tumors. Am J Roentgenol. 2000;174:1279–84.
Yu M, Liu Q, Song HP, Han ZH, Su HL, He GB, et al. Clinical application of contrast enhanced ultrasonography in diagnosis of superficial lymphadenopathy. J Ultrasound Med. 2010;29:735–40.
Moritz JD, Ludwig A, Oestmann JW. Contrast-enhanced color Doppler sonography for evaluation of enlarged cervical lymph nodes in head and neck tumors. AJR Am J Roentgenol. 2000;174:1279–84.
Bercoff J, Tanter M, Fink M. Supersonic shear imaging: a new technique for soft tissue elasticity mapping. IEEE Trans Ultrason Ferroelectr Freq Control. 2004;51:396–409.
Alam F, Naito K, Horiguchi J, Fukuda H, Tachikake T, Ito K. Accuracy of sonographic elastography in the differential diagnosis of enlarged cervical lymph nodes: comparison with conventional B-mode sonography. AJR Am J Roentgenol. 2008;191:604–10.
Bhatia KS, Cho CC, Tong CS, Yuen EH, Ahuja AT. Shear wave elasticity imaging of cervical lymph nodes. Ultrasound Med Biol. 2012;38:195–201.
Bhatia K, Tong CS, Cho CC, Yuen EH, Lee J, Ahuja AT. Reliability of shear wave ultrasound elastography for neck lesions identified in routine clinical practice. Ultraschall Med. 2012;33:463–8.
Lyshchik A, Higashi T, Asato R, Tanaka S, Ito J, Hiraoka M, et al. Cervical lymph node metastases: diagnosis at sonoelastography—initial experience. Radiology. 2007;243:258–67.
Das D, Gupta M, Kaur H, Kalucha A. Elastography: the next step. J Oral Sci. 2011;53:137–41.
Hong Y-R, Luo Z-Y, Mo G-Q, Wang P, Ye Q, Huang P-T. Role of contrast-enhanced ultrasound in the pre-perative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma. Ultrasound Med Biol. 2017;43:2567–75.
Ito Y, Fukushima M, Higashiyama T, Kihara M, Takamura Y, Kobayashi K, et al. Tumor size is the strongest predictor of microscopic lymph node metastasis and lymph node recurrence of N0 papillary thyroid carcinoma. Endocr J. 2013;60:113–7.
Kim SS, Lee BJ, Lee JC, Kim SJ, Lee SH, Jeon YK, et al. Preoperative ultrasonographic tumor characteristics as a predictive factor of tumor stage in papillary thyroid carcinoma. Head Neck. 2011;33:1719–26.
Dewall RJ. Ultrasound elastography: principles, techniques, and clinical applications. Crit Rev Biomed Eng. 2013;41:1–19.
Suh CH, Choi YJ, Baek JH, Lee JH. The diagnostic performance of shear wave elastography for malignant cervical lymph nodes: a systematic review and meta-analysis. Eur Radiol. 2017;27:222–30.
Desmots F, Fakhry N, Mancini J, Reyre A, Vidal V, Jacquier A, et al. Shear wave elastography in head and neck lymph node assessment: image quality and diagnostic impact compared with B-mode and Doppler ultrasonography. Ultrasound Med Biol. 2016;42:387–98.
Poanta L, Serban O, Pascu I, Pop S, Cosgarea M, Fodor D. The place of CEUS in distinguishing benign from malignant cervical lymph nodes: a prospective study. Med Ultrason. 2014;16:7–14.
Xiang D, Hong Y, Zhang B, Huang P, Li G, Wang P, et al. Contrast-enhanced ultrasound (CEUS) facilitated US in detecting lateral neck lymph node metastasis of thyroid cancer patients: diagnosis value and enhancement patterns of malignant lymph nodes. Eur Radiol. 2014;24:2513–9.
Slaisova R, Benda K, Jarkovsky J, Petrasova H, Szturz P, Valek V. Contrast-enhanced ultrasonography compared to gray-scale and power Doppler in the diagnosis of peripheral lymphadenopathy. Eur J Radiol. 2013;82:693–8.
Rubaltelli L, Corradin S, Dorigo A, Tregnaghi A, Adami F, Rossi CR. Automated quantitative evaluation of lymph node perfusion on contrast-enhanced sonography. AJR Am J Roentgenol. 2007;188:977–83.
Rubaltelli L, Beltrame V, Tregnaghi A, Scagliori E, Frigo AC, Stramare R. Contrast-enhanced ultrasound for characterizing lymph nodes with focal cortical thickening in patients with cutaneous melanoma. AJR Am J Roentgenol. 2011;196:W8-12.
Zenk J, Bozzato A, Steinhart H, Greess H, Iro H. Metastatic and inflammatory cervical lymph nodes as analyzed by contrast-enhanced color-coded Doppler ultrasonography: quantitative dynamic perfusion patterns and histopathologic correlation. Ann Otol Rhinol Laryngol. 2005;114:43–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Yang, JR., Song, Y., Jia, YL. et al. Application of multimodal ultrasonography for differentiating benign and malignant cervical lymphadenopathy. Jpn J Radiol 39, 938–945 (2021). https://doi.org/10.1007/s11604-021-01131-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-021-01131-7