Abstract
Purpose
To determine the prevalence and degree of aortic dilatation (Adilatation), severity of aortic stiffness (Astiff), factors for Adilatation, and level of aortic root most sensitive to Astiff in patients with repaired tetralogy of Fallot (rTOF).
Materials and methods
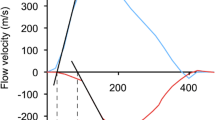
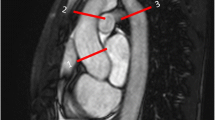
269 patients with rTOF (mean age 14.9 ± standard deviation 5.0 years) were analyzed for Adilatation at annulus, sinus, sinotubular junction, and ascending aorta (aAo). Aortic size index was graded as Z score < 2, 2–2.99, 3–4.99 and ≥ 5. Aortic distensibility (aAdis) was categorized according to 4 aortic levels and dilatation severity. Factors for Adilatation and level of aortic root most sensitive to Astiff were analyzed.
Results
Sinus and aAo were the two most common sites of Adilatation, with a prevalence of 84% and 76%, respectively. A decreased aAdis was found (mean 5.38 ± 1.79 10−3 mmHg−1). aAdis only declined significantly at the sinus level (p = 0.009). Male sex, age-at-repair and aortic regurgitation were significant factors for Adilatation, with male sex as the strongest factor (odds ratio 2.94). There was a significant decline in aAdis at sinus level (p = 0.002) as Adilatation progressed.
Conclusions
We observed a high prevalence of Adilatation and Astiff in patients with rTOF. Male sex is the strongest factor for Adilatation. The sinus is the most sensitive area for determining a negative aAdis effect.



Similar content being viewed by others
Abbreviations
- aAo:
-
Ascending aorta
- aA dis :
-
Aortic distensibility
- A stiff :
-
Aortic stiffness
- aAomax-area :
-
Maximal ascending aortic luminal areas
- aAomin-area :
-
Minimal ascending aortic luminal areas
- A dilatation :
-
Aortic dilatation
- bSSFP:
-
Balanced steady-state free precession
- LVEF:
-
Left ventricular ejection fraction
- LVOT:
-
Left ventricular outflow tract
- MRI:
-
Magnetic resonance imaging
- PC-VENC:
-
Phase contrast velocity encoded
- RF:
-
Regurgitation fraction
- rTOF:
-
Repaired tetralogy of Fallot
- STJ:
-
Sinotubular junction
- TOF:
-
Tetralogy of Fallot
References
Chowdhury UK, Mishra AK, Ray R, Kalaivani M, Reddy SM, Venugopal P. Histopathologic changes in ascending aorta and risk factors related to histopathologic conditions and aortic dilatation in patients with tetralogy of Fallot. J Thorac Cardiovasc Surg. 2008;135(1):69–77. https://doi.org/10.1016/j.jtcvs.2007.06.011.
Tan JL, Davlouros PA, McCarthy KP, Gatzoulis MA, Ho SY. Intrinsic histological abnormalities of aortic root and ascending aorta in tetralogy of Fallot: evidence of causative mechanism for aortic dilatation and aortopathy. Circulation. 2005;112(7):961–8. https://doi.org/10.1161/CIRCULATIONAHA.105.537928.
Niwa K, Perloff JK, Bhuta SM, Laks H, Drinkwater DC, Child JS, Miner PD. Structural abnormalities of great arterial walls in congenital heart disease: light and electron microscopic analyses. Circulation. 2001;103(3):393–400. https://doi.org/10.1161/01.CIR.103.3.393.
Chong WY, Wong WHS, Chiu CSW, Cheung YF. Aortic root dilatation and aortic elastic properties in children after repair tetralogy of Fallot. Am J Cardiol. 2006;97(6):905–9. https://doi.org/10.1016/j.amjcard.2005.09.141.
Niwa K, Siu SC, Webb GD, Gatzoulis MA. Progressive aortic root dilatation in adults late after repair of tetralogy of Fallot. Circulation. 2002;106(11):1374–8. https://doi.org/10.1161/01.CIR.0000028462.88597.AD.
Mongeon FP, Gurvitz MZ, Broberg CS, Aboulhosn J, Opotowsky AR, Kay JD, et al. Aortic root dilatation in adults with surgically repaired tetralogy of Fallot. A multicenter cross-sectional study. Circulation. 2013;127(2):172–9. https://doi.org/10.1161/CIRCULATIONAHA.112.129585.
Burman ED, Keegan J, Kilner PJ. Aortic root measurement by cardiovascular magnetic resonance. Specification of planes and lines of measurement and corresponding normal values. Circ Cardiovasc Imaging. 2008;1(2):104–13. https://doi.org/10.1161/CIRCIMAGING.108.768911.
Grotenhuis HB, Dallaire F, Verpalen IM, van den Akker MJE, Mertens L, Friedberg MK. Aortic root dilatation and aortic-related complications in children after tetralogy of Fallot repair. Circ Cardiovasc Imaging. 2018;11(12):e007611. https://doi.org/10.1161/CIRCIMAGING.118.007611.
Sluysmans T, Colan SD. Structural measurements and adjustment for growth. In: Lai WW, Cohen MS, Geva T, Mertens L, editors. Echocardiography in pediatric and congenital heart disease. 1st ed. West Sussex: Wiley-Blackwell; 2009. p. 51–62.
Colan SD. Normal echocardiographic values for cardiovascular structures. In: Lai WW, Cohen MS, Geva T, Mertens L, editors. Echocardiography in pediatric and congenital heart disease. 1st ed. West Sussex: Wiley-Blackwell; 2009. p. 765–85.
McMahon CJ, Ravekes WJ, Smith EO, Denfield SW, Pignatelli RH, Altman CA, et al. Risk factors for neo-aortic root enlargement and aortic regurgitation following arterial switch operation. Pediatr Cardiol. 2004;25(4):329–35. https://doi.org/10.1007/s00246-003-0483-6.
Voges I, Jerosch-Herold M, Hedderich J, Pardun E, Hart C, Gabbert DD, et al. Normal values of aortic dimensions, distensibility, and pulse wave velocity in children and young adults: a cross-sectional study. J Cardiovasc Magn Reson. 2012;14(1):77. https://doi.org/10.1186/1532-429X-14-77.
Enriquez-Sarano M, Tajik AJ. Aortic regurgitation. N Engl J Med. 2004;351:1539–46. https://doi.org/10.1056/NEJMcp030912.
Burman ED, Keegan J, Kilner PJ. Aortic root measurement by cardiovascular magnetic resonance: specification of planes and lines of measurement and corresponding normal values. Circ Cardiovasc Imaging. 2008;1(2):104–13. https://doi.org/10.1161/CIRCIMAGING.108.768911.
Francois K, Zaqout M, Bové T, Vandekerckhove K, De Groote K, Panzer J, et al. The fate of the aortic root after early repair of tetralogy of Fallot. Eur J Cardio Thoracic Surg. 2010;37(6):1254–8. https://doi.org/10.1016/j.ejcts.2009.12.019.
Francois K, Creytens D, De Groote K, Panzer J, Vandekerckhove K, De Wolf D, et al. Analysis of the aortic root in patients with tetralogy of Fallot undergoing early repair: form follows function. J Thoracic Cardiovasc Surg. 2014;148(4):1555–9. https://doi.org/10.1016/j/t.cvs2013.11.044.
Radonic T, de Witte P, Groenink M, de Bruin-Bon RACM, Timmermans J, Scholte AJH, et al. Critical appraisal of the revised Ghent criteria for diagnosis of Marfan syndrome. Clin Genet. 2011;8(4):346–53. https://doi.org/10.1111/j.1399-0004.2011.01646.x.
Hager A, Kaemmerer H, Rapp-Bernhardt U, Blücher S, Rapp K, Bernhardt TM, et al. Diameters of the thoracic aorta throughout life as measured with helical computed tomography. J Thorac Cardiovasc Surg. 2002;123(6):1060–6. https://doi.org/10.1067/mtc.2002.122310.
Aburawi EH, O’Sullivan J. Relation of aortic root dilatation and age in Marfan’s syndrome. Eur Heart J. 2007;28(3):376–9. https://doi.org/10.1093/eurheartj/ehl457.
Takei K, Murakami T, Takeda A. Implication of aortic root dilatation and stiffening in patients with tetralogy of Fallot. Pediatr Cardiol. 2018;39(7):1462–7. https://doi.org/10.1007/s00246-018-1917-5.
Glukhova MA, Frid MG, Koteliansky VE. Phenotypic changes of human aortic smooth muscle cells during development and in the adult vessel. Am J Physiol. 1991;261(4 suppl):78–80. https://doi.org/10.1152/ajpheart.1991.261.4.78.
Martyn CN, Greenwald SE. Impaired synthesis of elastin in walls of aorta and large conduit arteries during early development as an initiating event in pathogenesis of systemic hypertension. Lancet. 1997;350(9082):953–5. https://doi.org/10.1016/s0140-6736(96)10508-0.
Niwa K. Aortic dilatation in complex congenital heart disease. Cardiovasc Diagn Ther. 2018;8(6):725–38. https://doi.org/10.21037/cdt.2018.12.05
Rieker RP, Berman MA, Stansel HC Jr. Postoperative studies in patients with tetralogy of Fallot. Ann Thorac Surg. 1975;19(1):17–26. https://doi.org/10.1016/S003-4975(10)65727-X.
Azadani AN, Chitsaz S, Matthews PB, Jaussaud N, Leung J, Tsinman T, et al. Comparison of mechanical properties of human ascending aorta and aortic sinuses. Am J Thorac Surg. 2012;93(1):87–94. https://doi.org/10.1016/j.athoracsur.2011.08.002.
Christensen JT, Lu JC, Donohue J, Yu S, Mahani MG, Agarwal PP, et al. Relation of aortic stiffness and strain by cardiovascular magnetic resonance imaging to age in repaired tetralogy of Fallot. Am J cardiol. 2014;113(6):1031–5. https://doi.org/10.1016/j.amjcard.2013.11.067.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical statement
All procedures performed in these studies were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the institutional Human Research Ethics Committee, Faculty of Medicine, Ramathibodi Hospital, Mahidol University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Siripornpitak, S., Sriprachyakul, A., Wongmetta, S. et al. Magnetic resonance imaging assessment of aortic dilatation and distensibility in 269 patients with repaired tetralogy of Fallot. Jpn J Radiol 39, 774–782 (2021). https://doi.org/10.1007/s11604-021-01119-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-021-01119-3