Abstract
Purpose
The aim of the study was to investigate the diagnostic accuracy of peri-thrombus vascular hyperintensity sign (PVHS) on three-dimensional (3D) black-blood (BB) contrast-enhanced MRI for the detection of intracranial thrombus location and length in acute ischemic stroke (AIS) patients.
Materials and methods
Consecutive AIS patients who underwent MRI including 3D BB contrast-enhanced MRI sequence within 8 h of clinical onset were prospectively evaluated. Two readers independently reviewed the 3D BB contrast-enhanced MRI data to assess the presence and location of PVHS. Findings were compared with those of contrast-enhanced MR angiography (CE-MRA) as the reference standard.
Results
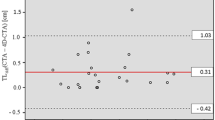
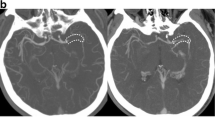
The PVHS was identified in 49% (63/129) of AIS patients with good agreement. The PVHS had 100% specificity, 88% negative predictive value, 89% sensitivity, and 100% positive predictive value for detection of acute arterial occlusions. Eight patients showed discordant thrombus locations between 3D BB contrast-enhanced MRI and CE-MRA. Median thrombus length in patients with complete occlusion was 9.61 mm.
Conclusion
The PVHS on 3D BB contrast-enhanced MRI is a highly specific tool for evaluating the location and length of a thrombus in AIS patients.





Similar content being viewed by others
References
Powers WJ, Derdeyn CP, Biller J, et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46(10):3020–35.
Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–31.
Borst J, Berkhemer OA, Santos EMM, et al. Value of thrombus CT characteristics in patients with acute ischemic stroke. Am J Neuroradiol. 2017;38(9):1758–64.
Saver JL, Goyal M, van der Lugt A, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016;316(12):1279.
Le Bras A, Raoult H, Ferré JC, Ronzière T, Gauvrit JY. Optimal MRI sequence for identifying occlusion location in acute stroke: which value of time-resolved contrast-enhanced MRA? Am J Neuroradiol. 2015;36(6):1081–8.
Stock KW, Wetzel S, Kirsch E, Bongartz G, Steinbrich W, Radue EW. Anatomic evaluation of the circle of Willis: MR angiography versus intraarterial digital subtraction angiography. AJNR Am J Neuroradiol. 1996;17(8):1495–9.
Diouf A, Fahed R, Gaha M, et al. Cervical internal carotid occlusion versus pseudo-occlusion at CT angiography in the context of acute stroke: an accuracy, interobserver, and intraobserver agreement study. Radiology. 2018;286(3):1008–155.
Boujan T, Neuberger U, Pfaff J, et al. Value of contrast-enhanced MRA versus time-of-flight MRA in acute ischemic stroke MRI. AJNR Am J Neuroradiol. 2018;39(9):1710–6.
Chen Z, Zhang M, Shi F, et al. Pseudo-occlusion of the internal carotid artery predicts poor outcome after reperfusion therapy. Stroke. 2018;49(5):1204–9.
Park M, Oh S, Baik SK, Jung DS, Park K. Susceptibility-weighted imaging for detection of thrombus in acute cardioembolic stroke. J Stroke. 2016;18(1):73–9.
Liebeskind DS, Sanossian N, Yong WH, et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke. 2011;42(5):1237–43.
Rovira A, Orellana P, Alvarez-Sabín J, et al. Hyperacute ischemic stroke: middle cerebral artery susceptibility sign at echo-planar gradient-echo MR imaging. Radiology. 2004;232(2):466.
Flacke S, Urbach H, Keller E, et al. Middle cerebral artery (MCA) susceptibility sign at susceptibility-based perfusion MR imaging: clinical importance and comparison with hyperdense MCA sign at CT. Radiology. 2000;215(2):476.
Lindenholz A, van der Kolk AG, Zwanenburg JJM, Hendrikse J. The use and pitfalls of intracranial vessel wall imaging: how we do it. Radiology. 2018;286(1):12–28.
Mandell DM, Mossa-Basha M, Qiao Y, et al. Intracranial vessel wall MRI: principles and expert consensus recommendations of the American Society of Neuroradiology. Am J Neuroradiol. 2017;38(2):218–29.
Mossa-Basha M, Shibata DK, Hallam DK, et al. Added value of vessel wall magnetic resonance imaging for differentiation of nonocclusive intracranial vasculopathies. Stroke. 2017;48(11):3026–33.
Lee JS, Demchuk AM. Choosing a hyperacute stroke imaging protocol for proper patient selection and time efficient endovascular treatment: lessons from recent trials. J Stroke. 2015;17(3):221–8.
Renú A, Laredo C, Lopez-Rueda A, et al. Vessel wall enhancement and blood-cerebrospinal fluid barrier disruption after mechanical thrombectomy in acute ischemic stroke. Stroke. 2017;48(3):651–7.
Niu P, Yu Y, Zhou H, et al. Vessel wall differences between middle cerebral artery and basilar artery plaques on magnetic resonance imaging. Sci Rep UK. 2016;6(1):38534.
Jang W, Kwak HS, Chung GH, Hwang SB. Three-dimensional black-blood contrast-enhanced MRI improves detection of intraluminal thrombi in patients with acute ischaemic stroke. Eur Radiol. 2018;28(9):3840–7.
Obara M, Kuroda K, Wang J, et al. Comparison between two types of improved motion-sensitized driven-equilibrium (iMSDE) for intracranial black-blood imaging at 3.0 tesla. J Magn Reson Imaging. 2014;40(4):824–31.
Grossberg JA, Haussen DC, Cardoso FB, et al. Cervical carotid pseudo-occlusions and false dissections. Stroke. 2017;48(3):774–7.
Korn A, Bender B, Brodoefel H, et al. Grading of carotid artery stenosis in the presence of extensive calcifications: dual-energy CT angiography in comparison with contrast-enhanced MR angiography. Clin Neuroradiol. 2015;25(1):33–40.
Funding
This study was supported in part by the National Natural Science Foundation of China (No. 81601459).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The protocol of this study was reviewed and approved by our Institutional Ethics Committee. All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Chen, Q., Wang, W., Chen, YC. et al. Peri-thrombus vascular hyperintensity sign: detection of intracranial thrombus location and length in acute ischemic stroke. Jpn J Radiol 38, 516–523 (2020). https://doi.org/10.1007/s11604-020-00937-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-020-00937-1