Abstract
Objective
This study aimed to compare the clinical effects of double ovulation stimulation (DouStim) applied during the follicular and luteal phases with the antagonist protocol in patients with diminished ovarian reserve (DOR) and asynchronous follicular development undergoing assisted reproductive technology (ART).
Methods
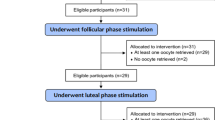
The clinical data of patients with DOR and asynchronous follicular development receiving ART from January 2020 to December 2021 were retrospectively analyzed. The patients were divided into two groups according to their ovulation stimulation protocol: DouStim group (n=30) and antagonist group (n=62). Assisted reproduction and clinical pregnancy outcomes were compared between the two groups.
Results
In the DouStim group, the number of oocytes retrieved, metaphase II (MII) oocytes, two-pronuclei (2PN), day 3 (D3) embryos, D3 high-quality embryos as well as blastocyst formation, implantation, and human chorionic gonadotropin-positive rates were significantly greater than those in the antagonist group (all P<0.05). No significant differences were found in MII, fertilization, or continued pregnancy rates at the first frozen embryo transfer (FET), in-vitro fertilization (IVF) cancellation, or early medical abortion rates between the groups (all P>0.05). Except for the early medical abortion rate, the DouStim group generally had favorable outcomes. In the DouStim group, the dosage and duration of gonadotropin and the fertilization rate were significantly greater in the first ovulation stimulation induction than in the second ovulation stimulation induction (P<0.05).
Conclusion
The DouStim protocol efficiently and economically obtained more mature oocytes and high-quality embryos for patients with DOR and asynchronous follicular development.
Similar content being viewed by others
References
Zhao X, Ma B, Mo S, et al. Improvement of pregnancy outcome by extending embryo culture in IVF-ET during clinical application. J Assist Reprod Genet, 2018,35(2):321–329
Wang R, Lin S, Wang Y, et al. Comparisons of GnRH antagonist protocol versus GnRH agonist long protocol in patients with normal ovarian reserve: A systematic review and meta-analysis. PLoS One, 2017,12(4):e0175985
Lambalk CB, Banga FR, Huirne JA, et al. GnRH antagonist versus long agonist protocols in IVF: a systematic review and meta-analysis accounting for patient type. Hum Reprod Update, 2017,23(5):560–579
Pereira N, Lekovich JP, Kligman I, et al. Severe ovarian hyperstimulation syndrome after combined GnRH-agonist and low-dose human chorionic gonadotropin trigger in a patient with a single kidney. Gynecol Endocrinol, 2017,33(8):593–597
Kuang Y, Chen Q, Hong Q, et al. Double stimulations during the follicular and luteal phases of poor responders in IVF/ICSI programmes (Shanghai protocol). Reprod Biomed Online, 2014,29(6):684–691
Kamath MS, Maheshwari A, Bhattacharya S, et al. Oral medications including clomiphene citrate or aromatase inhibitors with gonadotropins for controlled ovarian stimulation in women undergoing in vitro fertilisation. Cochrane Database Syst Rev, 2017,11(11):CD008528
Heijnen EM, Eijkemans MJ, De Klerk C, et al. A mild treatment strategy for in-vitro fertilisation: a randomised noninferiority trial. Lancet, 2007,369(9563):743–749
Ferraretti AP, La Marca A, Fauser BC, et al. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod, 2011,26(7):1616–1624
Wang N, Wang Y, Chen Q, et al. Luteal-phase ovarian stimulation vs conventional ovarian stimulation in patients with normal ovarian reserve treated for IVF: a large retrospective cohort study. Clin Endocrinol, 2016,84(5):720–728
Siristatidis C, Salamalekis G, Dafopoulos K, et al. Mild versus conventional ovarian stimulation for poor responders undergoing IVF/ICSI. In Vivo, 2017,31(2):231–237
Oktay K, Bedoschi G, Berkowitz K, et al. Fertility preservation in women with Turner syndrome: A comprehensive review and practical guidelines. J Pediatr Adolesc Gynecol, 2016,29(5):409–416
Humaidan P, Chin W, Rogoff D, et al. Efficacy and safety of follitropin alfa/lutropin alfa in ART: a randomized controlled trial in poor ovarian responders. Human Reprod, 2017,32(3):544–555
Chinese Medical Doctor Association Committee of Reproductive Medicine. Cumulative delivery/live birth rate of complete ovarian stimulation cycle consensus. Reprod Contracept (Chinese), 2018,38:963–968
Sfakianoudis K, Pantos K, Grigoriadis S, et al. What is the true place of a double stimulation and double oocyte retrieval in the same cycle for patients diagnosed with poor ovarian reserve? A systematic review including a meta-analytical approach. J Assist Reprod Genet, 2020,37(1):181–204
Vaiarelli A, Cimadomo D, Trabucco E, et al. Double stimulation in the same ovarian cycle (DouStim) to maximize the number of oocytes retrieved from poor prognosis patients: A multicenter experience and SWOT analysis. Front Endocrinol (Lausanne), 2018,14;9:317
Ubaldi FM, Capalbo A, Vaiarelli A, et al. Follicular versus luteal phase ovarian stimulation during the same menstrual cycle (DouStim) in a reduced ovarian reserve population results in a similar euploid blastocyst formation rate: new insight in ovarian reserve exploitation. Fertil Steril, 2016,105(6):1488–1495
Humaidan P, Papanikolaou EG, Kyrou D, et al. The luteal phase after GnRH-agonist triggering of ovulation: present and future perspectives. Reprod Biomed Online, 2012,24(2):134–141
Zhang Q, Guo XM, Li Y. Implantation rates subsequent to the transfer of embryos produced at different phases during double stimulation of poor ovarian responders. Reprod Fertil Dev, 2017,29(6):1178–1183
Zhang W, Wang M, Wang S, et al. Luteal phase ovarian stimulation for poor ovarian responders. JBRA Assist Reprod, 2018,22(3):193–198
Kol S, Humaidan P. LH (as HCG) and FSH surges for final oocyte maturation: sometimes it takes two to tango? Reprod Biomed Online, 2010,21(5):590–592
Humaidan P, Kol S, Papanikolaou EG. GnRH agonist for triggering of final oocyte maturation: time for a change of practice? Hum Reprod Update, 2011,17(4):510–524
Lamb JD, Shen S, McCulloch C, et al. Follicle-stimulating hormone administered at the time of human chorionic gonadotropin trigger improves oocyte developmental competence in in vitro fertilization cycles: a randomized, double-blind, placebo-controlled trial. Fertil Steril, 2011,95(5):1655–1660
Lu BJ, Lin CJ, Lin BZ, et al. ART outcomes following ovarian stimulation in the luteal phase: a systematic review and meta-analysis. J Assist Reprod Genet, 2021,38(8):1927–1938
Massin N. New stimulation protocol: endogenous and exogenous progesterone use to block the LH surge during ovarian stimulation for IVF. Hum Reprod Update, 2017,23(2):211–220
Boots CE, Meister M, Cooper AR, et al. Ovarian stimulation in the luteal phase: systematic review and meta-analysis. J Assist Reprod Genet, 2016,33(8):971–980
Evans MB, Parikh T, DeCherney AH, et al. Evaluation of the cost-effectiveness of ovulation suppression with progestins compared with GnRH analogs in assisted reproduction cycles. Reprod Biomed Online, 2019,38(5):691–698
Acknowledgments
We wish to acknowledge the support of the Chinese PLA General Hospital. We would also like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of Interest Statement
The authors declare that they have no conflicts of interest.
This study was supported by a Chinese Military family planning project grant (No. 17JS014).
Rights and permissions
About this article
Cite this article
Yang, Yz., Zhang, M., Mu, S. et al. Clinical Application of Double Ovulation Stimulation in Patients with Diminished Ovarian Reserve and Asynchronous Follicular Development Undergoing Assisted Reproduction Technology. CURR MED SCI 43, 304–312 (2023). https://doi.org/10.1007/s11596-022-2687-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-022-2687-0