Summary
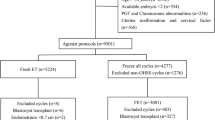
The clinical outcomes of five groups of infertility patients receiving frozen-thawed, cleavage-stage embryo transfers with exogenous hormone protocols with or without a depot gonadotropin-releasing hormone (GnRH) agonist were assessed. A retrospective cohort analysis was performed on 1003 cycles undergoing frozen-thawed, cleavage-stage embryo transfers from January 1, 2012 to June 31, 2015 in the Reproductive Medicine Center of Wuhan General Hospital of Guangzhou Military Region. Based on the infertility etiologies of the patients, the 1003 cycles were divided into five groups: tubal infertility, polycystic ovary syndrome (PCOS), endometriosis, male infertility, and unexplained infertility. The main outcome was the live birth rate. Two groups were set up based on the intervention: group A was given a GnRH agonist with exogenous estrogen and progesterone, and group B (control group) was given exogenous estrogen and progesterone only. The results showed that the baseline serum hormone levels and basic characteristics of the patients were not significantly different between groups A and B. The live birth rates in groups A and B were 41.67% and 29.29%, respectively (P<0.05). The live birth rates in patients with PCOS in groups A and B were 56.25% and 30.61%,respectively (P<0.05). The clinical pregnancy, implantation and on-going pregnancy rates showed the same trends as the live birth rates between groups A and B. The ectopic pregnancy rate was significantly lower in group A than in group B. We concluded that the live birth rate was higher and other clinical outcomes were more satisfactory with GnRH agonist cotreatment than without GnRH agonist co-treatment for frozen-thawed embryo transfer. The GnRH agonist combined with exogenous estrogen and progesterone worked for all types of infertility tested, especially for women with PCOS.
Similar content being viewed by others
References
Roque M, Lattes ?, Serra S, et al. Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and metaanalysis. Fertil Steril, 2013, 99(1):156–162
Weinerman R, Mainigi M. Why we should transfer frozen instead of fresh embryos: the translational rationale. Fertil Steril, 2014, 02(1):10–18
Devroey P, Polyzos NP, Blockeel C. An OHSSFree Clinic by segmentation of IVF treatment. Hum Reprod, 2011, 26(10):2593–2597
Roque M. Freeze-all policy: is it time for that? J Assist Reprod Genet, 2015, 32(2):171–176
Shapiro BS, Daneshmand ST, Gamer FC, et al. Freeze-all at the blastocyst or bipronuclear stage: a randomized clinical trial. Fertil Steril, 2015, 104(5):1138–1144
Glujovsky D, Pesce R, Fiszbajn G, et al. Endometrial preparation for women undergoing embryo transfer with frozen embryos or embryos derived from donor oocytes. Cochrane Database Syst Rev, 2010, 1:CD006359
Groenewoud ER, Cantineau AE, Köllen BJ, et al. What is the optimal means of preparing the endometrium in frozen-thawed embryo transfer cycles? A systematic review and meta-analysis. Hum Reprod Update, 2013, 9(5):458–470
Ma WG, Song H, Das SK, et al. Estrogen is a critical determinant that specifies the duration of the window of uterine receptivity for implantation. Proc Natl Acad Sei, 2003, 4, 100(5):2963–2968
Raga F, Casan EM, Kruessel JS, et al. Quantitative gonadotropin-releasing hormone gene expression and immunohistochemical localization in human endometrium throughout the menstrual cycle. Biol Reprod, 1998, 59(3):661–669
Khan KN, Kitajima M, Hiraki K, et al Cell proliferation effect of GnRH agonist on pathological lesions of women with endometriosis, adenomyosis and uterine myoma. Hum Repród, 2010, 25:2878–2890
Muasher SJ, Kruithoff C, Simonetti S, et al. Controlled preparation of the endometrium with exogenous steroids for the transfer of frozen-thawed pre-embryos in patients with anovulatory or irregular cycles. Hum Reprod, 1991, 6(3):443–445
Hill MJ, Miller KA, Frattarelli JL. A GnRH agonist and exogenous hormone stimulation protocol has a higher live-birth rate than a natural endogenous hormone protocol for frozen-thawed blastocyst-stage embryo transfer cycles: an analysis of 1391 cycles. Fertil Steril, 2010, 93(2):416–422
Dal Prato L, Borini A, Cattoli M, et al. Endometrial preparation for frozen-thawed embryo transfer with or without pretreatment with gonadotropin-releasing hormone agonist. Fertil Steril, 2002, 77(5):956–960
van de Vijver A, Polyzos NP, Van Landuyt L, et al. Cryopreserved embryo transfer in an artificial cycle: is GnRH agonist down-regulation necessary? Reprod Biomed Online, 2014, 29(5):588–594
AzimiNekoo E, Chamani M, Shahrokh Tehrani E, et al. Artificial Endometrial Preparation for Frozen-Thawed Embryo Transfer with or without Pretreatment with Depot Gonadotropin Releasing Hormone Agonist in Women with Regular Menses. J Family Reprod Health, 2015, 9(1):l–4
Broekmans FJ, Bernardus RE, Berkhout G, et al. Pituitary and ovarian suppression after early follicular and mid-luteal administration of a LHRH agonist in a depot formulation: decapeptyl CR. Gynecol Endocrinol, 1992, 6(3):153–161
Iwashita M, Kudo Y, Shinozaki Y, et al. Gonadotropinreleasing hormone increases serum human chorionic gonadotropin in pregnant women. Endoer J, 1993, 40(5):539–544
Casan EM, Raga F, Polan ML. GnRH mRNA and protein expression in human preimplantation embryos. Mol Hum Reprod, 1999, 5(3):234–239
De Leo V, Musacchio MC, Cappelli V, et al. Genetic, hormonal and metabolic aspects of PCOS: an update. Reprod Biol Endocrinol, 2016, 14(1):38
Yu J, Ma Y, Wu Z, et al. Endometrial preparation protocol of the frozen-thawed embryo transfer in patients with polycystic ovary syndrome. Arch Gynecol Obstet, 2015, 291(1):201–211
Gong F, Li X, Zhang S, et al. A modified ultralong pituitary downregulation protocol improved endometrial receptivity and clinical outcome for infertile patients with polycystic ovarian syndrome. Exp Ther Med, 2015, 10(5):1865–1870
Refaat B, Dalton E, Ledger WL. Ectopic pregnancy secondary to in vitro fertilisation-embryo transfer: pathogenic mechanisms and management strategies. Reprod Biol Endocrinol, 2015, 13:30
Shao R, Feng Y, Zou S, et al. The role of estrogen in the pathophysiology of tubal ectopic pregnancy. Am J Transi Res, 2012, 4(3):269–278
Zhu L, Li Y, Xu A. Influence of controlled ovarian hyper-stimulation on uterine peristalsis in infertile women. Hum Reprod, 2012, 27(9):2684–2689
Rickes D, Nickel I, Kropf S, etal. Increased pregnancy rates after ultralong postoperative therapy with gonadotropin releasing hormone analogs in patients with endometriosis. Fertil Steril, 2002, 78(4):757–762
Sallam HN, Garcia-Velasco JA, Arici A. Long-term pituitary down-regulation before in vitro fertilization (IVF) for women with endometriosis (Protocol). Cochrane Database Syst Rev, 2006, 1:CD004635
Franasiak JM, Holoch KJ, Yuan L, et al. Prospective assessment of midsecretory endometrial leukemia inhibitor factor expression versus avβ3 testing in women with unexplained infertility. Fertil Steril, 2014, 101(6):1724–1731
Yang X, Huang R, Wang YF, et al. Pituitary suppression before frozen embryo transfer is beneficial for patients suffering from idiopathic repeated implantation failure. J Huazhong Univ Sei Technolog Med Sei, 2016, 36(1):127–131
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by the Wu JiePing Medical Foundation (No. 320.6755.15032) and the Wuhan Science and Technology Project (No. 2016060101010030).
Rights and permissions
About this article
Cite this article
Xie, D., Chen, F., Xie, Sz. et al. Artificial Cycle with or without a Depot Gonadotropin-releasing Hormone Agonist for Frozen-thawed Embryo Transfer: An Assessment of Infertility Type that Is Most Suitable. CURR MED SCI 38, 626–631 (2018). https://doi.org/10.1007/s11596-018-1923-0
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-018-1923-0