Abstract
Purpose
The deep circumflex iliac crest flap (DCIA) is used for the reconstruction of the jaw. For fitting of the transplant by computer-aided planning (CAD), a computerized tomography (CT) of the jaw and the pelvis is necessary. Ready-made cutting guides save a pelvic CT and healthcare resources while maintaining the advantages of the CAD planning.
Methods
A total of 2000 CTs of the pelvis were divided into groups of 500 by sex and age (≤ 45 and > 45 years). Three-dimensional (3D) pelvis models were aligned and averaged. Cutting guides were designed on the averaged pelvis for each group and an overall averaged pelvis. The cutting guides and 50 randomly selected iliac crests (10 from each group and 10 from the whole collective) were 3D printed. The appropriate cutting guide was mounted to the iliac crest and a cone beam CT was performed. The thickness of the space between the iliac crest and the cutting guide was evaluated.
Results
Overall the mean thickness of the space was 2.137 mm and the mean volume of the space was 4513 mm3. The measured values were significantly different between the different groups. The overall averaged group had not the greatest volume, maximum thickness and mean thickness of the space.
Conclusion
Ready-made cutting guides for the DCIA flap fit to the iliac crest and make quick and accurate flap raising possible while radiation dose and resources can be saved. The cutting guides fit sufficient to the iliac crest and should keep the advantages of a standard CAD planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Squamous cell carcinoma of the head and neck (HNSCC) is a common form of cancer with an increasing incidence [1]. For small HNSCC in the oral cavity without metastasis in the lymphatic nodes, the surgical resection can achieve a cure rate of up to 80% [2]. Even for larger tumors, surgical resection is chosen as a treatment in combination with radiation and systemic therapy. In advanced cases, the ablation of the jaw bone is necessary in curative treatment. However, large benign tumors, extensive necrosis of the jaw or trauma can also lead to the loss of a large part of the jaw. This leaves the patients with reduced quality of life [3].
After ablative surgery of the jaw, the bony reconstruction using microvascular bone flaps is the gold standard in the literature [4]. The deep circumflex iliac crest (DCIA) flap is commonly used for the reconstruction of the jaw and following dental prosthetic rehabilitation using enosseous dental implants [5, 6].
The pelvis is a central bone in the human body. It is crucial in human locomotion and for obstetrics [7]. It is a bone with huge dimorphism and growth between males and females [8]. This results in many different morphologies of the pelvis and consequently the iliac crest. Currently, for exact placement and size of the DCIA flap computer-aided planning (CAD) is regularly used prior to surgery [9].
For CAD planning, a computerized tomography (CT) of the jaw and the pelvis is necessary [10, 11]. The CT of the jaw is necessary for measuring the bony defect and the placement of the later DCIA flap. The CT of the pelvis is necessary for the design of the transplant and the cutting guides for harvesting the DCIA flap. However, the price for the higher accuracy achievable with CAD planning is a high radiation dose for the patient. The dose of a head CT is 1–2 mSv and the dose of a pelvis CT accumulates to 3–4 mSv [12]. If the advantages of the CAD planning could be obtained without the necessity of a pelvis CT, the patients’ dose could be reduced about 75%. In addition, the cost of computerized-planning is high, making it difficult to use in societies with less well-funded healthcare systems. A ready-made cutting guide with predefined outlines that fits to the donor bone and can easily be customized in its’ extensions could reduce the cost significantly. No standard CAD planning is carried out, as the cutting guides are not planned on the individual iliac crest but a universal guide is used to assist raising the DCIA flap. Nevertheless, the extent of the cutting guide will be digitally adjusted preoperatively to the defect of the jaw to be reconstructed.
The anatomy of the nourishing vessels of the DCIA flap is well known and recent publications show no severe stenosis by atherosclerosis [13]. Therefore, a CT scan is only necessary to obtain the anatomy of the iliac crest to create the cutting guide.
In every day clinical practice, numerous CT scans of the pelvis are performed for several reasons. Due to legal reasons, the pictures have to be archived and create a huge amount of data that can be used for a secondary purpose. Following the trend of big data in medicine, the data could enable to create average models of the pelvis for designing cutting guides for the iliac crest that fit to nearly every iliac crest.
Therefore, it was hypothesized that a ready-made cutting guide for the iliac crest could be developed from the data, making a pelvic CT unnecessary before DCIA flap harvest.
Materials and methods
After institutional approval (EK 260/20) of the local ethics committee, the local picture archiving and communication system was searched for CT examinations including the complete pelvis. Exclusion criteria were as follows: artifacts, fractures, implants, obvious deformities. A total number of 2000 CT scans were downloaded. From these 500 CT scans were grouped in each group divided for gender and age. For females and males, there were two groups each. One group consisted of patients from 18 to 45 years (YF: females ≤ 45 years; YM: males ≤ 45 years) and the other consisted of patients from 46 to 99 years (OF: females > 45 years; OM: males > 45 years). In addition, there was a universal group (UNIV) in which all 2000 CT scans were. The division into groups according to sex is based on the sexual dimorphism of the pelvis [14]. A division by age was necessary because of the different growth patterns of the pelvis before and after menopause [8]. The data was saved as digital imaging and communications in medicine (DICOM) files.
Segmentation
The DICOM files of each examination were imported into ProPlan CMF version 3.0.1 (Materialise, Leuven, Belgium). In this software, the DICOM images were segmented and converted into three-dimensional (3D) models of the pelvis. Therefore, the spine was cut above the Os sacrum and the femur was removed from the pelvis model. After segmentation, the model was saved as a standard tessellation language (STL) file.
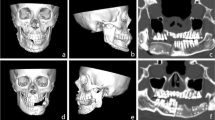
Definition of a generalizable topology
As all geometrical models stored in STL files are arbitrarily meshed, a direct geometrical relation that allows statistical evaluation is not possible. Hence, it was necessary to define a mesh topology that can be individualized to represent the different geometrical shapes of the bones. To avoid geometrical errors due to mesh deformation, quadrilaterals were chosen over triangular meshes, as this allows a consistent topological flow, i.e., following anatomical features, such as the top of the iliac crest, and is more robust toward deformations (Fig. 1).
The topologies were designed to respect salient anatomical structures and to cover the portions of the iliac crest that are relevant for transplant harvesting in reconstructive surgery [15]. To individualize the standard topology in order to represent accurately the shape of each individual pelvic bone surface, a morphing based on guiding landmarks and a cascade of subsequent projection and mesh smoothing operations was performed as implemented in the software Blender version 2.7.8 (Blender Foundation, Amsterdam, Netherlands) and previously reported [16]
Alignment and averaging
Each of the 2000 pelvic models was imported into Blender version 2.7.8 (Blender Foundation, Amsterdam, Netherlands). First, a coarse alignment of the models was performed manually to place them in the center of the global coordinate system and give them matching orientations by turning and tilting until both iliac crests were at the same height and both spinae iliaca anterior superior were facing to the front. This coarse alignment was required to standardize the subsequent steps of generating topologically standardized meshes, as described in the previous section. By the use of a custom in-house developed plugin for the software Blender, anatomical landmarks were placed automatically in relation to salient geometrical features of the pelvic bone models. These landmarks were used to guide the geometry of the standardized topology. To allow for an individual fine adjustment, it was possible to modify the positions of these guiding landmarks. This step was performed by one single, specifically trained operator after defining standardized criteria. The geometrical data of the topologically standardized meshes was stored in a custom file format to allow subsequent statistical averaging.
In the scope of geometrical averaging, all data was loaded and aligned to a common coordinate system by applying the generalized Procrustes analysis (GPA) [17], while omitting scale correction. By doing so, averages were calculated for the whole population.
Cutting guide design and 3D printing
The cutting guides were designed on the 3D model of the averaged pelvis. One cutting guide was designed for each group and one cutting guide was designed on the 3D model of the pelvis, which was averaged from all models (UNIV: overall averaged cutting guide group). The guides were designed with hockey stick layout and an offset of 1 mm to the pelvis. The width of the cutting guides was 30 mm measured from the iliac crest to the caudal border and 30 mm from the spina iliaca anterior superior to the dorsal border (Fig. 2). This design was chosen because it represents the maximum bone portion nourished by the circumflex ilium profunda artery, which is the nourishing vessel. The vessel reaches the Spina iliaca anterior superior at the medial side of the iliac crest [18]. It continues dorsally on the inner side and gives off small branches to the bone. After about 6 cm it crosses the iliac crest, and from there it nourishes the bone [19]. The total length was 80 mm. Also, if bone elevation to the sacroiliac joint is possible, this length is sufficient for most mandibular reconstructions and keeps the integrity of the sacroiliac joint.
From each of the four groups, 10 models were randomly selected and 3D printed. For printing a Stratasys, Fortus 450 mc printer (Stratasys, Eden Prairie, MN, USA) was used. The models were printed with Acrylnitril–Butadien–Styrol copolymer (ABS). Respectively, 10 cutting guides of each group and 10 overall averaged cutting guides were 3D printed via selective laser sintering out of Polyamid 12 (PA12).
Accuracy test
The printed cutting guide was fixed to the printed iliac crest of the matching group with two screws. To do this, a sliding hole was drilled through the template and the screws were tightened manually without creating tension on the guide. This prevents deformation of the guide. Then, the models were scanned with the cone beam CT Galileos Comfort Plus (Sirona Dental Systems GmbH, Wals, Austria) with 98 kV and 30 mAS. The resulting 3D scan was imported into Mimics inPrint version 3.0.0.249 (Materialise, Leuven, Belgium). The gap between the outer surface of the iliac crest and the cutting guide was segmented and saved a STL file.
Evaluation of the models was performed in Geomagic Control X (3D Systems Corporation, Rock Hill, SC, USA). In the software, the thickness of the model was measured (Fig. 3). The mean thickness, and the maximum thickness as well as the volume of the space between the cutting guide and the model of the pelvis were recorded.
Statistical analysis
Statistical analysis was performed using Prism GraphPad version 9 (GraphPad Software Inc., San Diego, California, USA). A Mann–Whitney U test was performed, and the level of significance was set as p ≤ 0.05. All data was expressed as mean values ± standard deviation.
Results
The measured values for the minimum and maximum thickness and the volume of the space between the cutting guide and the pelvic model are shown in Table 1.
In all measured values, the YM group reached significantly lower values than the UNIV and the OM group (Figs. 4, 5, 6). For the maximum and the mean thickness, the values of the YM group were significantly lower than in the OF group (Figs. 4, 5). All other differences between the groups were not significant. The group YM reached the lowest values for each measured category, while the UNIV group did neither reach the greatest thickness nor the highest volume (Table 1).
Discussion
The microvascular reconstruction with a DCIA flap offers enough bone for dental rehabilitation via enossal dental implants and an excellent preformed shape for reconstruction of the mandibular angle [20,21,22]. Before CAD planning was the gold standard for preoperative planning of the DCIA flap transfer [23], the result was highly dependent from the experience and skill of the surgeon. Using CAD planning enables the preoperative simulation of different variants and conditions [24, 25]. The first hurdle in conventional raising of a DCIA flap is determining the necessary dimensions of the graft. To do this, a paper sheet or a metal plate is commonly adapted to the defect as a template and then transferred to the iliac crest using the template. The surgeon has to oversize the template because he can grind away excess bone freehand. However, if the transplant is too small, the missing bone can only be added with difficulty. Compared to the conventional raising of the flap, the CAD planning of microvascular bone flaps for reconstruction of the mandible led to a shortened ischemic time of the transplant [26] and less time for shaping the transplant [27]. Additionally, the supernatant of bone harvested from the pelvis is smaller than harvesting the DCIA with conventional techniques [27]. These advantages have made preoperative CAD planning of microvascular bone flaps the gold standard. The cutting guides developed in this study are intended to offer the same advantages as complete CAD planning, without the need for a pelvic CT. This is achieved by preoperatively adapting the universal cutting guide to the defect of the jaw. The dimensions of the cutting guide are digitally adjusted to the size of the defect and then the universal cutting guide is printed. This means that the DCIA flap can be raised and there is no excess bone but, above all, there is no undersized flap. Due to the precise lifting and the lack of adjustment of the DCIA flap after raising, the cutting guides presented here can be used to keep the excess of raised iliac crest small and reduce the ischemic time compared to the conventional method of flap raising.
A disadvantage that comes with preoperative CAD planning is the necessity of 3D images of the pelvis and the mandible. While the images of the mandible are commonly already available due to the underlying disease, the 3D images of the pelvis must be made exclusively for CAD planning. Unlike the free fibula flap, the vascular anatomy of the DCIA is nearly constant and so angiography is unnecessary [15, 28]. The dose of a CT of the pelvis is around 3–4 mSv [12]. This dose is comparable to the whole natural background radiation dose of a citizen in the USA for a whole year with 3.11 mSv [29]. HNSCC patients receive additional CT scans during follow-up but only of the head and neck area [30]. Without the pelvic CT scan, the cumulative dose for these patients could be reduced.
A completely new approach in medicine is the use of big data [31, 32]. Accessing big data opens up the possibility to improve medical processes. The processing of big data becomes possible with increasing computing capacity. Therefore, it was the aim of this study to prove that the usage of a large dataset of pelvic anatomy could make a CT scan of the pelvis prior CAD planning of the DCIA flap obsolete.
Since dose avoidance is a principle of radiation protection, any avoidable exposure to ionizing radiation should be avoided. Therefore, the aim of this study was to use CT scans already obtained for other reasons to calculate a standard geometry of the iliac crest and design cutting guides on this average geometry. This could make the preoperative CT scan of the pelvis obsolete and save a radiation dose of 3–4 mSv for the patient. Additionally, expensive and scarce resources could be saved in the health system and reduce the expenses for the patient.
The weight of the intestines is transferred to the legs and children are delivered through the female pelvis, leading to a sexual dimorphism between male and females pelvises [14]. The morphological dimorphism is not equally pronounced at every structure of the pelvis. Current literature describes the sexual dimorphism at the iliac crest, which is used for DCIA harvesting, as moderate [33]. Furthermore, because of the different hormonal development of males and females the morphology of the pelvis changes depending not only on the sex but also the age. The female pelvis develops in a different pattern in younger years than after the menopause [8]. To address these differences, a separation of males and females as well as a separation in two separate groups of age was necessary for creating the best fitting stock cutting guide for the DCIA flap. Additionally, a universal cutting guide group (Univ) was created. The Univ group contained all pelvis models for averaging. This group was used as a control group to check whether the gender and age split actually resulted in a better fit of the cutting guides. The CT data used for averaging was obtained in daily routine and retrospectively accessed. Therefore, the ethnicity and race as well as the exact body habitus could not be considered for separation of the data into different groups.
The study was deliberately not conducted purely digitally. Due to the printing of the anatomical models, a printer error of ± 0.127 mm was accepted [34]. However, printing the guides would also be necessary when using them on patients. Therefore, the additional error due to the renewed digitization of the models using CBCT was also accepted. A purely digital comparison of the fit would disregard these processes, which are necessary for use on the patient.
The fitting of the cutting guides to the pelvis was examined by measuring the space between the cutting guide and the iliac crest which was filled with air. The incongruence between the ready-made cutting guide developed in this study and the actual iliac crest of the patient should not result in an error that makes the jaw reconstruction with the DCIA flap impossible. The space had a mean thickness of 2.267 ± 0.6055 mm and a maximum thickness of 6.318 ± 1.459 mm in the UNIV group. Even a gap of 6.5 mm between the guide with its flange and the bone enables the surgeon to securely saw the DCIA transplant at the defined position.
The allocation of the pelvis CTs into different groups led to a significantly reduced mean and maximum thickness of the space as well as their volume for the YM group compared to the UNIV group (p = 0.024; p = 0.001; p = 0.009). Additionally, the results of the YM group were significantly lower in mean and maximum thickness compared to the OF and OM group (p values see Figs. 4, 5, 6) while there was no significant difference for the mean and maximum thickness and the volume between the UNIV group and the YF, OF and OM group. This leads to the assumption that the sexual dimorphism of the pelvis is not that distinct at the iliac crest. Furthermore, the missing significant difference for the mean and maximum thickness as well as the volume between the groups YF and OF shows that the hormonal effect on the morphology of the iliac crest is negligible.
Exact data on how precise the cutting guides fit to the iliac crest is not available in the literature. However, the use of CAD planned cutting guides for osteotomies of free bone flaps should lead to an accurate transition of the virtual plan from the computer into the patient. Nevertheless, the use of 3D printed cutting guides implements an error in this transition [35, 36]. The error does not only result from the design or the existence of the sawing slots, or flanges [37], the secure and reproducible positioning of the guides on the bone is crucial as well [38, 39]. This results in deviations from the original planned position of the osteotomy to the actual position of 1.2 ± 1.0 mm to 2.00 ± 1.12 mm [35, 38]. A perfect transition from the virtual plan into the patient is not possible with this technique. The cutting guides designed in this study should achieve comparable accuracies for the position of the osteotomy as reported in the literature.
As described in the Material and Methods section, the cutting guides in this study were designed for the raising a hockey stick-shaped DCIA flap. However, the dimensions of the universal cutting guides can be modified to adapt the DCIA flap to the bone defect to be reconstructed. A reduction in the dimensions of the cutting guide would in most cases lead to a better fitting of the universal guide with the iliac crest, as in the cases tested in this study the edge of the cutting guide rested at some point. By removing this point, the entire guide can better adhere to the iliac crest. In cases where the edge of the cutting guide does not rest on the iliac crest and the size is reduced, the distance to the iliac crest cannot increase as the contact surface remains the same. A deterioration of the fit by adjusting the size of the guides to a defect is therefore not to be expected.
Conclusion
Even though the anatomy of the iliac crest is highly variable, the large amount of data allows the development of a ready-made cutting guide for the DCIA. These can be adapted to the determined defect size of the mandible and allow the DCIA flap to be lifted quickly and accurately without the need for CT imaging of the pelvis. Thus, significant radiation dose can be saved while maintaining the surgical quality and improving the patient’s outcome.
References
DE Johnson B Burtness CR Leemans VWY Lui JE Bauman JR Grandis 2020 Head and neck squamous cell carcinoma Nat Rev Dis Primers 6 92 https://doi.org/10.1038/s41572-020-00224-3
NCJ Lee JR Kelly HS Park Y An BL Judson BA Burtness ZA Husain 2018 Patterns of failure in high-metastatic node number human papillomavirus-positive oropharyngeal carcinoma Oral Oncol 85 35 39 https://doi.org/10.1016/j.oraloncology.2018.08.001
MM Davudov I Harirchi A Arabkheradmand A Garajei H Mahmudzadeh M Shirkhoda M Motiee-Langroudi Z Mirzajani J Zebardast A Montazeri 2019 Evaluation of quality of life in patients with oral cancer after mandibular resection: comparing no reconstruction, reconstruction with plate, and reconstruction with flap Medicine 98 e17431 https://doi.org/10.1097/md.0000000000017431
S Lonie P Herle A Paddle N Pradhan T Birch R Shayan 2016 Mandibular reconstruction: meta-analysis of iliac- versus fibula-free flaps ANZ J Surg 86 337 342 https://doi.org/10.1111/ans.13274
WY Zhu WS Choi YX Su 2021 Three-dimensional printing technology for deep circumflex iliac artery flap: from recipient to donor sites Plast Reconstr Surg Glob Open 9 e3618https://doi.org/10.1097/gox.0000000000003618
GI Taylor P Townsend R Corlett 1979 Superiority of the deep circumflex iliac vessels as the supply for free groin flaps Clinical work Plast Reconstr Surg 64 745 759 https://doi.org/10.1097/00006534-197912000-00001
JM DeSilva KR Rosenberg 2017 Anatomy, development, and function of the human pelvis Anat Rec 300 628 632 https://doi.org/10.1002/ar.23561
A Huseynov CP Zollikofer W Coudyzer D Gascho C Kellenberger R Hinzpeter MS Ponce de León 2016 Developmental evidence for obstetric adaptation of the human female pelvis Proc Natl Acad Sci USA 113 5227 5232 https://doi.org/10.1073/pnas.1517085113
NK Kim HY Kim HJ Kim IH Cha W Nam 2014 Considerations and protocols in virtual surgical planning of reconstructive surgery for more accurate and esthetic neomandible with deep circumflex iliac artery free flap Maxillofac Plast Reconstr Surg 36 161 167 https://doi.org/10.14402/jkamprs.2014.36.4.161
G Bettini G Saia S Valsecchi G Bedogni A Sandi A Bedogni 2021 Three-dimensional CAD/CAM reconstruction of the iliac bone following DCIA composite flap harvest Int J Oral Maxillofac Surg 50 32 37 https://doi.org/10.1016/j.ijom.2020.05.014
LS Brandenburg PJ Voss T Mischkowsky J Kühle MA Ermer JV Weingart RM Rothweiler MC Metzger R Schmelzeisen P Poxleitner 2023 Donor site morbidity after computer assisted surgical reconstruction of the mandible using deep circumflex iliac artery grafts: a cross sectional study BMC Surg 23 4 https://doi.org/10.1186/s12893-022-01899-z
Medicine AAoPi. AAPM report no. 96. The measurement, reporting, and management of radiation dose in CT College Park, MD: American Association of Physicists in Medicine (2008)
R Schulte C Loberg A Ghassemi 2023 Evaluating the length, diameter, and stenosis of deep circumflex iliac artery and neighboring arteries based on digital subtraction angiography Microsurgery https://doi.org/10.1002/micr.31022
B Fischer P Mitteroecker 2017 Allometry and sexual dimorphism in the human pelvis Anat Rec 300 698 705 https://doi.org/10.1002/ar.23549
K-D Wolff F Hölzle 2005 Raising of microvascular flaps: a systematic approach Springer Berlin
S Raith S Wolff T Steiner A Modabber M Weber F Hölzle H Fischer 2017 Planning of mandibular reconstructions based on statistical shape models Int J Comput Assist Radiol Surg 12 99 112 https://doi.org/10.1007/s11548-016-1451-y
JC Gower 1975 Generalized procrustes analysis Psychometrika 40 33 51
GI Taylor P Townsend R Corlett 1979 Superiority of the deep circumflex iliac vessels as the supply for free groin flaps Plast Reconstr Surg 64 595 604
A Ghassemi R Furkert A Prescher D Riediger M Knobe D O'Dey M Gerressen 2013 Variants of the supplying vessels of the vascularized iliac bone graft and their relationship to important surgical landmarks Clin Anat 26 509 521 https://doi.org/10.1002/ca.22199
JL Frodel Jr GF Funk DT Capper KL Fridrich JR Blumer JR Haller HT Hoffman 1993 Osseointegrated implants: a comparative study of bone thickness in four vascularized bone flaps Plast Reconstr Surg 92 449 455 discussion 56-8
K Kniha SC Möhlhenrich AC Foldenauer F Peters N Ayoub E Goloborodko F Hölzle A Modabber 2017 Evaluation of bone resorption in fibula and deep circumflex iliac artery flaps following dental implantation: a three-year follow-up study J Craniomaxillofac Surg 45 474 478 https://doi.org/10.1016/j.jcms.2017.01.014
D Riediger 1988 Restoration of masticatory function by microsurgically revascularized iliac crest bone grafts using enosseous implants Plast Reconstr Surg 81 861 877 https://doi.org/10.1097/00006534-198806000-00007
P Winnand N Ayoub T Redick J Gesenhues M Heitzer F Peters S Raith D Abel F Hölzle A Modabber 2022 Navigation of iliac crest graft harvest using markerless augmented reality and cutting guide technology: a pilot study Int J Med Robot 18 e2318https://doi.org/10.1002/rcs.2318
A Modabber N Ayoub A Bock SC Möhlhenrich B Lethaus A Ghassemi DA Mitchell F Hölzle 2017 Medial approach for minimally-invasive harvesting of a deep circumflex iliac artery flap for reconstruction of the jaw using virtual surgical planning and CAD/CAM technology Br J Oral Maxillofac Surg 55 946 951 https://doi.org/10.1016/j.bjoms.2017.09.005
A Modabber M Gerressen N Ayoub D Elvers JP Stromps D Riediger F Hölzle A Ghassemi 2013 Computer-assisted zygoma reconstruction with vascularized iliac crest bone graft Int J Med Robot 9 497 502 https://doi.org/10.1002/rcs.1557
A Modabber M Gerressen MB Stiller N Noroozi A Füglein F Hölzle D Riediger A Ghassemi 2012 Computer-assisted mandibular reconstruction with vascularized iliac crest bone graft Aesthetic Plast Surg 36 653 659 https://doi.org/10.1007/s00266-012-9877-2
N Ayoub A Ghassemi M Rana M Gerressen D Riediger F Holzle A Modabber 2014 Evaluation of computer-assisted mandibular reconstruction with vascularized iliac crest bone graft compared to conventional surgery: a randomized prospective clinical trial Trials 15 114 https://doi.org/10.1186/1745-6215-15-114
ML Urken ML Cheney KE Blackwell JR Harris TA Hadlock N Futran 2012 Atlas of regional and free flaps for head and neck reconstruction: flap harvest and insetting Lippincott Williams & Wilkins Philadelphia
J Thurston 2010 NCRP report no. 160: ionizing radiation exposure of the population of the United States Phys Med Biol 55 6327 https://doi.org/10.1088/0031-9155/55/20/6327
JP Machiels C René Leemans W Golusinski C Grau L Licitra V Gregoire 2020 Squamous cell carcinoma of the oral cavity, larynx, oropharynx and hypopharynx: EHNS-ESMO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up Ann Oncol 31 1462 1475 https://doi.org/10.1016/j.annonc.2020.07.011
K Benke G Benke 2018 Artificial intelligence and big data in public health Int J Environ Res Public Health https://doi.org/10.3390/ijerph15122796
L Wang CA Alexander 2020 Big data analytics in medical engineering and healthcare: methods, advances and challenges J Med Eng Technol 44 267 283 https://doi.org/10.1080/03091902.2020.1769758
SL Cox 2021 A geometric morphometric assessment of shape variation in adult pelvic morphology Am J Phys Anthropol 176 652 671 https://doi.org/10.1002/ajpa.24399
Stratasys (2023) Fortus 450mc brochure https://www.stratasys.com/contentassets/4f4547ca56fb493eaaa7fffe3aeb678e/br_fdm_fortus450mc_0823b.pdf?v=4a8ee9. Accessed 19 Dec 2023
SM Roser S Ramachandra H Blair W Grist GW Carlson AM Christensen KA Weimer MB Steed 2010 The accuracy of virtual surgical planning in free fibula mandibular reconstruction: comparison of planned and final results J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 68 2824 2832 https://doi.org/10.1016/j.joms.2010.06.177
D Steybe P Poxleitner MC Metzger R Schmelzeisen MF Russe MA Fuessinger LS Brandenburg PJ Voss S Schlager 2022 Analysis of the accuracy of computer-assisted DCIA flap mandibular reconstruction applying a novel approach based on geometric morphometrics Head Neck-J Sci Spec 44 2810 2819 https://doi.org/10.1002/hed.27196
Z Dong B Li R Xie Q Wu L Zhang S Bai 2017 Comparative study of three kinds of fibula cutting guides in reshaping fibula for the reconstruction of mandible: an accuracy simulation study in vitro J Craniomaxillofac Surg 45 1227 1235 https://doi.org/10.1016/j.jcms.2017.04.009
SG Brouwer de Koning TP Braak Ter F Geldof RLP Veen van MJA Alphen van LHE Karssemakers WH Schreuder MB Karakullukcu 2021 Evaluating the accuracy of resection planes in mandibular surgery using a preoperative, intraoperative, and postoperative approach Int J Oral Maxillofac Surg 50 287 293 https://doi.org/10.1016/j.ijom.2020.06.013
B Philippe 2020 Accuracy of position of cutting and drilling guide for sagittal split guided surgery: a proof of concept study Br J Oral Maxillofac Surg 58 940 946 https://doi.org/10.1016/j.bjoms.2020.04.034
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Florian Peters, Stefan Raith, Anna Bock, Kristian Kniha, Stephan Christian Möhlhenrich, Marius Heitzer, Frank Hölzle and Ali Modabber have no financial or proprietary interests in any material discussed in this article.
Ethical approval
Institutional approval (EK 260/20) of the local ethics committee was obtained.
Human and animal rights
All procedures in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peters, F., Raith, S., Bock, A. et al. Development of a universal cutting guide for raising deep circumflex iliac artery flaps. Int J CARS (2024). https://doi.org/10.1007/s11548-024-03144-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11548-024-03144-9