Abstract
Purpose
A methodological framework is introduced to assess and compare a conventional fluoroscopy protocol for peripheral angioplasty with a new magnetic resonant imaging (MRI)-guided protocol. Different scenarios were considered during interventions on a perfused arterial phantom with regard to time-based and cognitive task analysis, user experience and ergonomics.
Methods
Three clinicians with different expertise performed a total of 43 simulated common iliac angioplasties (9 fluoroscopic, 34 MRI-guided) in two blocks of sessions. Six different configurations for MRI guidance were tested in the first block. Four of them were evaluated in the second block and compared to the fluoroscopy protocol. Relevant stages’ durations were collected, and interventions were audio-visually recorded from different perspectives. A cued retrospective protocol analysis (CRPA) was undertaken, including personal interviews. In addition, ergonomic constraints in the MRI suite were evaluated.
Results
Significant differences were found when comparing the performance between MRI configurations versus fluoroscopy. Two configurations [with times of 8.56 (0.64) and 9.48 (1.13) min] led to reduce procedure time for MRI guidance, comparable to fluoroscopy [8.49 (0.75) min]. The CRPA pointed out the main influential factors for clinical procedure performance. The ergonomic analysis quantified musculoskeletal risks for interventional radiologists when utilising MRI. Several alternatives were suggested to prevent potential low-back injuries.
Conclusions
This work presents a step towards the implementation of efficient operational protocols for MRI-guided procedures based on an integral and multidisciplinary framework, applicable to the assessment of current vascular protocols. The use of first-user perspective raises the possibility of establishing new forms of clinical training and education.





Similar content being viewed by others
References
Saeed M, Wilson M (2012) Value of MR contrast media in image-guided body interventions. World J Radiol 4(1):1–12
Bock M, Wacker FK (2008) MR-guided intravascular interventions: techniques and applications. JMRI 27(2):326–338
Kos S, Huegli R, Bongartz GM, Jacob AL, Bilecen D (2008) MR-guided endovascular interventions: a comprehensive review on techniques and applications. Eur Radiol 18(4):645–657
Losey A, Lillaney P, Martin A, Cooke D (2014) Magnetically assisted remote-controlled endovascular catheter for interventional MR imaging. In vitro navigation at 1.5 T versus X-ray fluoroscopy. Radiology 271(3):862–869
Gentric J-C, Trelhu B, Jannin P, Riffaud L, Ferré J-C (2013) Development of workflow task analysis during cerebral diagnostic angiographies: time-based comparison of junior and senior tasks. J Neuroradiol 40(5):342–347
Flin R, Yule S, McKenzie L, Paterson-Brown S, Maran N (2006) Attitudes to teamwork and safety in the operating theatre. Surgeon 4(3):145–151
Johnson S, Healey a, Evans J, Murphy M, Crawshaw M, Gould D (2006) Physical and cognitive task analysis in interventional radiology. Clin Radiol 61(1):97–103
Van Herzeele I, Aggarwal R, Neequaye S, Darzi A, Vermassen F, Cheshire NJ (2008) Cognitive training improves clinically relevant outcomes during simulated endovascular procedures. J Vasc Surg 48(5):1223–1230
van Gog T, Paas F, van Merriënboer JJG, Witte P (2005) Uncovering the problem-solving process: cued retrospective reporting versus concurrent and retrospective reporting. J Exp Psychol Appl 11(4):237–244
Brusin JH (2011) Ergonomics in radiology. J Am Soc Radiol Technol 83(2):141–157
García-Lallana a, Viteri-Ramírez G, Saiz-Mendiguren R, Broncano J (2011) Ergonomics of the workplace in radiology. Radiol Engl Ed 53(6):507–515
Sikkink CJJM, Reijnen MMPJ, Zeebregts CJ (2008) The creation of the optimal dedicated endovascular suite. Eur J Vasc Endovasc Surg 35(2):198–204
Rostenberg B, Barach PR (2011) Design of cardiovascular operating rooms for tomorrow’s technology and clinical practice—part one. Prog Pediatr Cardiol 33(1):57–65
Rube MA, Fernandez-Gutierrez F, Cox BF, Holbrook AB, Houston JG, White RD, McLeod H, Fatahi M, Melzer A (2014) Preclinical feasibility of a technology framework for MRI-guided iliac angioplasty. Int J CARS. doi:10.1007/s11548-014-1102-0
Chaffin D (2008) Digital human modeling for workspace design. Rev Hum Factors Ergon 4(1):41–74
Santos JM, Wright Ga, Pauly JM (2004) Flexible real-time magnetic resonance imaging framework. Conf Proc IEEE Eng Med Biol Soc 2:1048–1051
Ballinger Ga (2004) Using generalized estimating equations for longitudinal data analysis. Organ Res Methods 7(2):127–150
Law AM (2007) Simulation modeling and analysis, 4th edn. Mcgraw Hill Higher Education, New York
He Y (2010) Missing data analysis using multiple imputation: getting to the heart of the matter. Circul Cardiovasc Qual Outcomes 3(1):98–105
McAtamney L, Nigel Corlett E (1993) RULA: a survey method for the investigation of work-related upper limb disorders. Appl Ergon 24(2):91–99
Woodson WE, Tillman B, Tillman P (1992) Human factors design handbook, 2nd edn. McGraw Hill, New York
Fernandez-Gutierrez F, Ferut J, Smink J, Houston G, Melzer A (May 2013) Ergonomics for MRI guided procedures. Case of study: postural analysis for MRI scanners. In: Proceedings of the 27th international congress and exhibition. Int J Comput Assist Radiol Surg 8(S1):5–11
Takahara T, Kwee T, Kibune S, Ochiai R, Sakamoto T, Niwa T, Van Cauteren M, Luijten P (2010) Whole-body MRI using a sliding table and repositioning surface coil approach. Eur Radiol 20(6):1366–1373
Kettenbach J, Kacher DF, Kanan AR, Rostenberg B, Fairhurst J, Stadler A, Kienreich K, Jolesz Fa (2006) Intraoperative and interventional MRI: recommendations for a safe environment. MITAT 15(2):53–64
Buckingham G, Wong JD, Tang M, Gribble PL, Goodale MA (2014) Observing object lifting errors modulates cortico-spinal excitability and improves object lifting performance. Cortex 50:115–124
Duncan JR, Kline B, Glaiberman CB (2007) Analysis of simulated angiographic procedures. Part 2: extracting efficiency data from audio and video recordings. JVIR 18(4):535–544
Beta E, Parikh AS, Street M, Duncan JR (2009) Capture and analysis of data from image-guided procedures. JVIR 20(6):769–781
Klein LW, Miller DL, Balter S, Laskey W, Haines D, Norbash A, Mauro MA, Goldstein JA (2009) Occupational health hazards in time for a safer environment. Radiology 250(2):538–544
Mohseni-Bandpei Ma, Ahmad-Shirvani M, Golbabaei N, Behtash H, Shahinfar Z, Fernández-de-las-Peñas C (2011) Prevalence and risk factors associated with low back pain in Iranian surgeons. J Manip Physiol Therap 34(6):362–370
Pérez-Duarte FJ, Lucas-Hernández M, Matos-Azevedo a, Sánchez-Margallo Ja, Díaz-Güemes FM (2014) Objective analysis ofsurgeons’ ergonomy during laparoendoscopic single-site surgery through the use of surface electromyography and a motion capture data glove. Surg Endosc 28(4):1314–1320
Kramp KH, van Det MJ, Totte ER, Hoff C, Pierie J-PEN (2014) Ergonomic assessment of the French and American position for laparoscopic cholecystectomy in the MIS Suite. Surg Endosc 28(5):1571–1578
Neumuth T, Jannin P, Strauss G, Meixensberger J, Burgert O (2008) Validation of knowledge acquisition for surgical process models. J Am Med Inform Assoc 6(1):72–80
Acknowledgments
We thank Lynda Cochrane from the Dundee Epidemiology and Biostatistics Unit (University of Dundee) for her assistance during the statistical analysis, as well as John Ferrut for his support for the ergonomic evaluation. The authors are thankful for financial assistance provided by the FUSIMO (“Patient specific modelling and simulation of focused ultrasound in moving organs”) project funded under the European Community’s Seventh Framework Programme (FP7/2007–2013) for Research and Technological Development under Grant Agreement No. 270186. The Marie Curie Initial Training Network supported this work, and the Integrated Interventional Imaging Operating System (IIIOS) project has received funding from the European Community’s Seventh Framework Programme (FP7/2007–2013) under Grant Agreement No. 238802.
Conflict of interest
The Integrated Interventional Imaging Operating System (IIIOS) project has received funding from the European Community’s Seventh Framework Programme (FP7/2007–2013) under Grant Agreement No. 238802. Fabiola Fernandez-Gutierrez, Martin A. Rube, Mahsa Fatahi and Benjamin F. Cox have received funding from the European Union (IIIOS project). Helen McLeod, Karen French and Mariana Gueoguieva have received funding from the European Union (FUSIMO project, Grant Agreement No. 270186). Kenneth Scott-Brown, Santiago Martinez, Richard D. White and Erwin Immel have no conflicts of interest. Graeme J. Houston is director, shareholder, patent holder and receives royalty at Tayside Flow Technologies Ltd. Andreas Melzer is consultant and shareholder at INNOMEDIC GmbH, Herxheim, Germany.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
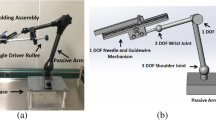
Facilities and equipment
Fluoroscopy-guided interventions were performed on a digital subtraction angiography (DSA) unit (OEC 9900 Elite, GE Medical Systems, Waukesha, WI, USA). MRI-guided interventions used a 1.5 T MRI scanner (Signa HDxt, GE Medical Systems, Waukesha, WI, USA).
The experimental set-ups were all conducted on an arterial vessel phantom consisting of linked femoral, abdominal and thoracic module (L-F-S-Left-003, A-S-N-001, T-R-N-020, Elastrat, Sarl, Switzerland). The phantom was connected to a heart-lung machine (HL-30, Maquet, Rastatt, Germany), customising one HL-30 D150 pump to mimic (pulsatile) physiologic flow. Plastic tubes were taken from the phantom to the heart-lung machine, which was in an annex room. Tubes passed the Faraday cage through the wave guides. Silicon tubing (PT 12.7 \(\times \) 3.2, Silex, Bordon, UK) with an inner diameter of 16 mm and length of 5 m was used. An arterial blood pressure monitoring kit with a trace was also used to examine systolic/diastolic pressures during the interventions. A permanent introducer sheath (12F) was inserted into the femoral artery to provide access and exchange of devices during the interventions. A neonatal blood pressure cuff (SoftCheck Neonatals, Statcorp Medical, Jacksonville, FL, USA) was secured to the right common iliac artery (with electrical tape and rubber sheet) to mimic stenosis (see “Appendix” in Fig. 6).
Fully perfused thorax to above the knee vascular phantom (Elastrat, Sarl, Switzerland). Red arrow indicates the 12F sheath introducer used for permanent access. Blue arrow indicates a neonatal pressure cuff (SoftCheck Neonatals, Statcorp Medical, Jacksonville, FL, USA) that was attached to the right common iliac artery to mimic a stenosis
The two workstations used in the MRI, standard control console (software release 15.0M4A, GE Healthcare, Waukeska, WI, USA) and the real-time MRI software framework (RTHawk, Version 0.9.28, HeartVista, Inc., Los Altos, CA, USA) were in communication via Gigabit Ethernet and were connected via optical fibre cables (M1-1000, Opticis, Sungnam City, Korea) to a shielded 40” LCD monitor (Multeos 401, NEC Corporation, Tokyo, Japan) to display the MR images inside the MRI scanner room.
IP cameras models were: M1011w and M1031w, Axis Communications, Lund, Sweden.
Recoding spectacles were PivotHead, models Durango Chameleon and Recon Black Jet frames with no lenses fitted (Cape Evolution Ltd, Greenwood Village, CO, USA).
Second tablet device used for scanner/control room communication was an iPad 3 (Apple Inc., Cupertino, CA, USA), and the Bluetooth earphones were Calisto B70 (Plantronics, Santa Cruz, CA, USA).
Devices
We customised commercially available non-braided balloon catheters (5F PTA Balloon catheter, Workhorse II, AngioDynamics, Lathan, NY, USA) by attaching a resonant circuit 5 mm distally to the inflatable balloon. Each resonant circuit was tuned to 63.8 MHz (the proton Larmor frequency at 1.5 T) in 0.9 % saline solution.
Additional devices used during the interventions included:
-
5-F Straight catheter (BeaconTipRoyal Flush, CookInc., Bloomington, IN, USA), length 70 cm (lumen 0.035”)
-
6-F Multipurpose catheter (Soft-Vu, AngioDynamics, Latham, NY, USA), length 90 cm (lumen 0.035”)
-
For fluoroscopy, commercially available 0.035” guidewires (Standard Glidewire, Terumo, Somerset, NJ, USA) were used.
-
For MRI, a novel hydrophilic-coated and MRI-safe guidewire prototype that was developed with EPflex GmbH (Dettingen/Erms, Germany) was used, with a diameter of 0.035” and a length of 120 cm.
A detailed description of the fabrication of this devices can be read in Rube et al. [14].
Rights and permissions
About this article
Cite this article
Fernández-Gutiérrez, F., Martínez, S., Rube, M.A. et al. Comparative ergonomic workflow and user experience analysis of MRI versus fluoroscopy-guided vascular interventions: an iliac angioplasty exemplar case study. Int J CARS 10, 1639–1650 (2015). https://doi.org/10.1007/s11548-015-1152-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-015-1152-y