Abstract
Background
Stereotactic radiotherapy (SRT) and Proton therapy (PT) are both options in the management of liver lesions. Limited clinical-dosimetric comparison are available. Moreover, dose-constraint routinely used in liver PT and SRT considers only the liver spared, while optimization strategies to limit the liver damaged are poorly reported.
Methods
Primary endpoint was to assess and compare liver sparing of four contemporary RT techniques. Secondary endpoints were freedom from local recurrence (FFLR), overall survival (OS), acute and late toxicity. We hypothesize that Focal Liver Reaction (FLR) is determined by a similar biologic dose. FLR was delineated on follow-up MRI. Mean C.I. was computed for all the schedules used. A so-called Fall-off Volume (FOV) was defined as the area of healthy liver (liver-PTV) receiving more than the isotoxic dose. Fall-off Volume Ratio (FOVR) was defined as ratio between FOV and PTV.
Results
213 lesions were identified. Mean best fitting isodose (isotoxic doses) for FLR were 18Gy, 21.5 Gy and 28.5 Gy for 3, 5 and 15 fractions. Among photons, an advantage in terms of healthy liver sparing was found for Vmat FFF with 5mm jaws (p = 0.013) and Cyberknife (p = 0.03). FOV and FOVR resulted lower for PT (p < 0.001). Three years FFLR resulted 83%. Classic Radiation induced liver disease (RILD, any grade) affected 2 patients.
Conclusions
Cyberknife and V-MAT FFF with 5mm jaws spare more liver than V-MAT FF with 10 mm jaws. PT spare more liver compared to photons. FOV and FOVR allows a quantitative analysis of healthy tissue sparing performance showing also the quality of plan in terms of dose fall-off.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver metastasis represent the most frequent type of liver cancer, whereas Hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC) are the two most common types of primary liver cancer [1].
Even if characterized by different biology and natural history, metastatic and primary liver cancer both share the possibility to be effectively managed with local therapies [2,3,4]. In the past, radiotherapy played an ancillary role given the impossibility to safely deliver therapeutic dose while sparing the healthy liver [5,6,7,8,9]. The development of Stereotactic radiotherapy (SRT) and Proton therapy (PT) has revolutionized the role of radiation oncologist in the management of liver lesions [10, 11]. Such techniques guarantee to reach ablative doses to the target while minimizing healthy liver irradiation, making radiation induced liver disease (RILD) a relative rare adverse event [12].
Photon SRT techniques, such as Volumetric modulated IMRT (V-MAT) with or without flattening filter and Robotic IMRT present an high degree of conformity to the target and different possibilities concerning motion management strategies [13,14,15,16,17]. PT has the theoretical advantage to exploit the unique proton beams physics proprieties, with an energy deposition at a pre-specified depth, that allows to spare beam exits and consequently reduce the radiation exposure of normal tissues [18]. A Recent meta-analysis comparing efficacy and safety of these two treatment modalities did not show differences in terms of local control and suggested a possible lower toxicity with PT [12]. Advances in systemic treatments and the consequent longer survival expected in the context of metastatic disease and HCC will require local treatment optimization in terms of efficacy and healthy liver sparing [19,20,21]. The aim of present study is to compare plan performance and clinical results of four advanced radiotherapy techniques performed for the treatment of HCC, ICC and liver metastasis. Particular interest will be reserved in the assessment and comparison of the four different techniques in terms of healthy liver sparing.
Materials and methods
The present study is a multicentric, retrospective analysis run by 4 Radiation Oncology Center. The local Ethical committee approved the study. Inclusion criteria were:
-
Localized HCC, ICC, or liver metastasis.
-
Treatment performed with photon SRT using three techniques, robotic delivered Cyberknife® M6 Linac, V-MAT 5 mm jaws flattening filter free (V-MAT FFF 5 mm) and V-MAT 10 mm jaws with flattening filter (V-MAT FF 10 mm).
-
Treatment performed with PT with active scanning technique.
-
Biologic effective dose (BED) of more than 70 Gy (alpha beta ratio of 10 Gy for the tumor).
-
ECOG (Eastern Cooperative Oncology Group criteria) Performance status ≤ 2
-
Patients ineligible for surgery or radiofrequency ablation because of tumor site/characteristics, advanced age, comorbidity or procedure refusal
-
Child–Pugh class up to B7
-
All patients were staged with contrast enhanced computed tomography (CT) scan. Upper abdomen MRI or PET-CT were suggested but not mandatory.
-
Have participated at follow-up following protocol indication listed in the specific section.
-
Additional inclusion criteria for primary endpoint analysis were:
-
Dose to 95% of PTV reached at least 95% of prescription dose.
-
Available DICOM images of three months follow-up contrast enhanced Hepatobiliary phase MRI (T1-weighted fat-suppressed sequences).
-
Lesions more than one centimeter from the liver surface (extremely peripherical lesion excluded).
RT planning
Simulation, planning and delivery protocols strictly depended by RT technique used. All patients were simulated and treated in supine position. When indicated, three phasic contrast enhanced CT scan was performed. For Photon SRT, patients were treated with Cyberknife, V-MAT FFF 5 mm (TrueBeam™, Varian®) and V-MAT FF 10 mm Synergy ™, Elekta®). Simulation, planning and delivery exploited 4D-ITV delivery and tumor tracking with perilesional gold fiducial marker implant.
For PT, patients were simulated in supine position, the ABC System ™ (ELEKTA®) was exploited and deep inspiration breath hold (DIBH)-triggered planning CT scan was acquired. Patients were treated with active scanning technology that allows intensity modulated proton therapy. Pre-treatment IGRT consisted in surface guidance and portal imaging during DIBH. In supplementary Table 1s is reported the RT technique used by each center.
Follow-up protocol and assessment of tumor response
Physical examination, blood count, liver function test, total bilirubin, INR, ALP, GGT, were performed 28–30 days after SBRT and then at each follow-up. Patients were followed every 3 months the first year after treatment, every 4 months for the second year and every 6 months thereafter. Assessment of tumor response followed RECIST criteria and was made with contrast enhanced CT scan [22] and upper abdomen contrast enhanced MRI to confirm tumor response and to perform the primary endpoint analysis. Technical aspects of MRI were represented by the use of both 1.5 T and 3 T MRI (Philips®, Siemens®). Hepatobiliary phase images of contrast-enhanced MRI were acquired 20 min after the Gd-EOB-DTPA contrast medium injection, T1-weighted fat-suppressed sequences were considered for primary endpoint purpose [23].
Study endpoints and study methodology
Primary endpoint was to assess and compare the dosimetric healthy liver sparing performance of the four RT techniques included in the present study. We firstly standardized plans in terms of dose to the healthy liver. Secondly, we identified variables useful to quantify and compare liver sparing of RT plans [Fall-off volume (FOV) and Fall-off volume ratio (FOVR)].
The methodology for the primary endpoint analysis is reported as follows:
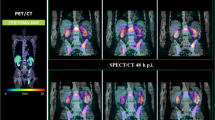
The first step was to identify isotoxic dose resulting in liver damage for treatment using different schedules and techniques. We exploited the concept of SRT-induced area of liver damage called focal liver reaction (FLR). FLR refers to the change in imaging features of the liver parenchyma adjacent to the SRT target lesion, corresponding pathologically to veno-occlusive disease. [24] We hypothesize that such damage becomes evident at MRI for similar biologically effective doses (BED), despite the dose-fractionation used. We exploited the unique features of FLR imaging to identify BED values needed to induce FLR. We delineated on each available 3 months follow-up MRI of each patient (on hepatobiliary phase, fat suppressed T1 weighted images) the FLR. Original plans and original DICOM images of planning CT were coregistered with the corresponding follow-up MRI. Two trained radiation oncologist delineated area of FLR on each available MRI image, after the delineation a radiologist with more than 10 years of experience on liver MRI supervised and confirmed the results. To identify best fitting isodose corresponding to FLR, Conformity Index (CI) was assessed for each patient on each RT plan available and was defined as follows:
where “A” consists in isodose overlapping with liver and “B” the FLR. The contouring was performed on the Velocity™ software both for photons and protons treatments. A representation of the process is reported in Fig. 1. Mean CI and mean isodose related to FLR were computed for patients treated with schedules of three, five and fifteen fractions, with the objective to identifying mean isotoxic doses.
Representation of the isodose extraction process. In brief, coregistration of planning CT and 3 months follow-up MRI (hepatobiliary phase, fat-suppressed T1 weighted images), delineation on the FLR on MRI, coregistration of dose deliverd and CI extraction. Such process has been performed for all patients respecting study inclusion criteria
Thereafter, linear quadratic model was applied to verify radiobiologic consistency of our assumptions. Biologic effective dose was computed as follows:
where “D” is the total dose, “d” is the dose per fraction; for the healthy liver α/β ratio was considered equal to 5 Gy. [25]
The second step was to identify parameters useful to compute and compare liver sparing in the standardized population.
A so-called Fall-off Volume (FOV) was conceived and defined as follows:
where “rVx” is the liver volume receiving less than the isotoxic dose (Gy).
The result represents the area of the healthy liver receiving at least the isotoxic dose with photon- or proton-therapy, respectively. Iconographic description of FOV is represented in Fig. 2.
Subsequently, a Fall-off volume ratio (FOVR) was conceived and defined as:
FOVR is a quantitative representation reflecting the steepness of dose fall-off in relationship to PTV dimension. Therefore, FOVR can result as reported in Fig. 3.
Secondary endpoints were freedom from local recurrence (FFLR), overall survival (OS), acute and late toxic effects, assessed with the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 5.0 [26];
Statistical analysis
For statistical analysis concerning FOV and FOVR, normality of the distributions was assessed using the Kolmogorov–Smirnov test, continuous variables were presented as medians, and min/max (in case of a skewed distribution). Comparison between FOV and FOVR between techniques were performed with the use of the Mann–Whitney and Kruskal–Wallis test; a two-sided α level of 0.05 was used for all tests.
For statistical analysis concerning secondary endpoints, the distribution of the different clinical and therapeutic features was compared with Chi square test.
Univariate analysis was performed to identify variables with a statistically significant impact on each outcome. Survival analysis was performed with the Kaplan–Meier method and the log rank test was applied to compare the effect of the individual variables on the different outcomes. A Cox proportional hazards model was planned to find independent predictors of local recurrence and survival. Univariate analysis led the selection of variables to consider as predictors. All tests were two tailed and the probability value of less than 0.05 was considered statistically significant.
Acute toxicity was defined as any adverse event occurring from the beginning of the RT up to 180 days afterward. Late toxicity was defined as any adverse event occurring at least 181 days after RT. Concerning RILD [27] this definition was used:
-
CLASSIC “anicteric” radiation induced liver disease (RILD): ascites, hepatomegaly, fatigue, abdominal pain, ALP × 2 1–3 months after RT (Type 1)
-
NON-CLASSIC RILD: jaundice with elevated transaminase × 5, without increase in ALP OR a decline in liver function (measured by a worsening of Child–Pugh score by 2 points or more (Type 2)
Gathered data were analyzed using SPSS® v.26.0 software (IBM®).
Moreover, given the rarity of RILD in modern series, an eventual upgrade in CHILD–PUGH class was scored after radiotherapy.
Results
The current study was carried out according to the Declaration of Helsinki and was approved by local ethical committee. Between February 2014 and May 2021, a total of 178 patients bearing 213 hepatic lesions meeting the inclusion criteria were identified. Median age was 72 years (range 38–88 years). Majority of patients presented with Child–Pugh class A5 (87%). Hepatocellular carcinoma was the most frequent type of lesion included in the study (39%), 6% were ICC, whereas almost 55,1% of the lesions were metastasis from various kinds of primary cancers. Median lesion diameter was 2,3 cm (range 0,5–13 cm) while median liver volume was 1348 cc (range 689–3189 cc). Eligible patient’s characteristics are available in supplementary material Table 2s.
Table 1 reports treatment characteristics. Radiation therapy techniques were classified as follows: 62 lesions (29%) were treated with V-MAT FFF 5 mm, 74 (35%) with V-MAT FF 10 mm, 50 (23%) of lesions were treated with robotic SRT with Cyberknife™ and 27 (13%) with protons. The most frequent treatment schedules were 60 Gy/3 fractions (43% of the cases) for photon SRT, while proton therapy schedules delivered 58–67.5 Gy in 15 fractions (13%). Concerning target characteristics, median GTV was 6.4 cc (range 0.13–789.1 cc) and median PTV was 29.3 cc (range 4.4–1318.9 cc).
Table 2 describes the different radiation therapy techniques in relation to GTV and PTV dimension. Median PTV was comprised between 20 and 30 cc for the entire population treated with photons whereas median PTV resulted 242 cc for the lesions treated with PT. Dose to the 95% of the PTV reached at least 95% of the prescription dose in 155 lesions (79%). For photons, 12% of planned treatments did not respect the criteria of ICRU 83 coverage whereas this percentage rises to 78% for PT. Supplementary Table 3s describes the different radiation therapy techniques in relation to ICRU 83 coverage of the target volume. Moreover, dosimetric details of plan quality for the whole series are provided in supplementary material Table 4s.
Primary endpoint analysis
161 patients meet the inclusion criteria to participate in primary endpoint analysis.
The 18 Gy isodose (range 16.9–19.3Gy) resulted to be the mean best fitting isodose related to FLR for three fractions schedule (with a mean CI 0.78, range 0.74–0.91). Corresponding mean values for five and fifteen fraction schedules were 21.5 Gy (range 19.7- 22.4 Gy), with a mean CI of 0.8 (range 0.76–0.93), and 28.5 Gy (range 27–29 Gy), with a mean CI of 0.74 (range 0.7–0.91). Complete results of best fitting isodose and CI extraction for each lesion treated with three, five and fifteen fractions radiotherapy schedule are presented in supplementary Table 5s, 6s and 7s.
The linear quadratic model was used to calculate the BED for 18 Gy in three fractions (39.6 Gy in 3 fractions). We derived from this value of BED the corresponding value of the isotoxic dose in 5 and 15 fractions, which resulted 21.3 Gy and 28.6 Gy for 5 and 15 fractions, respectively. Such results confirmed the results of our MRI-based biological model. To take into account impact of background liver health, we verified isotoxic dose related to liver damage in patients with healthy liver versus patients with Cirrhosis. Of 161 patients available for the analysis, 60 presented a at radiotherapy with a Cirrhosis condition. Beneath this subpopulation, fifty four presented a Child–Pugh class A5, four patients A6 and two patients B7. Concerning RT schedule in cirrhotic patients, 45 were treated with 60Gy in 3 fractions in alternate days, two patients with 48 Gy in 3 fractions in alternate days, 19 with 67.5 Gy in 15 fractions. C.I. for FLR in the whole Cirrhotic population resulted 17.3 Gy (i.e., versus 18 Gy in the whole population) for three fractions schedule (mean C.I. 0.81). Corresponding value for fifteen fractions schedule were 27.6 Gy (i.e., versus 28.5 Gy in the whole population) (mean C.I. 0.74). At statistical analysis, comparison between dose related to FLR between non-Cirrhotic and Cirrhotic population did not reach statistical significance.
Therefore, 18 Gy in three fractions, 21.5 Gy in five fractions and 28.5 Gy in 15 fractions seem to be isoeffective in causing the FLR and presence of cirrhosis seems to have a minor or no impact in FLR we proceeded in the primary endpoint analysis.
A so-called Fall-off Volume (FOV) was defined as follows:
where “rV” is the liver volume receiving less than 18, 21.5 and 28.5 Gy, respectively.
The result represents the area of the healthy liver receiving at least 18 Gy (3 fractions), 21.5 Gy (5 fraction) and 28.5 Gy (15 fractions) with photon- or proton-therapy, respectively.
Median FOV resulted 158 cc, 180cc, 129 cc, 62 cc in V-MAT FFF 5mm, V-MAT FF 10mm, Cyberknife and Proton plans, respectively. Difference in FOV between proton and photons (any techniques) resulted statistically significant in favor to protons (p < 0.001). A significantly better FOV between photons techniques was observed for V-MAT FFF 5mm and for Cyberknife treatment compared to V-MAT 10MM (p = 0.02 and p = 0.014 respectively).
Median FOVR was 0,57 (range 0.1–1.54) for proton plans, whereas rises up to 4.5 (range 0.93–16) for V-MAT FFF 5 mm, 5 (range 3–9.7) for Cyberknife plans, 6.2 (range 2–24.5) for V-MAT FF 10mm. Difference in FOVR between proton and photons (any techniques) resulted statistically significant (p < 0.001). A significantly better FOVR between photons techniques was observed for VMAT FFF 5mm and for Cyberknife treatment compared to VMAT FF 10mm (p = 0.013 and p = 0.03, respectively). No difference between VMAT FFF 5mm and Cyberknife technique was found. A comparison between each technique concerning FOV and FOVR is presented in Table 3.
Secondary endpoints analysis
Chi square test showed that patients treated with proton therapy were more likely to have more locally advanced disease and larger PTV volumes in comparison with patients treated with photons (p < 0,001). Median FFLR was not reached in the whole series; two and three years FFLR were 83%. At univariate analysis, factors associated with worse FFLR were: proton therapy technique (versus photon technique p = 0.014), BED < 124 Gy (p = 0.004), presence of portal thrombosis (p = 0.003). No difference in local control emerged between patients treated with BED = 124Gy versus more than 124 Gy. In a subgroup analysis concerning BED, BED < 124 remained significantly related with poorer local control only in case of plans that meet target coverage criteria. Multivariate analysis confirmed BED < 124 Gy (OR 3.57 I.C. 1.1–11.5, p = 0.033) and portal vein thrombosis (OR 5.2, I.C. 1.1–24 p = 0.034) to be related with a poorer local control.
Median OS was 37,5 months in the whole series. Two- and three-years OS resulted in 61,4% and 52,9%. At univariate analysis, factors associated with poorer OS were female sex (p = 0.033), ECOG PS 2 (p < 0.001), proton technique (p < 0.001), GTV ≥ 9.4 cc (p < 0,001) and local control not achieved (p < 0.001). Multivariate analysis confirmed GTV ≥ 9.4 cc to be related with worse OS (OR 1.7, I.C. 1.05–3, p = 0,039).
RILD and acute and late toxicity
Acute toxicity was assessed for the entire population. Complete acute toxicity report is described in Table 4. Moreover, a proper evaluation for RILD diagnosis was available for 106 treatments. 2 cases of type 1 RILD were described in the cohort (one in PT group and one in a pts treated with V-MAT FF 10mm, both presented a GTV more than 150 cc); no type 2 RILD was described in the study. In both two cases symptoms were mild and resolved at 6 months. In 6 cases, an upgrade in Child–Pugh classification was registered in 6 patients (from A5 to A6) in four patients treated with PT and two patients treated with photons. Late toxicity was rare: one case of G3 cholangitis not certainly related to treatment occurred.
Discussion
Several dosimetric experiences demonstrated theoretically an improved plan quality with PT compared with photon SRT. The advantages were demonstrated in terms of reduced provisional dose to organs at risk. [28,29,30,31,32,33,34,35] Healthy liver sparing is routinely considered in both PT and SRT planning, using commonly published liver dose-constraints. However, the dose-constraint represented by volume respected by a certain dose (rVx) is strictly dependent by whole liver volume, and it is not a reliable parameter of dose fall-off quality [36]. Our study identified FOV and FOVR as instruments to better measure and compare plan quality in terms of healthy liver sparing. In fact, FOV is useful to quantify absolute fall-off plan quality (in cc), thus representing an instrument of both quality evaluation and optimization. FOVR constitutes an index of the extent of healthy liver injured by simply reporting standardized steepness of dose fall-off in relation to PTV.
Exploiting FOV and FOVR, our results shows that Cyberknife and V-MAT FFF 5mm are similar in liver sparing performance. For both, to treat a lesion it is expected to lose a volume 4–5 times bigger of the PTV itself. V-MAT-FF 10mm performed worse than other photons technique loosing approximately 6 times more healthy liver volume in relation to PTV. Despite based on limited data, PT plans seems to perform better than photons plans. Clinical consequences of such differences are not evident in our series and remain to be demonstrated.
Concerning efficacy, radiation dose remains crucial in predicting local control, with BED equal or higher to 124 Gy presenting an advantage in local control, as reported by other authors [37, 38]. Nevertheless, BED ≥ 124 Gy is not associated with an advantage in local control if plans do not meet target coverage objectives. Such result suggests that if plan does not meet ICRU 83 requirements, switching to a different schedule could be warranted. Remarkably, in our series no simultaneous integrated protection technique (SIP) was used [39, 40]. Comparison of local control and OS between techniques is biased by heterogeneity in patient characteristics. In fact, patients treated with PT had adverse features that could explain worse local control achieved and lower OS probability. Median BED in PT group was lower than 124 Gy, and an impact in local control could not be completely excluded. Remarkably, use of more biological effective schedules for PT is currently under investigation in clinical trials [41].
Our study presents some relevant limitations beside the obvious one due to its retrospective nature. A potential weakness is that the comparisons between PT and photon radiotherapy could be biased by the characteristics of PT patients, the small number of cases, and the small subgroup of PT patients that meet inclusion criteria concerning target coverage. Conversely, our results are more robust concerning comparison between different photon techniques, given the similar characteristics of patients and lesions.
Another limit is that FOV and FOVR and their implications are not applicable to lesions that arise less than 1 cm to liver surface and for FOVR, caution must be used in comparing plans with huge differences in PTV absolute volumes. Moreover, background liver health did not significantly impact on dose related to FLR, but caution must be applied in generalizing this conclusion, given the fact that the majority of cirrhotic patients in our series presented with Child–Pugh class A5 and this could explain the absence of a clear increase in radiosensitization of liver to a certain dose in comparison to healthy liver group.
Finally, the study has been conceived to present the potential role of FOV and FOVR in modern high dose liver RT. Their use, integrated with the classical dose-constraints, could contribute to refine RT planning in terms of healthy liver sparing. Whether such parameters could result in superior quality of plans is beyond the scope of this paper and remains to be demonstrated.
Despite these limitations, to our knowledge, our series try to address a critical issue poorly considered in liver high dose RT planning. In fact, taking into consideration parameters of liver damaged and not only liver spared is a new concept in liver radiotherapy, that could open new possibilities. FOV and FOVR could be integrated into modern radiotherapy planning with the aim to better measure and optimize liver sparing.
Conclusions
Our clinical MRI-based model shows that Robotic SRT with Cyberknife and V-MAT FFF 5mm spare more liver than V-MAT with FF 10mm. Our results suggest also that PT spares more healthy liver compared to photon SRT. FOV and FOVR are new tools to measure, optimize and compare quality of healthy liver sparing also in heterogeneous clinical situations. Demonstrating the clinical consequences of the integration of FOV and FOVR in modern RT planning is beyond the scope of our series, but better healthy liver sparing thanks to cutting edge techniques and advances in RT plan optimization may open the possibility to expand SRT and PT indications also in multifocal disease and treatment of metachronous lesions.
Data availability
Research data are stored in an institutional repository and will be shared upon request to the corresponding author.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 Countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Heimbach JK, Kulik LM, Finn RS et al (2018) AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67:358–380. https://doi.org/10.1002/hep.29086
NCCN (2022) NCCN clinical practice guidelines in oncology, https://www.nccn.org/professionals/physician_gls (2022, Accessed 15/04/2022)
Schwarz RE, Abou-Alfa GK, Geschwind JF et al (2010) Nonoperative therapies for combined modality treatment of hepatocellular cancer: expert consensus statement. HPB (Oxford) 12:313–320. https://doi.org/10.1111/j.1477-2574.2010.00183.x
Guha C, Kavanagh BD (2011) Hepatic radiation toxicity: avoidance and amelioration. Semin Radiat Oncol 21:256–263. https://doi.org/10.1016/j.semradonc.2011.05.003
Ingold JA, Reed GB, Kaplan HS et al (1965) Radiation hepatitis. Am J Roentgenol Radium Ther Nucl Med 93:200–208
Lawrence TS, Robertson JM, Anscher MS et al (1995) Hepatic toxicity resulting from cancer treatment. Int J Radiat Oncol Biol Phys 31:1237–1248. https://doi.org/10.1016/0360-3016(94)00418-k
Pan CC, Kavanagh BD, Dawson LA et al (2010) Radiation-associated liver injury. Int J Radiat Oncol Biol Phys 76:S94-100. https://doi.org/10.1016/j.ijrobp.2009.06.092
Reed GB Jr, Cox AJ Jr (1966) The human liver after radiation injury. A form of veno-occlusive disease. Am J Pathol 48:597–611
Dionisi F, Widesott L, Lorentini S et al (2014) Is there a role for proton therapy in the treatment of hepatocellular carcinoma? Syst Rev Radiother Oncol 111:1–10. https://doi.org/10.1016/j.radonc.2014.02.001
Potters L, Kavanagh B, Galvin JM et al (2010) American society for therapeutic radiology and oncology (ASTRO) and American college of radiology (ACR) practice guideline for the performance of stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys 76:326–332. https://doi.org/10.1016/j.ijrobp.2009.09.042
Qi WX, Fu S, Zhang Q et al (2015) Charged particle therapy versus photon therapy for patients with hepatocellular carcinoma: a systematic review and meta-analysis. Radiother Oncol 114:289–295. https://doi.org/10.1016/j.radonc.2014.11.033
Franzese C, Bonu ML, Comito T et al (2020) Stereotactic body radiotherapy in the management of oligometastatic and recurrent biliary tract cancer: single-institution analysis of outcome and toxicity. J Cancer Res Clin Oncol 146:2289–2297. https://doi.org/10.1007/s00432-020-03285-9
Kim N, Cheng J, Jung I et al (2020) Stereotactic body radiation therapy vs. radiofrequency ablation in Asian patients with hepatocellular carcinoma. J Hepatol 73:121–129. https://doi.org/10.1016/j.jhep.2020.03.005
Klement RJ, Guckenberger M, Alheid H et al (2017) Stereotactic body radiotherapy for oligo-metastatic liver disease—influence of pre-treatment chemotherapy and histology on local tumor control. Radiother Oncol 123:227–233. https://doi.org/10.1016/j.radonc.2017.01.013
Nicosia L, Cuccia F, Mazzola R et al (2020) Stereotactic body radiotherapy (SBRT) can delay polymetastatic conversion in patients affected by liver oligometastases. J Cancer Res Clin Oncol 146:2351–2358. https://doi.org/10.1007/s00432-020-03223-9
Winter JD, Wong R, Swaminath A et al (2015) Accuracy of robotic radiosurgical liver treatment throughout the respiratory cycle. Int J Radiat Oncol Biol Phys 93:916–924. https://doi.org/10.1016/j.ijrobp.2015.08.031
Wang X, Krishnan S, Zhang X et al (2008) Proton radiotherapy for liver tumors: dosimetric advantages over photon plans. Med Dosim 33:259–267. https://doi.org/10.1016/j.meddos.2007.04.008
Buglione M, Jereczek-Fossa BA, Bonù ML et al (2020) Radiosurgery and fractionated stereotactic radiotherapy in oligometastatic/oligoprogressive non-small cell lung cancer patients: results of a multi-institutional series of 198 patients treated with “curative” intent. Lung Cancer 141:1–8. https://doi.org/10.1016/j.lungcan.2019.12.019
Palma DA, Olson R, Harrow S et al (2019) Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomized, phase 2, open-label trial. Lancet 393:2051–2058. https://doi.org/10.1016/s0140-6736(18)32487-5
Triggiani L, Alongi F, Buglione M et al (2017) Efficacy of stereotactic body radiotherapy in oligorecurrent and in oligoprogressive prostate cancer: new evidence from a multicentric study. Br J Cancer 116:1520–1525. https://doi.org/10.1038/bjc.2017.103
Schwartz LH, Litière S, de Vries E et al (2016) RECIST 1.1-Update and clarification: from the RECIST committee. Eur J Cancer 62:132–137. https://doi.org/10.1016/j.ejca.2016.03.081
Jung SH, Yu JI, Park HC et al (2016) A feasibility study evaluating the relationship between dose and focal liver reaction in stereotactic ablative radiotherapy for liver cancer based on intensity change of Gd-EOB-DTPA-enhanced magnetic resonance images. Radiat Oncol J 34:64–75. https://doi.org/10.3857/roj.2016.34.1.64
Mastrocostas K, Jang HJ, Fischer S et al (2019) Imaging post-stereotactic body radiation therapy responses for hepatocellular carcinoma: typical imaging patterns and pitfalls. Abdom Radiol (NY) 44:1795–1807. https://doi.org/10.1007/s00261-019-01901-y
Kogel MJaAvd (2009) Basic clinical radiobiology 4th edition. Hodder Arnold
US Department of Health and Human Services NIoH, National cancer institute. Common terminology criteria for adverse events (CTCAE) Version 5: US department of health and human services
Pan CC, Kavanagh BD, Dawson LA, Li XA, Das SK, Miften M, Ten Haken RK (2010) Radiation-associated liver injury. Int J Radiat Oncol Biol Phys 76(3 Suppl):S94-100. https://doi.org/10.1016/j.ijrobp.2009.06.092.PMID:20171524;PMCID:PMC4388033
Arscott WT, Thompson RF, Yin L et al (2018) Stereotactic body proton therapy for liver tumors: dosimetric advantages and their radiobiological and clinical implications. Phys Imaging Radiat Oncol 8:17–22. https://doi.org/10.1016/j.phro.2018.11.004
Cheng JY, Liu CM, Wang YM et al (2020) Proton versus photon radiotherapy for primary hepatocellular carcinoma: a propensity-matched analysis. Radiat Oncol 15:159. https://doi.org/10.1186/s13014-020-01605-4
Cozzi L, Comito T, Loi M et al (2020) The potential role of intensity-modulated proton therapy in hepatic carcinoma in mitigating the risk of dose de-escalation. Technol Cancer Res Treat 19:1533033820980412. https://doi.org/10.1177/1533033820980412
Sun J, Wang Z, Sheng Y et al (2022) Indications of IMRT, PRT and CIRT for HCC from comparisons of dosimetry and normal tissue complication possibility. Strahlenther Onkol 198:361–369. https://doi.org/10.1007/s00066-021-01854-6
Hasan S, Abel S, Verma V et al (2019) Proton beam therapy versus stereotactic body radiotherapy for hepatocellular carcinoma: practice patterns, outcomes, and the effect of biologically effective dose escalation. J Gastrointest Oncol 10:999–1009. https://doi.org/10.21037/jgo.2019.08.03
Kim JY, Lim YK, Kim TH et al (2015) Normal liver sparing by proton beam therapy for hepatocellular carcinoma: Comparison with helical intensity modulated radiotherapy and volumetric modulated arc therapy. Acta Oncol 54:1827–1832. https://doi.org/10.3109/0284186x.2015.1009637
Toramatsu C, Katoh N, Shimizu S et al (2013) What is the appropriate size criterion for proton radiotherapy for hepatocellular carcinoma? A dosimetric comparison of spot-scanning proton therapy versus intensity-modulated radiation therapy. Radiat Oncol 8:48. https://doi.org/10.1186/1748-717x-8-48
Gandhi SJ, Liang X, Ding X et al (2015) Clinical decision tool for optimal delivery of liver stereotactic body radiation therapy: photons versus protons. Pract Radiat Oncol 5:209–218. https://doi.org/10.1016/j.prro.2015.01.004
Pollom EL, Chin AL, Diehn M et al (2017) Normal tissue constraints for abdominal and thoracic stereotactic body radiotherapy. Semin Radiat Oncol 27:197–208. https://doi.org/10.1016/j.semradonc.2017.02.001
Chang DT, Swaminath A, Kozak M et al (2011) Stereotactic body radiotherapy for colorectal liver metastases: a pooled analysis. Cancer 117:4060–4069. https://doi.org/10.1002/cncr.25997
Joo JH, Park JH, Kim JC et al (2017) Local control outcomes using stereotactic body radiation therapy for liver metastases from colorectal cancer. Int J Radiat Oncol Biol Phys 99:876–883. https://doi.org/10.1016/j.ijrobp.2017.07.030
Crane CH, Koay EJ (2016) Solutions that enable ablative radiotherapy for large liver tumors: fractionated dose painting, simultaneous integrated protection, motion management, and computed tomography image guidance. Cancer 122:1974–1986. https://doi.org/10.1002/cncr.29878
Bonù ML, Pedersoli G, Balduzzi J, Cefaratti M, Mataj E, Cossali G, Granello L, Singh N, Morelli V, Tomasini D, Frassine F, Vitali P, Terraneo F, Triggiani L, Buglione M, Magrini SM (2023) Stereotactic radiotherapy for critically located pancreatic and biliary targets: a review on simultaneous integrated protection and other dose-painting strategies to minimize dose to critical organs at risk. Radiation 3:98–109. https://doi.org/10.3390/radiation3020009
Oncology NRG (2022) National Cancer, I. Radiation therapy with protons or photons in treating patients with liver cancer. 579 Available online: https://ClinicalTrials.gov/show/NCT03186898 (Accessed on 27-07-2022)
Acknowledgements
We are grateful to Pixel Verona, Alberto Zizioli and the Fantini Bros. for support in images creation; we are grateful to Vittorio Morelli, Jacopo Balduzzi e Anastasia Domina for important help in follow-up and planning of patients.
Funding
Open access funding provided by Università degli Studi di Brescia within the CRUI-CARE Agreement. None.
Author information
Authors and Affiliations
Contributions
MLB, DT contributed to study conception, statistical analysis and writing; MB, SMM: statistical analysis and writing; LN, AT, PG, GC contributed to study conduction, data collection, contouring planning and delivery of treatments. PV, FF, EP, FB, PB, LT, AL contributed to data collection, contouring planning, follow up visits, manuscript review. ML, BF and LG contributed to staging of patients, biopsy of lesions, fiducial markers insertion and data collection. CT, LS contributed to treatment planning, manuscript review. NP contributed to biopsy, staging, data collection, manuscript review.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
Ethical committee approved such multi-institutional analysis. Practice number 5900.
Consent to participation
At the time of treatment, patients signed informed consent including the possibility to use anonymized data for study purpose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bonù, M.L., Nicosia, L., Turkaj, A. et al. High dose proton and photon-based radiation therapy for 213 liver lesions: a multi-institutional dosimetric comparison with a clinical perspective. Radiol med 129, 497–506 (2024). https://doi.org/10.1007/s11547-024-01788-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-024-01788-w