Abstract
Objective
To develop and validate an iodine maps-based radiomics nomogram for preoperatively predicting cervical lymph node metastasis (LNM) in head and neck squamous cell carcinoma (HNSCC).
Materials and methods
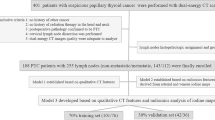
A total of 278 patients who pathologically confirmed as HNSCC were retrospectively recruited from two medical centers between June 2012 and July 2022. The training set (n = 152) and internal set (n = 67) were randomly selected from medical center A, and the patients from medical center B were enrolled as the external set (n = 69). The minority group in the training set was balanced by the adaptive synthetic sampling (ADASYN) approach. Radiomics features were extracted from dual-energy CT-derived iodine maps at arterial phase (AP) and venous phase (VP), respectively. Three radiomics signatures were constructed to predict the LNM by using a random forest algorithm. The independent clinical predictors for LNM were identified by multivariate analysis and combined with radiomics signatures to establish a radiomic–clinical nomogram. The performance of radiomic–clinical nomogram was evaluated with respect to its discrimination and clinical usefulness.
Results
The AP–VP-incorporated radiomics model exhibited a great predictive performance for LNM prediction with an area under curve (AUC) of 0.885 (95% CI, 0.836–0.933) in ADASYN-training set and confirmed in all validation sets. The nomogram that incorporated AP–VP radiomics signatures, CT-reported LN status, and histological grades yielded AUCs of 0.920 (95% CI, 0.881–0.959) in ADASYN-training set, 0.858 (95% CI, 0.771–0.944) in internal validation, and 0.849 (95% CI, 0.752–0.946) in external validation, with good calibration in all cohorts (p > 0.05). Decision curve analyses indicated the nomogram was clinically useful. In addition, the predictive performance of clinical–radiomics nomogram was also validation in combing cohorts. Stratified analysis confirmed the stability of nomogram, particularly in group negative for CT-reported LNM.
Conclusion
Clinical–radiomics nomogram based on iodine maps exhibited promising performance in predicting LNM and providing valuable information for making individualized therapy decisions.






Similar content being viewed by others
References
Chow LQM (2020) Head and neck cancer. N Engl J Med 382(1):60–72. https://doi.org/10.1056/NEJMra1715715
Plaxton NA, Brandon DC, Corey AS, Harrison CE, Karagulle Kendi AT, Halkar RK, Barron BJ (2015) Characteristics and limitations of FDG PET/CT for imaging of squamous cell carcinoma of the head and neck: a comprehensive review of anatomy, metastatic pathways, and image findings. AJR Am J Roentgenol 205(5):W519-531. https://doi.org/10.2214/AJR.14.12828
Nakamura T, Sumi M (2007) Nodal imaging in the neck: recent advances in US, CT and MR imaging of metastatic nodes. Eur Radiol 17(5):1235–1241. https://doi.org/10.1007/s00330-006-0490-0
Laimer J, Lauinger A, Steinmassl O, Offermanns V, Grams AE, Zelger B, Bruckmoser E (2020) Cervical lymph node metastases in oral squamous cell carcinoma-how much imaging do we need? Diagnostics (Basel). https://doi.org/10.3390/diagnostics10040199
Horvath A, Prekopp P, Polony G, Szekely E, Tamas L, Danos K (2021) Accuracy of the preoperative diagnostic workup in patients with head and neck cancers undergoing neck dissection in terms of nodal metastases. Eur Arch Otorhinolaryngol 278(6):2041–2046. https://doi.org/10.1007/s00405-020-06324-w
Kim JH, Choi KY, Lee SH, Lee DJ, Park BJ, Yoon DY, Rho YS (2020) The value of CT, MRI, and PET-CT in detecting retropharyngeal lymph node metastasis of head and neck squamous cell carcinoma. BMC Med Imaging 20(1):88. https://doi.org/10.1186/s12880-020-00487-y
Freihat O, Pinter T, Kedves A, Sipos D, Cselik Z, Repa I, Kovacs A (2020) Diffusion-Weighted Imaging (DWI) derived from PET/MRI for lymph node assessment in patients with head and neck squamous cell carcinoma (HNSCC). Cancer Imaging 20(1):56. https://doi.org/10.1186/s40644-020-00334-x
Chung MS, Choi YJ, Kim SO, Lee YS, Hong JY, Lee JH, Baek JH (2019) A scoring system for prediction of cervical lymph node metastasis in patients with head and neck squamous cell carcinoma. AJNR Am J Neuroradiol 40(6):1049–1054. https://doi.org/10.3174/ajnr.A6066
Hoang JK, Vanka J, Ludwig BJ, Glastonbury CM (2013) Evaluation of cervical lymph nodes in head and neck cancer with CT and MRI: tips, traps, and a systematic approach. AJR Am J Roentgenol 200(1):W17-25. https://doi.org/10.2214/AJR.12.8960
Colo AE, Simoes AC, Carvalho AL, Melo CM, Fahham L, Kowalski LP, Soares FA, Neves EJ, Reis LF, Carvalho AF (2011) Functional microarray analysis suggests repressed cell-cell signaling and cell survival-related modules inhibit progression of head and neck squamous cell carcinoma. BMC Med Genom 4:33. https://doi.org/10.1186/1755-8794-4-33
Flach GB, Tenhagen M, de Bree R, Brakenhoff RH, van der Waal I, Bloemena E, Kuik DJ, Castelijns JA, Leemans CR (2013) Outcome of patients with early stage oral cancer managed by an observation strategy towards the N0 neck using ultrasound guided fine needle aspiration cytology: no survival difference as compared to elective neck dissection. Oral Oncol 49(2):157–164. https://doi.org/10.1016/j.oraloncology.2012.08.006
Mayerhoefer ME, Materka A, Langs G, Haggstrom I, Szczypinski P, Gibbs P, Cook G (2020) Introduction to radiomics. J Nucl Med 61(4):488–495. https://doi.org/10.2967/jnumed.118.222893
Yu Y, He Z, Ouyang J, Tan Y, Chen Y, Gu Y, Mao L, Ren W, Wang J, Lin L, Wu Z, Liu J, Ou Q, Hu Q, Li A, Chen K, Li C, Lu N, Li X, Su F, Liu Q, Xie C, Yao H (2021) Magnetic resonance imaging radiomics predicts preoperative axillary lymph node metastasis to support surgical decisions and is associated with tumor microenvironment in invasive breast cancer: a machine learning, multicenter study. EBioMedicine 69:103460. https://doi.org/10.1016/j.ebiom.2021.103460
van Griethuysen JJM, Fedorov A, Parmar C, Hosny A, Aucoin N, Narayan V, Beets-Tan RGH, Fillion-Robin JC, Pieper S, Aerts H (2017) Computational radiomics system to decode the radiographic phenotype. Cancer Res 77(21):e104–e107. https://doi.org/10.1158/0008-5472.CAN-17-0339
Peng Z, Wang Y, Wang Y, Jiang S, Fan R, Zhang H, Jiang W (2021) Application of radiomics and machine learning in head and neck cancers. Int J Biol Sci 17(2):475–486. https://doi.org/10.7150/ijbs.55716
Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J, Sanduleanu S, Larue R, Even AJG, Jochems A, van Wijk Y, Woodruff H, van Soest J, Lustberg T, Roelofs E, van Elmpt W, Dekker A, Mottaghy FM, Wildberger JE, Walsh S (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 14(12):749–762. https://doi.org/10.1038/nrclinonc.2017.141
Zhou Y, Su GY, Hu H, Tao XW, Ge YQ, Si Y, Shen MP, Xu XQ, Wu FY (2022) Radiomics from primary tumor on dual-energy CT derived iodine maps can predict cervical lymph node metastasis in papillary thyroid cancer. Acad Radiol 29(Suppl 3):S222–S231. https://doi.org/10.1016/j.acra.2021.06.014
Li J, Dong D, Fang M, Wang R, Tian J, Li H, Gao J (2020) Dual-energy CT-based deep learning radiomics can improve lymph node metastasis risk prediction for gastric cancer. Eur Radiol 30(4):2324–2333. https://doi.org/10.1007/s00330-019-06621-x
Zhao X, Li W, Zhang J, Tian S, Zhou Y, Xu X, Hu H, Lei D, Wu F (2023) Radiomics analysis of CT imaging improves preoperative prediction of cervical lymph node metastasis in laryngeal squamous cell carcinoma. Eur Radiol 33(2):1121–1131. https://doi.org/10.1007/s00330-022-09051-4
Sananmuang T, Agarwal M, Maleki F, Muthukrishnan N, Marquez JC, Chankowsky J, Forghani R (2020) Dual energy computed tomography in head and neck imaging: pushing the envelope. Neuroimaging Clin N Am 30(3):311–323. https://doi.org/10.1016/j.nic.2020.04.003
Foust AM, Ali RM, Nguyen XV, Agrawal A, Prevedello LM, Bourekas EC, Boulter DJ (2018) Dual-energy CT-derived iodine content and spectral attenuation analysis of metastatic versus nonmetastatic lymph nodes in squamous cell carcinoma of the oropharynx. Tomography 4(2):66–71. https://doi.org/10.18383/j.tom.2018.00009
Luo YH, Mei XL, Liu QR, Jiang B, Zhang S, Zhang K, Wu X, Luo YM, Li YJ (2023) Diagnosing cervical lymph node metastasis in oral squamous cell carcinoma based on third-generation dual-source, dual-energy computed tomography. Eur Radiol 33(1):162–171. https://doi.org/10.1007/s00330-022-09033-6
Tawfik AM, Razek AA, Kerl JM, Nour-Eldin NE, Bauer R, Vogl TJ (2014) Comparison of dual-energy CT-derived iodine content and iodine overlay of normal, inflammatory and metastatic squamous cell carcinoma cervical lymph nodes. Eur Radiol 24(3):574–580. https://doi.org/10.1007/s00330-013-3035-3
Lenga L, Bernatz S, Martin SS, Booz C, Solbach C, Mulert-Ernst R, Vogl TJ, Leithner D (2021) Iodine map radiomics in breast cancer: prediction of metastatic status. Cancers (Basel) 13(10):2431. https://doi.org/10.3390/cancers13102431
Forghani R, Chatterjee A, Reinhold C, Perez-Lara A, Romero-Sanchez G, Ueno Y, Bayat M, Alexander JWM, Kadi L, Chankowsky J, Seuntjens J, Forghani B (2019) Head and neck squamous cell carcinoma: prediction of cervical lymph node metastasis by dual-energy CT texture analysis with machine learning. Eur Radiol 29(11):6172–6181. https://doi.org/10.1007/s00330-019-06159-y
Huang SH, O’Sullivan B (2017) Overview of the 8th edition TNM classification for head and neck cancer. Curr Treat Options Oncol 18(7):40. https://doi.org/10.1007/s11864-017-0484-y
Yang B, Zhou L, Zhong J, Lv T, Li A, Ma L, Zhong J, Yin S, Huang L, Zhou C, Li X, Ge YQ, Tao X, Zhang L, Son Y, Lu G (2021) Combination of computed tomography imaging-based radiomics and clinicopathological characteristics for predicting the clinical benefits of immune checkpoint inhibitors in lung cancer. Respir Res 22(1):189. https://doi.org/10.1186/s12931-021-01780-2
Patel SG, Amit M, Yen TC, Liao CT, Chaturvedi P, Agarwal JP, Kowalski LP, Ebrahimi A, Clark JR, Cernea CR, Brandao SJ, Kreppel M, Zoller J, Fliss D, Fridman E, Bachar G, Shpitzer T, Bolzoni VA, Patel PR, Jonnalagadda S, Robbins KT, Shah JP, Gil Z, International Consortium for Outcome Research in H, Neck C (2013) Lymph node density in oral cavity cancer: results of the international consortium for outcomes research. Br J Cancer 109(8):2087–2095. https://doi.org/10.1038/bjc.2013.570
Sun J, Li B, Li CJ, Li Y, Su F, Gao QH, Wu FL, Yu T, Wu L, Li LJ (2015) Computed tomography versus magnetic resonance imaging for diagnosing cervical lymph node metastasis of head and neck cancer: a systematic review and meta-analysis. Onco Targets Ther 8:1291–1313. https://doi.org/10.2147/OTT.S73924
de Bondt RB, Nelemans PJ, Hofman PA, Casselman JW, Kremer B, van Engelshoven JM, Beets-Tan RG (2007) Detection of lymph node metastases in head and neck cancer: a meta-analysis comparing US, USgFNAC, CT and MR imaging. Eur J Radiol 64(2):266–272. https://doi.org/10.1016/j.ejrad.2007.02.037
Jiang L, You C, Xiao Y, Wang H, Su GH, Xia BQ, Zheng RC, Zhang DD, Jiang YZ, Gu YJ, Shao ZM (2022) Radiogenomic analysis reveals tumor heterogeneity of triple-negative breast cancer. Cell Rep Med 3(7):100694. https://doi.org/10.1016/j.xcrm.2022.100694
Dong D, Fang MJ, Tang L, Shan XH, Gao JB, Giganti F, Wang RP, Chen X, Wang XX, Palumbo D, Fu J, Li WC, Li J, Zhong LZ, De Cobelli F, Ji JF, Liu ZY, Tian J (2020) Deep learning radiomic nomogram can predict the number of lymph node metastasis in locally advanced gastric cancer: an international multicenter study. Ann Oncol 31(7):912–920. https://doi.org/10.1016/j.annonc.2020.04.003
Greffier J, Villani N, Defez D, Dabli D, Si-Mohamed S (2022) Spectral CT imaging: technical principles of dual-energy CT and multi-energy photon-counting CT. Diagn Interv Imaging. https://doi.org/10.1016/j.diii.2022.11.003
Wang L, Zhang Y, Chen Y, Tan J, Wang L, Zhang J, Yang C, Ma Q, Ge Y, Xu Z, Pan Z, Du L, Yan F, Yao W, Zhang H (2020) The performance of a dual-energy CT derived radiomics model in differentiating serosal invasion for advanced gastric cancer patients after neoadjuvant chemotherapy: iodine map combined with 120-kV equivalent mixed images. Front Oncol 10:562945. https://doi.org/10.3389/fonc.2020.562945
Xue C, Yuan J, Lo GG, Chang ATY, Poon DMC, Wong OL, Zhou Y, Chu WCW (2021) Radiomics feature reliability assessed by intraclass correlation coefficient: a systematic review. Quant Imaging Med Surg 11(10):4431–4460. https://doi.org/10.21037/qims-21-86
Xu XQ, Zhou Y, Su GY, Tao XW, Ge YQ, Si Y, Shen MP, Wu FY (2022) Iodine maps from dual-energy CT to predict extrathyroidal extension and recurrence in papillary thyroid cancer based on a radiomics approach. AJNR Am J Neuroradiol 43(5):748–755. https://doi.org/10.3174/ajnr.A7484
Zhang Y, Yu J, Zhu H (2022) Risk factors for cervical lymph node metastasis of head and neck squamous cell carcinoma: a retrospective population-based study. J Stomatol Oral Maxillofac Surg 123(5):e484–e488. https://doi.org/10.1016/j.jormas.2022.05.001
Ai QYH, So TY, Hung KF, King AD (2022) Normal size of benign upper neck nodes on MRI: parotid, submandibular, occipital, facial, retroauricular and level IIb nodal groups. Cancer Imaging 22(1):66. https://doi.org/10.1186/s40644-022-00504-z
Kann BH, Likitlersuang J, Bontempi D, Ye Z, Aneja S, Bakst R, Kelly HR, Juliano AF, Payabvash S, Guenette JP, Uppaluri R, Margalit DN, Schoenfeld JD, Tishler RB, Haddad R, Aerts H, Garcia JJ, Flamand Y, Subramaniam RM, Burtness BA, Ferris RL (2023) Screening for extranodal extension in HPV-associated oropharyngeal carcinoma: evaluation of a CT-based deep learning algorithm in patient data from a multicentre, randomised de-escalation trial. Lancet Digit Health 5(6):e360–e369. https://doi.org/10.1016/S2589-7500(23)00046-8
Feng M, Zhang J, Zhou X, Mo H, Jia L, Zhang C, Hu Y, Yuan W (2022) Application of an interpretable machine learning model to predict lymph node metastasis in patients with laryngeal carcinoma. J Oncol 2022:6356399. https://doi.org/10.1155/2022/6356399
Lu S, Ling H, Chen J, Tan L, Gao Y, Li H, Tan P, Huang D, Zhang X, Liu Y, Mao Y, Qiu Y (2022) MRI-based radiomics analysis for preoperative evaluation of lymph node metastasis in hypopharyngeal squamous cell carcinoma. Front Oncol 12:936040. https://doi.org/10.3389/fonc.2022.936040
Saenthaveesuk P, Yang L, Zeng B, Xu M, Young S, Liao G, Liang Y (2021) Development and validation of multiparametric MRI-based nomogram for predicting occult metastasis risk in early tongue squamous cell carcinoma. BMC Cancer 21(1):408. https://doi.org/10.1186/s12885-021-08135-6
Cebeci S, Aydos U, Yeniceri A, Pula D, Duzlu M, Atay LO, Yilmaz M (2023) Diagnostic performance of FDG PET/MRI for cervical lymph node metastasis in patients with clinically N0 head and neck cancer. Eur Rev Med Pharmacol Sci 27(10):4528–4535. https://doi.org/10.26355/eurrev_202305_32459
McCollough CH, Leng S, Yu L, Fletcher JG (2015) Dual- and multi-energy CT: principles, technical approaches, and clinical applications. Radiology 276(3):637–653. https://doi.org/10.1148/radiol.2015142631
Yuan Y, Ren J, Tao X (2021) Machine learning-based MRI texture analysis to predict occult lymph node metastasis in early-stage oral tongue squamous cell carcinoma. Eur Radiol 31(9):6429–6437. https://doi.org/10.1007/s00330-021-07731-1
Acknowledgements
The authors would like to thank Dr. Siyun Liu (GE Healthcare, Beijing) for data analysis and statistical support.
Funding
This work was supported by the Natural Science Foundation of China (No. 81960310).
Author information
Authors and Affiliations
Contributions
WZ and JL contributed to this study equally. The study conception and design were directed by DH. Material preparation and data collection and analysis were performed by WZ, JL, WFJ, RL, XX, WZ, and SX. The first draft of the manuscript was written by WZ, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest to disclose.
Ethical approval
This retrospective study was approved by the institutional review board at The First Affiliated Hospital of Kunming Medical University, and the informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, W., Liu, J., Jin, W. et al. Radiomics from dual-energy CT-derived iodine maps predict lymph node metastasis in head and neck squamous cell carcinoma. Radiol med 129, 252–267 (2024). https://doi.org/10.1007/s11547-023-01750-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-023-01750-2