Abstract
Purpose
To assess the role of 2D-shear wave elastography (2D-SWE) in differentiating benign from malignant focal breast lesions (FBLs), providing new vendor-specific cutoff values.
Methods
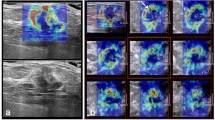
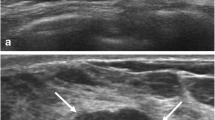
158 FBLs (size: 3.5–50 mm) detected in 151 women (age: 21–87 years) were prospectively evaluated by means 2D-SWE. For each lesion, an expert radiologist assessed US BI-RADS category and calculated the following four 2D-SWE parameters: (1) elasticity maximum (Emax); (2) mean elasticity (Emean); (3) minimum elasticity (Emin); (4) elasticity ratio (Eratio). US-guided core-biopsy was considered as standard of reference for all the FBLs classified as BI-RADS 4 or 5. For each 2D-SWE parameter, the optimal cutoff value for a diagnostic test was calculated using the Youden method. Diagnostic performance of the US BI-RADS and 2D-SWE parameters was calculated accordingly.
Results
83/158 (52.5%) FBLs were benign and 75/158 (47.5%) were malignant. Statistically significant higher stiffness values were observed in malignant FBLs for all 2D-SWE parameters than in benign ones (p < 0.001). 2D-SWE cutoff values were 82.6 kPa, 66.0 kPa and 53.6 kPa, respectively, for Emax, Emean, Emin and 330.8% for Eratio. The 2D-SWE parameter showing the best diagnostic accuracy was Emax (85.44%). Considering US BI-RADS 3 (n = 60) and 4a (n = 32) FBLs, Emax and Emean showed the best diagnostic accuracy (85.87% for both), without a statistically significant decrease in sensitivity (p = 0.7003 and p = 1, respectively).
Conclusion
Our study provides new vendor-specific cutoff values for 2D-SWE, suggesting its possible clinical use in the adjunctive assessment of category US-BI-RADS 3 and 4a breast masses.





Similar content being viewed by others
References
Krouskop TA, Dougherty DR, Vinson FS (1987) A pulsed Doppler ultrasonic system for making noninvasive measurements of the mechanical properties of soft tissue. J Rehabil Res Dev 24(2):1–8
Ginat DT, Destounis SV, Barr RG et al (2009) US elastography of breast and prostate lesions. Radiographics 29(7):2007–2016
Lee J, Kang HJ, Yoon JH et al (2021) Ultrasound-guided transient elastography and two-dimensional shear wave elastography for assessment of liver fibrosis: emphasis on technical success and reliable measurements. Ultrasonography 40(2):217–227. https://doi.org/10.14366/usg.20036
Bamber J, Cosgrove D, Dietrich CF et al (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: Basic principles and technology. Ultraschall Med 34(2):169–184. https://doi.org/10.1055/s-0033-1335205
Sezgin G, Coskun M, Apaydin M et al (2021) The role of rare breast cancers in the false negative strain elastography results. Radiol Med 126(3):349–355. https://doi.org/10.1007/s11547-020-01270-3
Bartolotta TV, Ienzi R, Cirino A et al (2011) Characterisation of indeterminate focal breast lesions on grey-scale ultrasound: role of ultrasound elastography. Radiol Med 116(7):1027–1038. https://doi.org/10.1007/s11547-011-0648-y
Youk JH, Gweon HM, Son EJ (2017) Shear-wave elastography in breast ultrasonography: the state of the art. Ultrasonography 36(4):300–309. https://doi.org/10.14366/usg.17024
Berg WA, Cosgrove DO, Doré CJ et al (2012) Shear-wave elastography improves the specificity of breast US: the BE1 multinational study of 939 masses. Radiology 262(2):435–449
Park SY, Kang BJ (2021) Combination of shear-wave elastography with ultrasonography for detection of breast cancer and reduction of unnecessary biopsies: a systematic review and meta-analysis. Ultrasonography 40(3):318–332. https://doi.org/10.14366/usg.20058
Balleyguier C, Canale S, Ben Hassen W et al (2013) Breast elasticity: principles, technique, results: an update and overview of commercially available software. Eur J Radiol 82(3):427–434. https://doi.org/10.1016/j.ejrad.2012.03.001
Au FW, Ghai S, Moshonov H et al (2014) Diagnostic performance of quantitative shear wave elastography in the evaluation of solid breast masses: determination of the most discriminatory parameter. AJR Am J Roentgenol 203(3):W328–W336
Kim H, Lee J, Kang BJ et al (2021) What shear wave elastography parameter best differentiates breast cancer and predicts its histologic aggressiveness? Ultrasonography 40(2):265–273. https://doi.org/10.14366/usg.20007
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310(20):2191–2194
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Dietrich CF, Bamber J, Berzigotti A et al (2017) EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (Long Version). Ultraschall Med 38(4):e16–e47. https://doi.org/10.1055/s-0043-103952
Mendelson E, Bohm-Velez M et al (2013) ACR BI- RADS Ultrasound. ACR BI-RADS atlas, breast imaging reporting and data system. Reston, VA: American College of Radiology [1–153]
Săftoiu A, Gilja OH, Sidhu PS et al (2019) The EFSUMB guidelines and recommendations for the clinical practice of elastography in non-hepatic applications: update 2018. Ultraschall Med 40(4):425–445. https://doi.org/10.1055/a-0838-9937
Barr RG, Nakashima K, Amy D et al (2015) WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 2: breast. Ultrasound Med Biol 41:1148–1160
Pesce K, Binder F, Chico MJ et al (2020) Diagnostic performance of shear wave elastography in discriminating malignant and benign breast lesions: our experience with QelaXtoTM software. J Ultrasound 23(4):575–583. https://doi.org/10.1007/s40477-020-00481-8
Wang ZL, Li JL, Li M et al (2013) Study of quantitative elastography with supersonic shear imaging in the diagnosis of breast tumours. Radiol Med 118(4):583–590. https://doi.org/10.1007/s11547-012-0903-x
Lee EJ, Jung HK, Ko KH et al (2013) Diagnostic performances of shear wave elastography: which parameter to use in differential diagnosis of solid breast masses? Eur Radiol 23(7):1803–1811. https://doi.org/10.1007/s00330-013-2782-5
Ko KH, Jung HK, Kim SJ et al (2014) Potential role of shear-wave ultrasound elastography for the differential diagnosis of breast non-mass lesions: preliminary report. Eur Radiol 24(2):305–311. https://doi.org/10.1007/s00330-013-3034-4
Shi XQ, Li JL, Wan WB et al (2015) A set of shear wave elastography quantitative parameters combined with ultrasound BI-RADS to assess benign and malignant breast lesions. Ultrasound Med Biol 41(4):960–966. https://doi.org/10.1016/j.ultrasmedbio.2014.11.014
Park J, Woo OH, Shin HS et al (2015) Diagnostic performance and color overlay pattern in shear wave elastography (SWE) for palpable breast mass. Eur J Radiol 84(10):1943–1948. https://doi.org/10.1016/j.ejrad.2015.06.020
Ganau S, Andreu FJ, Escribano F et al (2015) Shear-wave elastography and immunohistochemical profiles in invasive breast cancer: evaluation of maximum and mean elasticity values. Eur J Radiol 84(4):617–622. https://doi.org/10.1016/j.ejrad.2014.12.020
Elseedawy M, Whelehan P, Vinnicombe S et al (2016) Factors influencing the stiffness of fibroadenomas at shearwave elastography. ClinRadiol 71(1):92–95
Abdelwahab K, Hamdy O, Zaky M et al (2017) Breast fibromatosis, an unusual breast disease. J Surg Case Rep 2017(12):rjx248. https://doi.org/10.1093/jscr/rjx248
Ganau S, Frigola G, Bargalló X et al (2019) Breast fibromatosis: Variability among imaging methods. Breast J 25(4):750–752. https://doi.org/10.1111/tbj.13320
Toprak N, Gündüz AM, Çelik S (2018) Evaluation of giant galactocele with ultrasound and shearwave elastography findings. East J Med 23(4):338–340
Song EJ, Sohn YM, Seo M (2018) Diagnostic performances of shear-wave elastography and B-mode ultrasound to differentiate benign and malignant breast lesions: the emphasis on the cutoff value of qualitative and quantitative parameters. Clin Imaging 50:302–307. https://doi.org/10.1016/j.clinimag.2018.05.007
Altıntas Y, Bayrak M, Alabaz Ö et al (2021) A qualitative and quantitative assessment of simultaneous strain, shear wave, and point shear wave elastography to distinguish malignant and benign breast lesions. Acta Radiol 62(9):1155–1162. https://doi.org/10.1177/0284185120961422
Jia W, Luo T, Dong Y et al (2021) Breast elasticity imaging techniques: comparison of strain elastography and shear-wave elastography in the same population. Ultrasound Med Biol 47(1):104–113. https://doi.org/10.1016/j.ultrasmedbio.2020.09.022
Lee BE, Chung J, Cha ES et al (2015) Role of shear-wave elastography (SWE) in complex cystic and solid breast lesions in comparison with conventional ultrasound. Eur J Radiol 84(7):1236–1241. https://doi.org/10.1016/j.ejrad.2015.04.005
Lee EJ, Chang YW (2020) Combination of quantitative parameters of shear wave elastography and superb microvascular imaging to evaluate breast masses. Korean J Radiol 21(9):1045–1054
Barr RG (2019) Future of breast elastography. Ultrasonography 38(2):93–105. https://doi.org/10.14366/usg.18053
Choi HY, Seo M, Sohn YM et al (2019) Shear wave elastography for the diagnosis of small (≤2 cm) breast lesions: added value and factors associated with false results. Br J Radiol 92(1097):20180341. https://doi.org/10.1259/bjr.20180341
Kim SJ, Ko KH, Jung HK et al (2015) Shear wave elastography: is it a valuable additive method to conventional ultrasound for the diagnosis of small (≤2 cm) breast cancer? Medicine (Baltimore) 94(42):e1540
Seo M, Ahn HS, Park SH et al (2018) Comparison and combination of strain and shear wave elastography of breast masses for differentiation of benign and malignant lesions by quantitative assessment: preliminary study. J Ultrasound Med 37(1):99–109. https://doi.org/10.1002/jum.14309
Youk JH, Son EJ, Gweon HM et al (2014) Comparison of strain and shear wave elastography for the differentiation of benign from malignant breast lesions, combined with B-mode ultrasonography: qualitative and quantitative assessments. Ultrasound Med Biol 40(10):2336–2344. https://doi.org/10.1016/j.ultrasmedbio.2014.05.020
Hong S, Woo OH, Shin HS et al (2017) Reproducibility and diagnostic performance of shear wave elastography in evaluating breast solid mass. Clin Imaging 44:42–45. https://doi.org/10.1016/j.clinimag.2017.03.022
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
TVB, AAMO and DM contributed to the study conception and design. Material preparation, data collection and analysis were performed by TVB, AAMO, MD, AC, CZ, FF and SV. The first draft of the manuscript was written by TVB, AAMO and DM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.”
Corresponding author
Ethics declarations
Conflict of interest
Tommaso Vincenzo Bartolotta is lecturer and scientific advisor for Samsung. Other authors declare that they have no conflict of interest. This research was supported by research equipment from SAMSUNG MEDISON Co., Ltd.
Ethical approval
Institutional ethical committee approval was obtained, and full written informed consent was obtained for this prospective study. Our study complied with the terms of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bartolotta, T.V., Orlando, A.A.M., Dimarco, M. et al. Diagnostic performance of 2D-shear wave elastography in the diagnosis of breast cancer: a clinical appraisal of cutoff values. Radiol med 127, 1209–1220 (2022). https://doi.org/10.1007/s11547-022-01546-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01546-w