Abstract
Purpose
To identify the risk factors associated with patency loss after bailout stenting with third-generation hybrid heparin-bonded nitinol stent of the femoropopliteal segment.
Methods
Prospective, multicenter, single-arm registry including 156 patients (50 females, mean age 72 ± 11 years) subjected, from February 2017 to December 2018, to provisional stenting with Gore Tigris vascular stent of the distal superficial femoral artery, with or without involvement of the popliteal artery, in 9 different centers. The 194 lesions, with Rutherford score ≥ 3, were stented in case of recoil, dissection or residual stenosis not responding to percutaneous trans-luminal angioplasty (PTA). The follow-up (FU) was performed with clinical evaluation and duplex ultrasound (DUS) at 1, 6 and 12 months.
Results
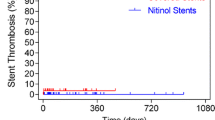
The primary patency rate was 99(95%CI 98–100)% at 1 month, 86(80–92)% at 6 months and 81(74–88)% at-12 months. After patency loss, 13/23 (56.5%) patients were re-treated, yielding a primary assisted patency of 91(86–96)% at 6 months and 88(82–94)% at 12 months and a secondary patency of 94(90–98)% at 6 months and 90(84–95)% at 12 months. Rutherford score ≥ 4 (p = 0.03) and previous severe treatments (p = 0.01) were identified as risk factors for early patency loss during FU. The involvement of the popliteal artery was not an independent risk factor for loss of patency.
Conclusions
The bailout stenting of the femoropopliteal segment with third-generation nitinol stents is a safe and effective option in case of recoil, dissection or residual stenosis not responding to PTA. Critical limb ischemia and history of previous major treatment at the same level are significant prognostic factors for patency loss during FU.



Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Shu J, Santulli G (2018) Update on peripheral artery disease: epidemiology and evidence-based facts. Atherosclerosis 275:379–381. https://doi.org/10.1016/j.atherosclerosis.2018.05.033
Fowkes FGR, Rudan D, Rudan I et al (2013) Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. The Lancet 382:1329–1340. https://doi.org/10.1016/S0140-6736(13)61249-0
Kasapis C, Gurm HS (2009) Current approach to the diagnosis and treatment of femoral-popliteal arterial disease a systematic review. Curr Cardiol Rev 5:296–311. https://doi.org/10.2174/157340309789317823
Norgren L, Hiatt WR, Dormandy JA et al (2007) Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 45:S5-67. https://doi.org/10.1016/j.jvs.2006.12.037
Hirsch AT, Haskal ZJ, Hertzer NR et al (2006) ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 113:e463-654. https://doi.org/10.1161/CIRCULATIONAHA.106.174526
Iida O, Yokoi H, Soga Y et al (2013) Cilostazol reduces angiographic restenosis after endovascular therapy for femoropopliteal lesions in the sufficient treatment of peripheral intervention by cilostazol study. Circulation 127:2307–2315. https://doi.org/10.1161/CIRCULATIONAHA.112.000711
Schillinger M, Sabeti S, Loewe C et al (2006) Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med 354:1879–1888. https://doi.org/10.1056/NEJMoa051303
Sabeti S, Mlekusch W, Amighi J et al (2005) Primary patency of long-segment self-expanding nitinol stents in the femoropopliteal arteries. J Endovasc Ther Off J Int Soc Endovasc Spec 12:6–12. https://doi.org/10.1583/04-1359.1
Lugmayr HF, Holzer H, Kastner M et al (2002) Treatment of complex arteriosclerotic lesions with nitinol stents in the superficial femoral and popliteal arteries: a midterm follow-up. Radiology 222:37–43. https://doi.org/10.1148/radiol.2221010268
Sabeti S, Schillinger M, Amighi J et al (2004) Primary patency of femoropopliteal arteries treated with nitinol versus stainless steel self-expanding stents: propensity score-adjusted analysis. Radiology 232:516–521. https://doi.org/10.1148/radiol.2322031345
Scheinert D, Scheinert S, Sax J et al (2005) Prevalence and clinical impact of stent fractures after femoropopliteal stenting. J Am Coll Cardiol 45:312–315. https://doi.org/10.1016/j.jacc.2004.11.026
Laird JR, Katzen BT, Scheinert D et al (2012) Nitinol stent implantation vs. balloon angioplasty for lesions in the superficial femoral and proximal popliteal arteries of patients with claudication: three-year follow-up from the RESILIENT randomized trial. J Endovasc Ther Off J Int Soc Endovasc Spec 19:1–9. https://doi.org/10.1583/11-3627.1
Sibé M, Kaladji A, Boirat C et al (2017) French multicenter experience with the GORE TIGRIS Vascular Stent in superficial femoral and popliteal arteries. J Vasc Surg 65:1329–1335. https://doi.org/10.1016/j.jvs.2016.11.056
Piorkowski M, Freitas B, Steiner S et al (2015) Twelve-month experience with the GORE® TIGRIS® Vascular Stent in the superficial femoral and popliteal arteries. J Cardiovasc Surg (Torino) 56:89–95
Lucatelli P, Cini M, Tommasino G et al (2018) Use of the gore tigris vascular stent in advanced femoropopliteal peripheral arterial disease. J Vasc Interv Radiol JVIR 29:614–622. https://doi.org/10.1016/j.jvir.2017.12.006
Parthipun A, Diamantopoulos A, Kitrou P et al (2015) Use of a new hybrid heparin-bonded nitinol ring stent in the popliteal artery: procedural and mid-term clinical and anatomical outcomes. Cardiovasc Interv Radiol 38:846–854. https://doi.org/10.1007/s00270-015-1113-4
Laird JR, Zeller T, Loewe C et al (2018) Novel nitinol stent for lesions up to 24 cm in the superficial femoral and proximal popliteal arteries: 24-month results from the TIGRIS randomized trial. J Endovasc Ther Off J Int Soc Endovasc Spec 25:68–78. https://doi.org/10.1177/1526602817749242
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study was approved by the local Ethics Committee of all participating centers (protocol number of the site principal investigator: 0038779). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ruffino, M.A., Fronda, M., Bergamasco, L. et al. Prognostic risk factors for loss of patency after femoropopliteal bailout stenting with dual-component stent: results from the TIGRIS Italian Multicenter Registry. Radiol med 126, 1129–1137 (2021). https://doi.org/10.1007/s11547-021-01373-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-021-01373-5