Abstract
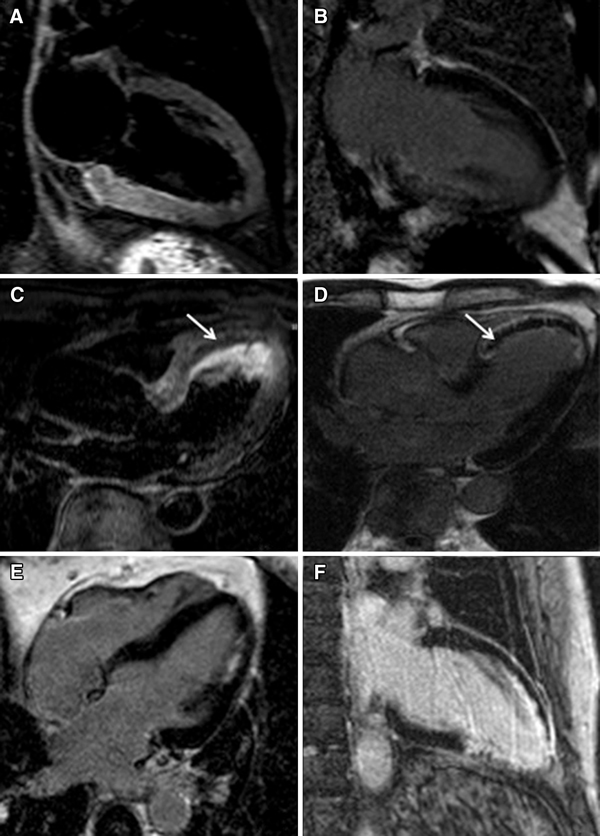
Cardiovascular magnetic resonance has always been more often used in the last 10 years in evaluation of heart disease. Role in diagnosis of ischemia and in evaluation of myocardial infarction is well established by many scientific papers and included in current guidelines. High accuracy in evaluation of stress-induced ischemia, tissue characterization and functional parameters are the pillars the make the method widely used. In this paper are described role and techniques in diagnosis of ischemia, myocardial infarction and its sequelae.


Similar content being viewed by others
References
Di Cesare E, Cademartiri F, Carbone I et al (2013) Clinical indications for the use of cardiac MRI. By the SIRM study Group on Cardiac Imaging. Radiol Med 118(5):752–798. https://doi.org/10.1007/s11547-012-0899-2
Francone M, Di Cesare E, Cademartini F et al (2014) Italian Registry of cardiac magnetic resonance. Eur J Radiol 83(1):e15–e22. https://doi.org/10.1016/j.ejrad.2013.10.006
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD (2019) ESC Scientific Document Group. Fourth universal definition of myocardial infarction. Eur Heart J 40:237–269
Sarkisian L, Saaby L, Poulsen TS, Gerke O, Jangaard N, Hosbond S, Diederichsen ACP, Thygesen K, Mickley H (2016) Clinical characteristics and outcomes of patients with myocardial infarction, myocardial injury, and nonelevated troponins. Am J Med 129:446e.5–446e.21
Sarkisian L, Saaby L, Poulsen TS, Gerke O, Hosbond S, Jangaard N, Diederichsen ACP, Thygesen K, Mickley H (2016) Prognostic impact of myocardial injury related to various cardiac and noncardiac conditions. Am J Med 129:506–514
Ooi DS, Isotalo PA, Veinot JP (2000) Correlation of antemortem serum creatine kinase, creatine kinase-MB, troponin I, and troponin T with cardiac pathology. Clin Chem 46:338–344
Secchi F, Ali M, Petrini M et al (2018) Blood-threshold CMR volume analysis of functional univentricular heart. Radiol Med 123:331–337. https://doi.org/10.1007/s11547-017-0851-6
Burns RJ, Gibbons RJ, Yi Q, Roberts RS, Miller TD, Schaer GL, Anderson JL, Yusuf S (2002) The relationships of left ventricular ejection fraction, end-systolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis. J Am Coll Cardiol 39:30–36
El Aidi H, Adams A, Moons KG, Den Ruijter HM, Mali WP, Doevendans PA, Nagel E, Schalla S, Bots ML, Leiner T (2014) Cardiac magnetic resonance imaging findings and the risk of cardiovascular events in patients with recent myocardial infarction or suspected or known coronary artery disease: a systematic review of prognostic studies. J Am Coll Cardiol 63:1031–1045
Reindl M, Tiller C, Holzknecht M, Lechner I, Beck A, Plappert D, Gorzala M, Pamminger M, Mayr A, Klug G et al (2019) Prognostic implications of global longitudinal strain by feature-tracking cardiac magnetic resonance in ST-elevation myocardial infarction. Circ Cardiovasc Imaging 12:e009404
Ibanez B, Aletras AH, Arai AE, Arheden H, Bax J, Berry C, Bucciarelli-Ducci C, Croisille P, Dall’Armellina E, Dharmakumar R et al (2019) Cardiac MRI endpoints in myocardial infarction experimental and clinical trials: JACC Scientific Expert Panel. J Am Coll Cardiol 74:238–256
Nordlund D, Kanski M, Jablonowski Koul S, Erlinge Carlsson M, Engblom H, Aletras AH, Arheden H (2017) Experimental validation of contrast-enhanced SSFP cine CMR for quantification of myocardium at risk in acute myocardial infarction. J Cardiovasc Magn Reson 19:12
Niccoli G, Montone RA, Ibanez B, Thiele H, Crea F, Heusch G, Bulluck H, Hausenloy DJ, Berry C, Stiermaier T et al (2019) Optimized treatment of ST-elevation myocardial infarction. Circ Res 125:245–258
Hamirani YS, Wong A, Kramer CM, Salerno M (2014) Effect of microvascular obstruction and intramyocardial hemorrhage by CMR on LV remodeling and outcomes after myocardial infarction: a systematic review and meta-analysis. JACC Cardiovasc Imaging 7:940–952
Galea N, Dacquino GM, Ammendola RM, Coco S, Agati L, De Luca L, Carbone I, Fedele F, Catalano C, Francone M (2019) Microvascular obstruction extent predicts major adverse cardiovascular events in patients with acute myocardial infarction and preserved ejection fraction. Eur Radiol 29:2369–2377
DeWaha S, Patel MR, Granger CB, Ohman EM, Maehara A, Eitel I, Ben-Yehuda O, Jenkins P, Thiele H, Stone GW (2017) Relationship between microvascular obstruction and adverse events following primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: an individual patient data pooled analysis from seven randomized trials. Eur Heart J 38:3502–3510
Messroghli DR, Niendorf T, Schulz-Menger J, Dietz R, Friedrich MG (2003) T1 mapping in patients with acute myocardial infarction. J Cardiovasc Magn Reson 5:353–359. https://doi.org/10.1081/jcmr-120019418
Ici DO, Jeuthe S, Al-Wakeel N, Berger F, Kuehne T, Kozerke S, Messroghli DR (2014) T1 mapping in ischaemic heart disease. Eur Heart J Cardiovasc Imaging 15:597–602
Tessa C, Del Meglio J, Lilli A et al (2018) T1 and T2 mapping in the identification of acute myocardial injury in patients with NSTEMI. Radiol Med 123:926–934. https://doi.org/10.1007/s11547-018-0931-2
Carrick D, Haig C, Rauhalammi S, Ahmed N, Mordi I, McEntegart M, Petrie MC, Eteiba H, Hood S, Watkins S et al (2016) Prognostic significance of infarct core pathology revealed by quantitative non-contrast in comparison with contrast cardiac magnetic resonance imaging in reperfused ST-elevation myocardial infarction survivors. Eur Heart J 37:1044–1059
Nakamori S, Alakbarli J, Bellm S, Motiwala SR, Addae G, Manning WJ, Nezafat R (2017) Native T1 value in the remote myocardium is independently associated with left ventricular dysfunction in patients with prior myocardial infarction. J Magn Reson Imaging 46:1073–1081
Biesbroek PS, Amier RP, Teunissen PFA, Hofman MBM, Robbers L, van de Ven PM, Beek AM, van Rossum AC, van Royen N, Nijveldt R et al (2017) Changes in remote myocardial tissue after acute myocardial infarction and its relation to cardiac remodeling: a CMR T1 mapping study. PLoS ONE 12:e0180115
Chan W, Duffy SJ, White DA, Gao XM, Du XJ, Ellims AH, Dart AM, Taylor AJ (2012) Acute left ventricular remodeling following myocardial infarction: coupling of regional healing with remote extracellular matrix expansion. JACC Cardiovasc Imaging 5:884–893
Rochitte CE, Lima JAC, Bluemke DA, Reeder SB, McVeigh ER, Furuta T, Becker LC, Melin JA (1998) Magnitude and time course of microvascular obstruction and tissue injury after acute myocardial infarction. Circulation 10:1006–1101
Reffelmann T, Kloner RA (2006) The no-reflow phenomenon: a basic mechanism of myocardial ischemia and reperfusion. Basic Res Cardiol 101:359–372
Reinstadler SJ, Stiermaier T, Reindl M, Feistritzer HJ, Fuernau G, Eitel C, Desch S, Klug G, Thiele H, Metzler B (2019) Intramyocardial haemorrhage and prognosis after ST-elevation myocardial infarction. Eur Heart J Cardiovasc Imaging 20:138–146
Stiermaier T, Jobs A, deWaha S, Fuernau G, Poss J, Desch S, Thiele H, Eitel I (2017) Optimized prognosis assessment in ST-segment-elevation myocardial infarction using a cardiac magnetic resonance imaging risk score. Circ Cardiovasc Imaging 10:e006774
Pontone G, Guaricci AI, Andreini D, Ferro G, Guglielmo M et al (2017) Prognostic stratification of patients with ST-segment-elevation myocardial infarction (PROSPECT): a cardiac magnetic resonance study. Circ Cardiovasc Imaging 10(11):e006428
Schuster A, Backhaus SJ, Stiermaier T, Navarra JL, Uhlig J, Rommel KP, Koschalka A, Kowallick JT, Lotz J, Gutberlet M et al (2019) Left atrial function with MRI enables prediction of cardiovascular events after myocardial infarction: insights from the AIDA STEMI and TATORT NSTEMI trials. Radiology 293:292–302
Albaeni A, Chatila K, Beydoun HA, Beydoun MA, Morsy M, Khalife WI (2020) In-hospital left ventricular thrombus following ST-elevation myocardial infarction. Int J Cardiol 299:1–6
Jobs A, Eitel C, Poss J, Desch S, Thiele H, Eitel I (2015) Effect of pericardial effusion complicating ST-elevation myocardial infarction as predictor of extensive myocardial damageand prognosis. Am J Cardiol 116:1010–1016
Grothoff M, Elpert C, Hoffmann J, Zachrau J, Lehmkuhl L, de Waha S, Desch S, Eitel I, Mende M, Thiele H, Gutberlet M (2012) Right ventricular injury in st-elevation myocardial infarction: Risk stratification by visualization of wall motion, edema, and delayed-enhancement cardiac magnetic resonance. Circul Cardiovasc Imaging 5:60–68
Medina de Chazal H, Del Buono MG, Keyser-Marcus L, Ma L, Moeller FG, Berrocal D, Abbate A (2018) Stress cardiomyopathy diagnosis and treatment: JACC state-of-the-art review. J Am Coll Cardiol 72(16):1955–1971
Tornvall P, Gerbaud E, Behaghel A et al (2015) Myocarditis or “true” infarction by cardiac magnetic resonance in patients with a clinical diagnosis of myocardial infarction without obstructive coronary disease: a meta-analysis of individual patient data. Atherosclerosis 241(1):87–91
West AM, Kramer CM (2010) Cardiovascular magnetic resonance imaging of myocardial infarction, viability, and cardiomyopathies. Curr Probl Cardiol 35(4):176–220
Rajiah P, Desai MY, Kwon D, Flamm SD (2013) MR imaging of myocardial infarction. RadioGraphics 33:1383–1412
Yang Y, Li W, Zhu H, PanX HuY, Arnott C, Mai W, Cai X, Huang Y (2020) Prognosis of unrecognised myocardial infarction determined by electrocardiography or cardiac magnetic resonance imaging: systematic review and meta-analysis. BMJ. https://doi.org/10.1136/bmj.m1184
Zhang N, Yang G, Gao Z, Xu C, Zhang Y, Shi R, Keegan J, Xu L, Zhang H, Fan Z, Firmin D (2019) Deep learning for diagnosis of chronic myocardial infarction on nonenhanced cardiac Cine MRI. Radiology 291:606–617
Knuuti J, Wins W, Saraste A et al (2020) ESC Guidelines for the diagnosis and management of chronic coronary syndromes. The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J 41:407–477
Thom H, West NE, Hughes V et al (2014) Cost-effectiveness of initial cardiovascular MR, stress SPECT or stress echocardiography as a gate-keeper test, compared with upfront invasive coronary angiography in the investigation and management of patients with stable chest pain:midterm oucomes from the CECat randomised trial. BMJ Open. https://doi.org/10.1136/bmjopen-2013-003419
Camici PG, Crea F (2007) Coronary microvascular dysfunction. N Engl J Med 356:830–840
Gould KI, Lipscomb H (1974) Effects of coronary stenoses on coronary flow reserve and resistance. Am J Cardiol 34:48–55
Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E (2013) Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. JCVMR 22:17. https://doi.org/10.1186/s12968-020-00607-1
Marano R, Natale L, Chiribiri A, Pirro F et al (2015) Cardic MR perfusion imaging: where we are. Radiol Med 120:190–206
Shehata ML, Basha T, Hayeri D, Harttung D et al (2014) MR myocardial perfusion imaging: insights on techniques, analysis, interpretation and findings. Radiographics 34:1636–1657
Khoo JP, Grundy BJ, Steadman CD et al (2012) Stress cardiovascular MR in routine clinical practise: referral patterns, accuracy, tolerance, safety and incidental findings. Br J Radiol 85:851–857
Karamitsos TD, Jayanth R, Tammy A, Pegg A et al (2009) Tolerance and safety of adenosine stress perfusion cardiovascular magnetic resonance imaging in patients with severe coronary artery disease. Int J Cardiovasc Imaging 25:277–283. https://doi.org/10.1007/s10554-008-9392-3
Lee SD, Huang WC, Peng NJ, Hu C (2017) Dipyridamole-induced adverse effects in myocardial perfusion scans: dynamic evaluation. Int J Cardiol Heart Vasc. 14:14–19. https://doi.org/10.1016/j.ijcha.2016.11.002
Pellikka PA, Arruda-Olson A, Chaudhry FA et al (2019) Guidelines for performance, interpretation, and application of stress echocardiography in Ischemic Heart Disease: from the American Society of Echocardiography. J Am Soc Echocardiogr 33(1):1–41. https://doi.org/10.1016/j.echo.2019.07.001
Manisty C, Ripley DP, Herrey AS et al (2015) Splenic switch-off: a tool to assess stress adeguacy in adenonosine perfusion cardiac MR imaging. Radiology 276:732–740
Di Bella EVR, Parker DL, Sinusas AJ (2005) On the dark rim artifact in dynamic contrast-enhanced MRI myocardial perfusion studies. Magn Reason Med 54:1295–1299
Hamon M, Fau G, Nee G et al (2010) Meta-analysis of the diagnostic performance of stress cardiac magnetic resonance imaging for detection of coronary artery disease. J Cardiovasc Magn Reson 12:29
De Jong MC, Genders TSS, van Geuns et al (2012) Diagnostic performance of stress myocardiale perfusion imaging for coronary artery disease: a systematic review and meta-analisys. Eur Radiol 22:1881–1895
Jaarsma C, Leiner T, Bekkers SC et al (2012) Diagnostic performance of noninvasive myocardial perfusion imaging using single-photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease a meta-analysis. JACC 59:1719–1728
Schwitter J, Wacker CM, Wilke N et al (2012) Superior diagnostic performance of perfusion-cardiovascular magnetic resonance versus SPECT to detect coronary artery disease: The secondary endpoints of multicenter multivendor MR-IMPACT II (Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial). J Cardiovasc Magn Reason 14:61
Greenwood JP, Maredia N, Younger JF et al (2012) Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 379:453–460
Chung SY, Lee KY, Chun EJ et al (2010) Comparison of stress perfusione MRI and SPECT for detection of myocardial ischemia in patients with angiographically proven three-vessel coronary artery disease. AJR 195:356362
Montalescot G, Sechtem V, Achenbach S et al (2013) ESC guidelines on the management of stable coronary artery disease The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34:2949–3003
Nandalur KR, Dwamena BA, Choudhri AF, Nandalur MR, Carlos RC (2007) Diagnostic performance of stress cardiac magnetic resonance in the detection of coronary artery disease; a meta-analisys. J Am Coll Cardiol 50:1343–1353
Greenwood JP, Ripley DP, Berry C et al (2016) Effect of care guided by cardiovascular magnetic resonance, myocardial perfusion scintigraphy, or NICE guidelines on subsequent unnecessary angiography rates. The CE-MARC 2 randomized clinical trial. JAMA 316(10):1051–1060. https://doi.org/10.1001/jama.2016.12680
Nagel E, Greenwood JP, McCann GP, for the MR-INFORM investigators et al (2019) Magnetic resonance perfusion or fractional flow reserve in coronary disease. N Engl J Med 380:2418–2428. https://doi.org/10.1056/nejmoa1716734
Lipinski MJ, McVey CM, Berger JS, Kramer CM, Salerno M (2013) Prognostic value of stress cardiac magnetic resonance imaging in patients with known or suspected coronary artery disease: a systematic review and meta-analysis. J Am Coll Cardiol 62(9):826–838. https://doi.org/10.1016/j.jacc.2013.03.080
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buffa, V., Di Renzi, P. CMR in the diagnosis of ischemic heart disease. Radiol med 125, 1114–1123 (2020). https://doi.org/10.1007/s11547-020-01278-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01278-9