Abstract
Purpose
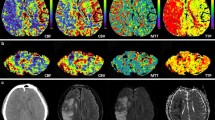
Crossed cerebellar (CC) diaschisis refers to a decrease in cerebellar perfusion in the presence of contralateral supratentorial lesions. Most of the previous studies have examined stroke patients. In contrast to strokes, seizure-related cerebral cortical lesions (SCCLs) usually show hyperperfusion, and therefore, cerebellar perfusion patterns are expected to be different from those of strokes. With arterial spin labelling (ASL), we evaluated the cerebellar perfusion status in patients with SCCLs.
Materials and methods
Using a search of the recent database over the last 31 months, 26 patients were enrolled in this study. The inclusion criteria were as follows: (1) a history of seizures, (2) MR examination taken within 24 h from the last seizure, (3) the presence of SCCLs on T2/FLAIR or DWI, (4) hyperperfusion in the corresponding areas of SCCLs on ASL, and (5) no structural abnormality in the cerebellum. The perfusion status in the contralateral cerebellum was evaluated and categorized as hyper-, iso- and hypoperfusion. The asymmetric index (AI) of cerebellar perfusion was calculated by ROI measurement of the signal intensity on ASL.
Results
The mean time between the last seizure and MR examinations was 5 h 30 min. CC hyperperfusion was observed in 17 patients (65.4%), hypoperfusion in 7 (26.9%) and isoperfusion in 2 (7.7%). Regarding the location of SCCLs, CC hyperperfusion was more frequent (71.4 vs. 58.3%), and the mean AI was higher (42.0 vs. 11.5) when the lesion involved the frontal lobe.
Conclusions
In patients with SCCLs, CC hyperperfusion occurred more often than hypo- and isoperfusion, especially when the lesions involved the frontal lobe.



Similar content being viewed by others
References
Ramnani N (2006) The primate cortico-cerebellar system: anatomy and function. Nat Rev Neurosci 7:511–522
Gold L, Lauritzen M (2002) Neuronal deactivation explains decreased cerebellar blood flow in response to focal cerebral ischemia or suppressed neocortical function. Proc Natl Acad Sci U S A 99:7699–7704
Graffeo CS, Snyder KA, Nasr DM et al (2016) Prognostic and mechanistic factors characterizing seizure-associated crossed cerebellar diaschisis. Neurocrit Care 24:258–263
Bailly P, Bazire A, Prat G et al (2017) Crossed cerebellar diaschisis in status epilepticus. Presse Med 46:117–118
Pantano P, Baron J, Samson Y et al (1986) Crossed cerebellar diaschisis: further studies. Brain 109:677–794
Cianfoni A, Caulo M, Cerase A et al (2013) Seizure-induced brain lesions: a wide spectrum of variably reversible MRI abnormalities. Eur J Radiol 82:1964–1972
Wolf RL, Detre JA (2007) Clinical neuroimaging using arterial spin-labeled perfusion magnetic resonance imaging. Neurotherapeutics 4:346–359
Detre JA, Rao H, Wang DJ et al (2012) Applications of arterial spin labeled MRI in the brain. J Magn Reson Imaging 35:1026–1037
Chen Y, Wang DJ, Detre JA (2011) Test–retest reliability of arterial spin labeling with common labeling strategies. J Magn Reson Imaging 33:940–949
Deibler AR, Pollock JM, Kraft RA et al (2008) Arterial spin-labeling in routine clinical practice, part 2: hypoperfusion patterns. AJNR Am J Neuroradiol 29:1235–1241
Matsuura K, Maeda M, Okamoto K et al (2015) Usefulness of arterial spin-labeling images in periictal state diagnosis of epilepsy. J Neurol Sci 359:424–429
Pizzini FB, Farace P, Manganotti P et al (2013) Cerebral perfusion alterations in epileptic patients during peri-ictal and post-ictal phase: PASL vs DSC-MRI. Magn Reson Imaging 31:1001–1005
Miyaji Y, Yokoyama M, Kawabata Y et al (2014) Arterial spin-labeling magnetic resonance imaging for diagnosis of late seizure after stroke. J Neurol Sci 339:87–90
Chen S, Guan M, Lian H et al (2014) Crossed cerebellar diaschisis detected by arterial spin-labeled perfusion magnetic resonance imaging in subacute ischemic stroke. J Stroke Cerebrovasc Dis 23:2378–2383
Kang KM, Sohn CH, Kim BS et al (2015) Correlation of asymmetry indices measured by arterial spin-labeling MR imaging and SPECT in patients with crossed cerebellar diaschisis. AJNR Am J Neuroradiol 36:1662–1668
Lin DD, Kleinman JT, Wityk RJ et al (2009) Crossed cerebellar diaschisis in acute stroke detected by dynamic susceptibility contrast MR perfusion imaging. AJNR Am J Neuroradiol 30:710–715
Kang KM, Sohn C, Choi SH et al (2017) Detection of crossed cerebellar diaschisis in hyperacute ischemic stroke using arterial spin-labeled MR imaging. PLoS ONE 12:e0173971
Varoquaux A, Rager O, Lovblad K et al (2013) Functional imaging of head and neck squamous cell carcinoma with diffusion-weighted MRI and FDG PET/CT: quantitative analysis of ADC and SUV. Eur J Nucl Med Mol Imaging 40:842–852
Oppo K, Leen E, Angerson WJ et al (1998) Doppler perfusion index: an interobserver and intraobserver reproducibility study. Radiology 208:453–457
Takasawa M, Watanabe M, Yamamoto S et al (2002) Prognostic value of subacute crossed cerebellar diaschisis: single-photon emission CT study in patients with middle cerebral artery territory infarct. AJNR Am J Neuroradiol 23:189–193
Shinohara Y, Kato A, Kuya K et al (2017) Perfusion MR imaging using a 3D pulsed continuous arterial spin-labeling method for acute cerebral infarction classified as branch atheromatous disease involving the lenticulostriate artery territory. AJNR Am J Neuroradiol 38:1550–1554
Won JH, Lee JD, Chung TS et al (1996) Increased contralateral cerebellar uptake of technetium-99 m-HMPAO on ictal brain SPECT. J Nucl Med 37:426–429
Marks DA, Katz A, Hoffer P et al (1992) Localization of extratemporal epileptic foci during ictal single photon emission computed tomography. Ann Neurol 31:250–255
Shin WC, Hong SB, Tae WS et al (2001) Ictal hyperperfusion of cerebellum and basal ganglia in temporal lobe epilepsy: SPECT subtraction with MRI coregistration. J Nucl Med 42:853–858
Poretti A, Boltshauser E (2012) Crossed cerebro-cerebellar diaschisis. Neuropediatrics 43:53–54
Long B, Koyfman A (2017) Clinical mimics: an emergency medicine-focused review of stroke mimics. J Emerg Med 52:176–183
Deibler AR, Pollock JM, Kraft RA et al (2008) Arterial spin-labeling in routine clinical practice, part 3: hyperperfusion patterns. AJNR Am J Neuroradiol 29:1428–1435
Acknowledgements
The authors would like to thank ‘Wiley Editing Services’ for the English: http://authorservices.wiley.com/bauthor/english_language.asp.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of our institutional review board (IRB) after its approval and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Our IRB determined that patient approval and informed consent were not required because of retrospectively reviewing images and records.
Rights and permissions
About this article
Cite this article
Won, J., Choi, D.S., Hong, S.J. et al. Crossed cerebellar hyperperfusion in patients with seizure-related cerebral cortical lesions: an evaluation with arterial spin labelling perfusion MR imaging. Radiol med 123, 843–850 (2018). https://doi.org/10.1007/s11547-018-0921-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0921-4