Abstract
Purpose
This article illustrates the feasibility of MR lymphangiography (MRL) for imaging lymphatic vessels in patients with lymphedema, its accuracy in distinguishing lymphatic vessels from veins, and its utility for planning Lymphaticovenous anastomosis (LVA) treatment.
Materials and methods
We prospectively enrolled 30 patients (24 women, range 18–70, 17 cases of lower limb lymphedema, 6 cases of primary lymphedema). All the patients underwent MRL, using a 1.5T MR unit (Signa Twin Speed Hdxt; GE), after the subcutaneous injection of gadobenate dimeglumine (Gd-BOPTA) with a little dose of lidocaine into the interdigital webs of the dorsal foot or hand. Lymphatic vessels identified for the LVA at MRL were histologically confirmed after surgery. Enhancement of lymphatic vessels and veins at different times after injection of contrast medium and their diameters were measured.
Results
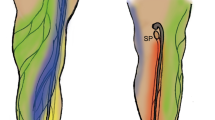
A total of 79 lymphatic vessels were clearly identified in 29 patients at MRL; their morphology was tortuous in 22 patients and rectilinear in 7, whereas, the adjacent veins were straight with focal bulging only at the level of venous valve; the enhancement kinetic of the two different structures were different (p < 0.05) but the mean diameter of affected lymphatic vessels was similar to the adjacent veins (p > 0.05). Thirty-four out of 38 specimens of presumed lymphatic vessels at MRL, collected during surgery, resulted positive at the immunoistochemical marker d2–40, with a significant association (Chi-square = 40.421, DF = 1, p < 0.05, contingency coefficent 0.644). One patient had an early complication 1 month after treatment.
Conclusions
MRL is easy and safe to use and combines extensive information on the anatomy and functionality of lymphatic vessels and veins in a single process; therefore, it could be useful in LVA treatment planning and evaluating possible super-microsurgical treatment complications in patients with lymphedema.




Similar content being viewed by others
References
Cho S, Atwood JE (2002) Peripheral edema. Am J Med 113(7):580–586
Mortimer P, Bates D, Brassington H, Stanton A, Strachan D, Levick J (1996) The prevalence of arm oedema following treatment for breast cancer. Q J Med 89:377–380
Szuba A, Rockson SG (1998) Lymphedema: classification, diagnosis and therapy. Vasc Med 3:145–156
Szuba A, Rockson SG (1997) Lymphedema: anatomy, physiology and pathogenesis. Vasc Med. 2:321–326
Mortimer PS (1998) The pathophysiology of lymphedema. Cancer 83:2798–2802
Passik SD, McDonald MV (1998) Psychosocial aspects of upper extremity lymphedema in women treated for breast carcinoma. Cancer 83:2817–2820 (Review)
Olszewski WL (2013) Lymphovenous microsurgical shunts in treatment of lymphedema of lower limbs: a 45-year experience of one surgeon/one center. Eur J Vasc Endovasc Surg 45(3):282–290
Lu Q, Bui D, Liu NF, Xu JR, Zhao XH, Zhang XF (2012) Magnetic resonance lymphography at 3T: a promising noninvasive approach to characterise inguinal lymphatic vessel leakage. Eur J Vasc Endovasc Surg 43(1):106–111
Gennaro P, Borghini A, Chisci G, Mazzei F, Weber E, Tedone Clemente E, Guerrini S, Gentili F, Gabriele G, Ungari C, Mazzei MA (2017) Could MRI visualize the invisible? An Italian single center study comparing magnetic resonance lymphography (MRL), super-microsurgery and histology in the identification of lymphatic vessels. Eur Rev Med Pharmacol Sci 21(4):687–694
White RD, Weir-McCall JR, Budak MJ, Waugh SA, Munnoch DA, Sudarshan TA (2014) Contrast-enhanced magnetic resonance lymphography in the assessment of lower limb lymphoedema. Clin Radiol 69:e435–e444
Mazzei FG, Gentili F, Guerrini S, Cioffi Squitieri N, Guerrieri D, Gennaro P, Scialpi M, Volterrani L, Mazzei MA (2017) MR lymphangiography: a practical guide to perform it and a brief review of the literature from a technical point of view. Biomed Res Int 2017:2598358
Mihara M, Hara H, Furniss D, Narushima M, Iida T, Kikuchi K, Ohtsu H, Gennaro P, Gabriele G, Murai N (2014) Lymphaticovenular anastomosis to prevent cellulitis associated with lymphoedema. Br J Surg 101:1391–1396
Koshima I, Narushima M, Yamamoto Y, Mihara M, Iida T (2012) Recent advancement on surgical treatments for lymphedema. Ann Vasc Dis 5(4):409–415
Lu Q, Xu J, Liu N (2010) Chronic lower extremity lymphedema: a comparative study of high-resolution interstitial MR lymphangiography and heavily T2-weighted MRI. EurJ Radiol 73:365–373
Jackson RJA (1966) Complications of lymphography. BMJ 1(5497):1203–1205
Lohrmann C, Foeldi E, Langer M (2006) Indirect magnetic resonance lymphangiography in patients with lymphedema preliminary results in humans. Eur J Radiol 59(3):401–406
Kirchin MA, Runge VM (2003) Contrast agents for magnetic resonance imaging: safety update. Top Magn Reson Imaging 14(5):426–435
Runge VM, Dickey KM, Williams NM, Peng X (2002) Local tissue toxicity in response to extravascular extravasation of magnetic resonance contrast media. Invest Radiol 37(7):393–398
Cohan RH, Leder RA, Herzberg AJ, Hedlund LW, Wheeler CT, Beam CA, Nadel SN, Dunnick NR (1991) Extravascular toxicity of two magnetic resonance contrast agents. Preliminary experience in the rat. Invest Radiol 26(3):224–226
Notohamiprodjo M, Baumeister RG, Jakobs TF, Bauner KU, Boehm HF, Horng A, Reiser MF, Glaser C, Herrmann KA (2009) MR-lymphangiography at 3.0T—a feasibility study. Eur Radiol 19(11):2771–2778
Lohrmann C, Foeldi E, Speck O, Langer M (2006) High-resolution MR lymphangiography in patients with primary and secondary lymphedema. AJR Am J Roentgenol 187(2):556–561
Gennaro P, Chisci G, Mazzei F, Gabriele G (2016) Magnetic resonance lymphangiography: how to prove it? J Magn Reson Imaging. doi:10.1002/jmri.25147
Lohrmann C, Foeldi E, Bartholomä JP, Langer M (2007) Interstitial MR lymphangiography—a diagnostic imaging method for the evaluation of patients with clinically advanced stages of lymphedema. Acta Trop 104(1):8–15
Cavagna FM, Maggioni F, Castelli PM, Daprà M, Imperatori LG, Lorusso V, Jenkins BG (1997) Gadolinium chelates with weak binding to serum proteins. A new class of high-efficiency, general purpose contrast agents for magnetic resonance imaging. Invest Radiol 32(12):780–796
Arrivé L, Derhy S, El Mouhadi S, Monnier-Cholley L, Menu Y, Becker C (2016) Noncontrast magnetic resonance lymphography. J Reconstr Microsurg 32(1):80–86
Lu Q, Delproposto Z, Hu A, Tran C, Liu N, Li Y, Xu J, Bui D, Hu J (2012) MR lymphography of lymphatic vessels in lower extremity with gynecologic oncology-related lymphedema. PLoS One 7(11):e50319
Jeon JY, Lee SH, Shin MJ, Chung HW, Lee MH (2016) Three-dimensional isotropic fast spin-echo MR lymphangiography of T1-weighted and intermediate-weighted pulse sequences in patients with lymphoedema. Clin Radiol 71(1):e56–e63
Mitsumori LM, McDonald ES, Wilson GJ, Neligan PC, Minoshima S, Maki JH (2015) MR lymphangiography: how I do it. J Magn Reson Imaging 42:1465–1477
Notohamiprodjo M, Weiss M, Baumeister RG, Sommer WH, Helck A, Crispin A, Reiser MF, Herrmann KA (2012) MR lymphangiography at 3.0T: correlation with lymphoscintigraphy. Radiology 264(1):78–87
Nagase T, Gonda K, Inoue K, Higashino T, Fukuda N, Gorai K, Mihara M, Nakanishi M, Koshima I (2005) Treatment of lymphedema with lymphaticovenular anastomoses. Int J Clin Oncol 10(5):304–310
Gilbert A, O’Brien BM, Vorrath JW et al (1976) Lymphaticovenous anastomosis by microvascular technique. Br J Plast Surg 29(4):355–360
Maegawa J, Yabuki Y, Tomoeda H, Hosono M, Yasumura K (2012) Outcomes of lymphaticovenous side-to-end anastomosis in peripheral lymphedema. J Vasc Surg 55(3):753–760
Author information
Authors and Affiliations
Contributions
Author contributions
Mazzei FG, Gennaro P, Weber E, Botta G., Mazzei MA, Volterrani L: conception, design and critical revision of this article; Gentili F, Guerrieri D, Nigri A, Weber E, Fausto A: analysis and interpretation of data and drafting of the article; all the authors: final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in this study involving human participants were undertaken in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Patients were fully informed of the procedure to obtain their complete collaboration and informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Mazzei, M.A., Gentili, F., Mazzei, F.G. et al. High-resolution MR lymphangiography for planning lymphaticovenous anastomosis treatment: a single-centre experience. Radiol med 122, 918–927 (2017). https://doi.org/10.1007/s11547-017-0795-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-017-0795-x