Abstract
Purpose
To understand the meaning of diffuse excessive high signal intensity (DEHSI) of white matter (WM), a frequently observed finding on MR in VLBW infants at a corrected term age.
Methods
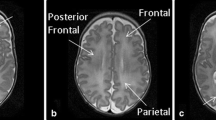
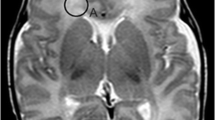
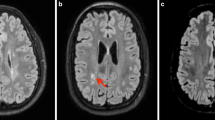
This is a retrospective study. Qualitative visual assessment of cerebral WM signal intensity on T2WI was performed by two readers on 78 VLBW infants, scanned on a 1.5 T-MRI at term equivalent age. ADC values were then measured in six regions of interest: four in frontal and parietal periventricular and two in parietal subcortical WM. Mean ADC values were then compared with qualitative visual assessment and with mean ADC values obtained ten term healthy babies. Both periventricular and subcortical mean ADC values were correlated with the neurological follow-up, evaluated with the Griffith’s mental developmental scale at 36 months.
Results
There was no agreement between the visual qualitative assessment of white matter DEHSI and corresponding ADC values (P values = 0.42 for periventricular WM; P values = 0.18 for subcortical WM). Mean ADC values were higher in preterms than in term babies (P values <0.001). No significant correlation was found between ADC values and the developmental quotient at 36 months (P values >0.05).
Conclusions
DEHSI in VLBW infants is a MR finding poorly defined with conventional T2 MRI. The presence of T2 hyperintensities weakly correlates with ADC, and ADC values are not associated with the neurological long-term outcome at 3 years, demonstrating that DEHSI should not be considered as a WM disease.



Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffuse coefficient
- DEHSI:
-
Diffuse excessive high signal intensity
- DQ:
-
Developmental quotient
- DTI:
-
Diffusion tensor imaging
- DWI:
-
Diffuse-weighted imaging
- GMDS:
-
Griffith’s mental developmental scale
- MRI:
-
Magnetic resonance imaging
- NICU:
-
Neonatal intensive care unit
- SGA:
-
Small for gestational age
- TTTS:
-
Twin-to-twin transfusion syndrome
- VLBW:
-
Very low birth weight
- WM:
-
White matter
References
Cheong JL, Doyle LW (2012) Increasing rates of prematurity and epidemiology of late preterm birth. J Paediatr Child Health 48(9):784–788
Hamrick SE, Miller SP, Leonard C et al (2004) Trends in severe brain injury and neurodevelopmental outcome in premature newborn infants: the role of cystic periventricular leukomalacia. DMJ Pediatr 145(5):593–599
Dyet LE, Kennea N, Counsell SJ et al (2006) Natural history of brain lesions in extremely preterm infants studied with serial magnetic resonance imaging from birth and neurodevelopmental assessment. Pediatrics 118(2):536–548
Rutherford MA, Supramaniam V, Ederies A et al (2010) Magnetic resonance imaging of white matter diseases of prematurity. Neuroradiology 52(6):505–521
Volpe JJ (2009) Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol 8(1):110–124
Battin MR, Maalouf EF, Counsell SJ et al (1998) Magnetic resonance imaging of the brain in very preterm infants: visualization of the germinal matrix, early myelination, and cortical folding. Pediatrics 101(6):957–962
Deng W (2010) Neurobiology of injury to the developing brain. Nat Rev Neurol 6(6):328–336
Maalouf EF, Duggan PJ, Rutherford MA et al (1999) Magnetic resonance imaging of the brain in a cohort of extremely preterm infants. J Pediatr 135(3):351–357
Hagmann CF, De Vita E, Bainbridge A, Gunny R et al (2009) T2 at MR imaging is an objective quantitative measure of cerebral white matter signal intensity abnormality in preterm infants at term-equivalent age. Radiology 252(1):209–217
Counsell SJ, Shen Y, Boardman JP et al (2006) Axial and radial diffusivity in preterm infants who have diffuse white matter changes on magnetic resonance imaging at term-equivalent age. Pediatrics 117(2):376–386
Hart AR, Whitby EH, Clark SJ et al (2010) Diffusion-weightedimaging of cerebral white matter and the cerebellum following preterm birth. Dev Med Child Neurol 52(7):652–659
Jeon TY, Kim JH, Yoo SY et al (2012) Neurodevelopmental outcomes in preterm infants: comparison of infants with and without diffuse excessive high signal intensity on mr images at near-term-equivalent age. Radiology 263(2):518–526
Krishnan ML, Dyet LE, Boardman JP et al (2007) Relationship between white matter apparent diffusion coefficients in preterm infants at term-equivalent age and developmental outcome at 2 years. Pediatrics 120(3):e604–e609
Counsell SJ, Allsop JM, Harrison MC, Larkman DJ et al (2003) Diffusion-weighted imaging of the brain in preterm infants with focal and diffuse white matter abnormality. Pediatrics 112(1 Pt 1):1–7
Hüppi PS, Murphy B, Maier SE et al (2001) Microstructural brain development after perinatal cerebral white matter injury assessed by diffusion tensor magnetic resonance imaging. Pediatrics 107(3):455–460
De Bruïne FT, Van denBerg-Huysmans AA, Leijser LM et al (2011) Clinical implications of MR imaging findings in the white matter in very preterm infants: a 2-year follow-up study. Radiology 261(3):899–906
Hart AR, Smith MF, Rigby AS et al (2010) Appearances of diffuse excessive high signal intensity (DEHSI) on MR imaging following preterm birth. Pediatr Radiol 40(8):1390–1396
Boardman James P, Serena J et al (2006) Abnormal deep grey matter development following preterm birthdetected using deformation-based morphometryi. NeuroImage 32:70–78
Armitage P, Berry G, Matthews JNS (2002) Statistical methods in medical research, 4th edn. Blackwell Science, Oxford
Fleiss JL (1981) Statistical methods for rates and proportions, 2nd edn. Wiley, New York, pp 38–46
Kidokoro H, Anderson PJ, Doyle LW et al (2011) High signal intensity on T2-weighted MR imaging at term-equivalent age in preterm infants does not predict 2-year neuro developmental outcomes. AJNR Am J Neuroradiol 32(11):2005–2010
Hart A, Whitby E, Wilkinson S et al (2011) Neuro-developmental outcome at 18 months in premature infants with diffuse excessive high signal intensity on MR imaging of the brain. Pediatr Radiol 41(10):1284–1292
Miller SP, Ferriero DM, Leonard C et al (2005) Early brain injury in premature newborns detected with magnetic resonance imaging is associated with adverse early neurodevelopmental outcome. JPediatr 147(5):609–616
Schneider JF, Confort-Gouny S, Le Fur Y, Viout P et al (2007) Diffusion-weighted imaging in normal fetal brain maturation. Eur Radiol 17(9):2422–2429
Ono J, Kodaka R, Imai K et al (1993) Evaluation of myelination by means of the T2 value on magnetic resonance imaging. Brain Dev 15(6):433–438
Grimmer I, Metze BC, Walch E et al (2010) Predicting neurodevelopmental impairment in preterm infants by standardized neurological assessments at 6 and 12 months corrected age. Acta Paediatr 99(4):526–530
Wisnowski JL, Schmithorst VJ, Rosser T, Paquette L, Nelson MD et al (2014) Magnetic resonance spectroscopy markers of axons and astrogliosis in relation to specific features of white matter injury in preterm infants. Neuroradiology 56(9):771–779
Conflict of interest
The authors whose names are listed immediately below certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author names: CMC, MD; SFC, MD; LB, MD; SA, MD; MF, MD; LB, MD; OP, MD; DC, MD; FM, MD; FT, MD.
Ethical standards and patient consent
We declare that this manuscript does not contain clinical studies or patient data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calloni, S.F., Cinnante, C.M., Bassi, L. et al. Neurodevelopmental outcome at 36 months in very low birth weight premature infants with MR diffuse excessive high signal intensity (DEHSI) of cerebral white matter. Radiol med 120, 1056–1063 (2015). https://doi.org/10.1007/s11547-015-0540-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-015-0540-2