Abstract
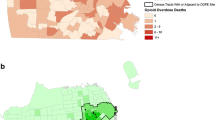
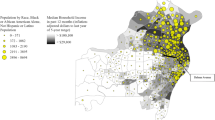
Improving access to naloxone for laypersons is a cornerstone of the US strategy to reduce opioid overdose deaths. This study evaluated change in distance to opioid overdose prevention programs (OOPPs) providing walk-in naloxone across two time points. We also explored individual and neighborhood disparities in distance to OOPPs, associations between 2020 OOPP locations and 2018 overdoses, and associations between OOPPs and neighborhood fatal overdose rates. Using fatal opioid overdose locations in 2018 (n = 1167) and 2020 (n = 2045) in New York City, we mapped OOPP locations and fatal overdose locations to visualize areas of unmet naloxone need. We used logistic regression to assess individual (age, sex, race/ethnicity) and neighborhood correlates of odds of an overdose occurring within walking distance (≤ 0.5 miles or 0.8 km) of an OOPP and negative binomial regression to assess the relationship between census tract-level OOPP counts and overdose rates. Distance to OOPPs significantly improved over time, with average distance decreasing by 1.7 miles (2.7 km) (p < 0.001). OOPPs were more likely to be located in neighborhoods with higher poverty in both years and in closer proximity to Latinos in 2020—suggesting improved access for Latinos and in higher poverty neighborhoods. OOPP locations in 2020 were significantly positively associated with overdose locations in 2018. OOPPs were not well-situated in neighborhoods with elevated overdose rates in 2018 but were better situated in 2020, controlling for other neighborhood variables. Community lay naloxone access through OOPPs improved over time and could have promising effects for improved overdose rates in the future.

Similar content being viewed by others
Data Availability
Fatal overdose data are proprietary and available from New York City Office of the Chief Medical Examiner at their discretion.
References
Centers for Disease Control and Prevention. U.S. Overdose deaths in 2021 increased half as much as in 2020 - but are still up 15%. 2022. Available from: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm. Accessed 21 Oct 2022.
Rubin R. Surgeon general urges expanded availability of naloxone. JAMA. 2018;319:2068–2068.
Owczarzak J, Weicker N, Urquhart G, Morris M, Park JN, Sherman SG. “We know the streets:” race, place, and the politics of harm reduction. Health Place. 2020;64:102376.
Weiner J, Murphy SM, Behrends C. Expanding access to naloxone: a review of distribution strategies. 2019. Available from: https://ldi.upenn.edu/our-work/research-updates/expanding-access-to-naloxone-a-review-of-distribution-strategies/. Accessed 2 Aug 2021.
Naumann RB, Durrance CP, Ranapurwala SI, Austin AE, Proescholdbell S, Childs R, et al. Impact of a community-based naloxone distribution program on opioid overdose death rates. Drug Alcohol Depend. 2019;204:107536.
Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174.
Langham S, Wright A, Kenworthy J, Grieve R, Dunlop WCN. Cost-effectiveness of take-home naloxone for the prevention of overdose fatalities among heroin users in the United Kingdom. Value Health. 2018;21:407–15.
Townsend T, Blostein F, Doan T, Madson-Olson S, Galecki P, Hutton DW. Cost-effectiveness analysis of alternative naloxone distribution strategies: first responder and lay distribution in the United States. Int J Drug Policy. 2020;75:102536.
Hayes BT, Favaro J, Davis CS, Gonsalves GS, Beletsky L, Vlahov D, et al. Harm reduction, by mail: the next step in promoting the health of people who use drugs. J Urban Health. 2021;98:532–7.
Byregowda H, Tomko C, Schneider KE, Russell E, Johnson RM, Susukida R, et al. Disruptions to naloxone training among lay and occupational responders in Maryland during the emergence of COVID-19: early impacts, recovery, and lessons learned. Drug Alcohol Depend Rep. 2023;8:100173.
Behrends CN, Gutkind S, Winkelstein E, Wright M, Dolatshahi J, Welch A, et al. Costs of opioid overdose education and naloxone distribution in New York City. Subst Abus. 2022;43:692–8.
Wheeler E, Davidson PJ, Jones TS, Stephen T, Public J, Consulting H, et al. Community-based opioid overdose prevention programs providing naloxone–United States, 2010. Morb Mortal Wkly Rep. 2012;61:101–5.
Abouk R, Pacula RL, Powell D. Association between state laws facilitating pharmacy distribution of naloxone and risk of fatal overdose. JAMA Intern Med. 2019;179:805–11.
Abbas B, Marotta PL, Goddard-Eckrich D, Huang D, Schnaidt J, El-Bassel N, et al. Socio-ecological and pharmacy-level factors associated with naloxone stocking at standing-order naloxone pharmacies in New York City. Drug Alcohol Depend. 2021;218:108388.
Graves RL, Andreyeva E, Perrone J, Shofer F, Merchant RM, Meisel ZF. Naloxone availability and pharmacy staff knowledge of standing order for naloxone in Pennsylvania pharmacies. J Addict Med. 2019;13:272–8.
Guadamuz JS, Alexander GC, Chaudhri T, Trotzky-Sirr R, Qato DM. Availability and cost of naloxone nasal spray at pharmacies in Philadelphia, Pennsylvania, 2017. JAMA Netw Open. 2019;2:e195388.
Cid A, Daskalakis G, Grindrod K, Beazely MA. What is known about community pharmacy-based take-home naloxone programs and program interventions? Scoping Rev Pharm. 2021;9:30.
Orgera K, Tolbert J. Key facts about uninsured adults with opioid use disorder. 2019. Available from: https://www.kff.org/uninsured/issue-brief/key-facts-about-uninsured-adults-with-opioid-use-disorder/. Accessed 3 May 2023.
Peet ED, Powell D, Pacula RL. Trends in out-of-pocket costs for naloxone by drug brand and payer in the US, 2010–2018. JAMA Health Forum. 2022;3:E222663.
Hoffman J. Over-the-counter narcan could save more lives. But price and stigma are obstacles. The New York Times. 2023. Available from: https://www.nytimes.com/2023/03/28/health/narcan-otc-price.html. Accessed 1 Sept 2023.
Correal A. Overdose antidote is supposed to be easy to get. It’s not. New York Times. 2018. Available from: https://www.nytimes.com/2018/04/12/nyregion/overdose-antidote-naloxone-investigation-hard-to-buy.html. Accessed 30 Jul 2021.
Treloar C, Rance J, Yates K, Mao L. Trust and people who inject drugs: the perspectives of clients and staff of Needle Syringe Programs. Int J Drug Policy. 2016;27:138–45.
Donovan E, Case P, Bratberg JP, Baird J, Burstein D, Walley AY, et al. Beliefs associated with pharmacy-based naloxone: a qualitative study of pharmacy-based naloxone purchasers and people at risk for opioid overdose. J Urban Health. 2019;96:367–78.
Trinidad JP, Warner M, Bastian BA, Minino AM, Hedegaard H. Using literal text from the death certificate to enhance mortality statistics: characterizing drug involvement in deaths. National Vital Statistics Reports. Hyattsville, MD; 2016. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27996933. Accessed 11 May 2019.
New York City Department of Health and Mental Hygiene. Naloxone/Narcan at New York City Opioid Overdose Programs. 2018. Available from: https://www1.nyc.gov/assets/doh/downloads/pdf/basas/naloxone-community-based%20programs.pdf. Accessed 21 Jul 2021.
New York City Department of Health and Mental Hygiene. Naloxone (Narcan) at New York City Opioid Overdose Prevention Programs. 2021. Available from: https://www1.nyc.gov/assets/doh/downloads/pdf/basas/naloxone-list-of-prevention-programs.pdf. Accessed 21 Jul 2021.
Blanchard SK. NYC revamps pharmacies’ role in preventing overdose deaths. Filter. 2021. Available from: https://filtermag.org/nyc-pharmacy-overdose/. Accessed 21 Aug 2021.
Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42:258–76.
Krieger N, Waterman P, Spasojevic J, Li W, Maduro G, van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. Am J Public Health. 2016;106:256–63.
Massey D. The prodigal paradigm returns: ecology comes back to sociology. In: Booth A, Crouter A, editors. Does It Take a Village? Community Effects on Children, Adolescents, and Families. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. p. 41–8.
Millward H, Spinney J, Scott D. Active-transport walking behavior: destinations, durations, distances. J Transp Geogr. 2013;28:101–10.
Yang Y, Diez-Roux AV. Walking distance by trip purpose and population subgroups. Am J Prev Med. 2012;43:11–9.
Waller LA, Gotway CA. Applied spatial statistics for public health data. Hoboken, NJ: Wiley; 2004.
Coulton CJ, Korbin J, Chan T, Su M. Mapping residents’ perceptions of neighborhood boundaries: a methodological note. Am J Community Psychol. 2001;29:371–83.
Khatri UG, Perrone J. Opioid Use Disorder and COVID-19: crashing of the Crises. J Addict Med. 2020;14:e6–7.
Karahalios A, Baglietto L, Carlin JB, English DR, Simpson JA. A review of the reporting and handling of missing data in cohort studies with repeated assessment of exposure measures. BMC Med Res Methodol. 2012;12:96.
Reed M, Wagner KD, Tran NK, Brady KA, Shinefeld J, Roth A. Prevalence and correlates of carrying naloxone among a community-based sample of opioid-using people who inject drugs. Int J Drug Policy. 2019;73:32–5.
Nolen S, Zang X, Chatterjee A, Behrends CN, Green TC, Linas BP, et al. Evaluating equity in community-based naloxone access among racial/ethnic groups in Massachusetts. Drug Alcohol Depend. 2022;241:109668.
Chan W. New York’s Narcan vending machine is stopping overdoses. New York Magazine. 2023. Available from: https://www.curbed.com/2023/07/vending-machine-narcan-brownsville-opioid-overdose.html. Accessed 10 Oct 2023.
Hoffman J, Weiland N. Narcan is headed to stores: what you need to know. New York Times. 2023. Available from: https://www.nytimes.com/2023/08/30/health/narcan-drug-stores.html1/2https://www.nytimes.com/2023/08/30/health/narcan-drug-stores.html. Accessed 10 Oct 2023.
Spadaro A, Agarwal AK, Sangha HK, Perrone J, Delgado MK, Lowenstein M. Motivation to Carry Naloxone: a Qualitative Analysis of Emergency Department Patients. Am J Health Promot. 2023;37:200–9.
Bessen S, Metcalf SA, Saunders EC, Moore SK, Meier A, McLeman B, et al. Barriers to naloxone use and acceptance among opioid users, first responders, and emergency department providers in New Hampshire, USA. Int J Drug Policy. 2019;74:144–51.
Yi G, Dayton L, Uzzi M, Browne K, Konstantopoulos A, Latkin C. Spatial and neighborhood-level correlates of lay naloxone reversal events and service availability. Int J Drug Policy. 2022;106:103739.
Acknowledgements
This work was supported by the National Institute on Drug Abuse (grant number K01DA049900). The authors thank New York City Office of the Chief Medical Examiner for providing fatal overdose data.
Author information
Authors and Affiliations
Contributions
EDN: conceptualization, methodology, supervision, formal analysis, writing—original and draft. HS: formal analysis, writing—original and draft. ZFM: writing—review and editing. SSM: methodology, writing—review an editing.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nesoff, E.D., Meisel, Z.F., Saeed, H. et al. Neighborhood and Individual Disparities in Community-Based Naloxone Access for Opioid Overdose Prevention. J Urban Health 101, 64–74 (2024). https://doi.org/10.1007/s11524-023-00821-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-023-00821-z