Abstract
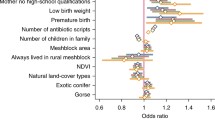
Vegetation may influence asthma exacerbation through effects on aeroallergens, localized climates, air pollution, or children’s behaviors and stress levels. We investigated the association between residential vegetation and asthma exacerbation by conducting a matched case–control study based on electronic health records of asthma patients, from the Children’s Hospital of Philadelphia (CHOP). Our study included 17,639 exacerbation case events and 34,681 controls selected from non-exacerbation clinical visits for asthma, matched to cases by age, sex, race/ethnicity, public payment source, and residential proximity to the CHOP main campus ED and hospital. Overall greenness, tree canopy, grass/shrub cover, and impervious surface were assessed near children’s homes (250 m) using satellite imagery and high-resolution landcover data. We used generalized estimating equations to estimate odds ratios (OR) and 95% confidence intervals (CI) for associations between each vegetation/landcover measure and asthma exacerbation, with adjustment for seasonal and sociodemographic factors—for all cases, and for cases defined by diagnosis setting and exacerbation frequency. Lower odds of asthma exacerbation were observed in association with greater levels of tree canopy near the home, but only for children who experienced multiple exacerbations in a year (OR = 0.94 per 10.2% greater tree canopy coverage, 95% CI = 0.90–0.99). Our findings suggest possible protection for asthma patients from tree canopy, but differing results by case frequency suggest that potential benefits may be specific to certain subpopulations of asthmatic children.





Similar content being viewed by others
References
Bryant-Stephens T. Asthma disparities in urban environments. J Allergy Clinical Immunol. 2009;123(6):1199–206.
Ferrante G, La Grutta S. The burden of pediatric asthma (editorial). Front Pediatr. 2018;6:186.
Nunes C, Pereira AM, Morais-Almeida M. Asthma costs and social impact. Asthma Res Pract. 2017;3:1.
Perry R, Braileanu G, Palmer T, Stevens P. The economic burden of pediatric asthma in the United States: literature review of current evidence. Pharmacoeconom. 2019;37(2):155–67.
Keet CA, Matsui EC, McCormack MC, Peng RD. Urban residence, neighborhood poverty, race/ethnicity, and asthma morbidity among children on Medicaid. J Allergy Clin Immunol. 2017;140(3):822–7.
Zheng XY, Ding H, Jiang LN, et al. 2015 Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS One;10(9):e0138146.
Markevych I, Schoierer J, Hartig T, et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res. 2017;158:301–17.
De Roos AJ, Kenyon CC, Zhao Y, et al. 2020 Ambient daily pollen levels in association with asthma exacerbation among children in Philadelphia, Pennsylvania. Environ Int.;145:106138.
Lovasi GS, Quinn JW, Neckerman KM, Perzanowski MS, Rundle A. Children living in areas with more street trees have lower prevalence of asthma. J Epidemiol Community Health. 2008;62(7):647–9.
Chen E, Miller GE, Shalowitz MU, et al. 2017 Difficult family relationships, residential greenspace, and childhood asthma. Pediatrics.;139(4):e20163056.
Tischer C, Gascon M, Fernández-Somoano A, et al. Urban green and grey space in relation to respiratory health in children. Eur Respir J. 2017;49(6):1502112.
Alcock I, White M, Cherrie M, et al. Land cover and air pollution are associated with asthma hospitalisations: a cross-sectional study. Environ Int. 2017;109:29–41.
DePriest K, Butz A, Curriero FC, Perrin N, Gross D. Associations among neighborhood greenspace, neighborhood violence, and children’s asthma control in an urban city. Ann Allergy Asthma Immunol. 2019;123(6):608–10.
Dzhambov AM, Lercher P, Rüdisser J, Browning MHEM, Markevych I. 2021 Allergic symptoms in association with naturalness, greenness, and greyness: a cross-sectional study in schoolchildren in the Alps. Environ Res.;198:110456.
Parmes E, Pesce G, Sabel CE, et al. 2020 Influence of residential land cover on childhood allergic and respiratory symptoms and diseases: evidence from 9 European cohorts. Environ Res.;183:108953.
Kim D, Ahn Y. The contribution of neighborhood tree and greenspace to asthma emergency room visits: an application of advanced spatial data in Los Angeles County. Int J Environ Res Public Health. 2021;18(7):3487.
Pennsylvania Department of Health. Pennsylvania Asthma Burden Report (2012). http://www.paasthma.org/images/docs/2012_asthma_burden_report.pdf. Accessed March 14, 2021.
Asthma and Allergy Foundation of America (AAFA). Asthma Capitals 2019: the most challenging places to live with asthma. https://www.aafa.org/asthma-capitals/. Accessed March 14, 2021.
Delaware Valley Regional Planning Commission (DVRPC). Health Data Snapshot. https://www.dvrpc.org/health/PASnapshot/. Accessed March 14, 2021.
Nowak DJ, Bodine AR, Hoehn R, et al. The urban forests of Philadelphia. Resource Bulletin NRS-106. Newtown Square, PA: US Department of Agriculture, Forest Service, Northern Research Station. 2016;106:1–80.
Fuhlbrigge A, Peden D, Apter AJ, et al. Asthma outcomes: exacerbations. J Allergy Clin Immunol. 2012;129(3 Suppl):S34-48.
Kenyon CC, Maltenfort MG, Hubbard RA, et al. Variability in diagnosed asthma in young children in a large pediatric primary care network. Acad Pediatr. 2020;20(7):958–66.
Mudd AE, Michael YL, Diez-Roux AV, et al. Primary care accessibility effects on health care utilization among urban children. Acad Pediatr. 2020;20(6):871–8.
Carroll ML, DiMiceli CM, Sohlberg RA, Townshend JR. 250m MODIS normalized difference vegetation index. College Park, MD: University of Maryland; 2004.
O’Neil-Dunne JP, Grove JM. A report on the City of Philadelphia’s existing and possible tree canopy. Washington, DC: USDA Forest Service; 2011.
Philadelphia Land Cover Raster 2018. University of Vermont Spatial Analysis Laboratory. http://www.pasda.psu.edu/uci/DataSummary.aspx?dataset=3193. Accessed November 7, 2016.
National Land Cover Database. www.mrlc.gov. Accessed April 19, 2016.
American Community Survey (ACS0509 & ACS1216). U.S. Census. https://www.census.gov/programs-surveys/acs. Accessed 2018
Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. New Engl Journal Med. 2001;345:99–106.
Berrocal VJ, Gelfand AE, Holland DM. A spatio-temporal downscaler for output from numerical models. J Agric Biol Environ Stat. 2010;15(2):176–97.
Berrocal VJ, Gelfand AE, Holland DM. Space-time data fusion under error in computer model output: an application to modeling air quality. Biometrics. 2012;68(3):837–48.
NOAA, National Centers for Environmental Information. https://www.ncdc.noaa.gov/cdo-web/datatools/lcd. Accessed 2017–2018.
National Asthma Education and Prevention Program. Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Heart Lung and Blood Institute. 2007. Available from https://www.ncbi.nml.gov/books/NBK7232/. Accessed October 2021
Pearsall H, De Roos AJ, Dickinson S, et al. The benefits and costs of urban public spaces. Philadelphia, PA: William Penn Foundation, 2020. https://williampennfoundation.org/what-we-are-learning/benefits-and-costs-urban-public-spaces. Accessed November 3, 2021.
Kanchongkittiphon W, Mendell MJ, Gaffin JM, Wang G, Phipatanakul W. Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environ Health Perspect. 2015;123(1):6–20.
Acknowledgements
This study is part of the Pediatric Big Health Data initiative funded by the State of Pennsylvania and led by the Children’s Hospital of Philadelphia, University of Pennsylvania, and the Urban Health Collaborative at Drexel University. We would like to thank the investigators of the Pediatric Big Health Data initiative for their contributions. These individuals include the following: Christopher B. Forrest, MD, PhD; L. Charles Bailey, MD, PhD; Shweta P. Chavan, MSEE; Rahul A. Darwar, MPH; Jillian Benedetti, MPH; Daniel Forsyth; Chén C. Kenyon, MD, MSHP; Ritu Khare, PhD; Mitchell G. Maltenfort, PhD; Aaron J. Masino, PhD, ME; Xueqin Pang, PhD; Ting Qian, PhD; Hanieh Razzaghi, MPH; Justine Shults, PhD; Levon H. Utidjian, MD, MBI from the Children’s Hospital of Philadelphia; Ana V. Diez Roux, MD, PhD, MPH; Amy H. Auchincloss, PhD, MPH; Elizabeth A. Campbell, MSPH; Kimberly Daniels, MS; Anneclaire J. De Roos, PhD, MPH; J. Felipe Garcia-Espana, MS, PhD; Irene Headen, PhD, MS; Félice Lê-Scherban, PhD, MPH; Steven Melly, MS, MA; Yvonne L. Michael, ScD, SM; Jeffrey Moore, MS; Kari Moore, MS; Abigail E. Mudd, MPH; Leah Schinasi, PhD, MSPH; and Yuzhe Zhao, MS from Drexel University and, Yong Chen, PhD; John H. Holmes, PhD; Rebecca A. Hubbard, PhD; A. Russell Localio, JD, MPH, PhD from the University of Pennsylvania.
This work was supported by a grant from the Commonwealth Universal Research Enhancement (C.U.R.E) program funded by the Pennsylvania Department of Health—2015 Formula award—SAP #4100072543.
Anneclaire J. De Roos would like to acknowledge the Whiteley Center at the University of Washington Friday Harbor Laboratories for providing a peaceful and inspirational setting in which to complete the bulk of this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De Roos, A.J., Kenyon, C.C., Yen, YT. et al. Does Living near Trees and Other Vegetation Affect the Contemporaneous Odds of Asthma Exacerbation among Pediatric Asthma Patients?. J Urban Health 99, 533–548 (2022). https://doi.org/10.1007/s11524-022-00633-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-022-00633-7