Abstract
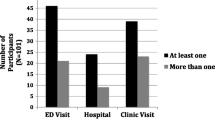
Release from short-term jail detention is highly destabilizing, associated with relapse to substance use, recidivism, and disrupted health care continuity. Little is known about emergency department (ED) use, potentially a surrogate for medical, psychiatric, or social instability, by people living with HIV/AIDS (PLWHA) leaving jails. All ED visits were reviewed from medical records for a cohort of 109 PLHWA in the year following release from county jail in Connecticut, between January 1, 2008 and December 31, 2010. Primary outcomes were frequency and timing of ED visits, modeled using multivariate negative binomial regression and Cox proportional hazards regression, respectively. Demographic, substance use, and psychiatric disorder severity factors were evaluated as potential covariates. Overall, 71 (65.1 %) of the 109 participants made 300 unique ED visits (2.75 visits/person-year) in the year following jail-release. Frequency of ED use was positively associated with female sex (incidence rate ratios, IRR 2.40 [1.36–4.35]), homelessness (IRR 2.22 [1.15–4.41]), and recent substance use (IRR 2.47 [1.33–4.64]), and inversely associated with lifetime drug severity (IRR 0.01 [0–0.10]), and being retained in HIV primary care (IRR 0.80 [0.65–0.99]). Those in late or sustained HIV care used the ED sooner than those not retained in HIV primary care (median for late retention 16.3 days, median for sustained retention 24.9 days, median for no retention not reached at 12 months, p value 0.004). Using multivariate modeling, those who used the ED earliest upon release were more likely to be homeless (HR 1.98 [1.02–3.84]), to be retained in HIV care (HR 1.30 [1.04–1.61]), and to have recently used drugs (HR 2.51 [1.30–4.87]), yet had a low lifetime drug severity (HR 0.01 [0.00–0.14]). Among PLWHA released from jail, frequency of ED use is high, often soon after release, and is associated with social and drug-related destabilizing factors. Future interventions for this specific population should focus on addressing these resource gaps, ensuring housing, and establishing immediate linkage to HIV primary care after release from jail.



Similar content being viewed by others
References
Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. Plos One. 2009; 4(11): A16–A21.
Flanigan T, Zaller N, Beckwith CG, et al. Testing for HIV, sexually transmitted infections, and viral hepatitis in jails: still a missed opportunity for public health and HIV prevention. J Acquir Immune Defic Syndr. 2010; 55(Suppl 2): S78–S83.
de Voux A, Spaulding AC, Beckwith C, et al. Early identification of HIV: empirical support for jail-based screening. PLoS One. 2012; 7(5): e37603.
Montague BT, Rosen DL, Solomon L, et al. Tracking linkage to HIV care for former prisoners. A public health priority. Virulence. 2012; 3(3): 319–324.
Draine J, Ahuja D, Altice FL, et al. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. Aids Care. 2011; 2011: 23(3).
Kavasery R, Altice FL. Observations on implementing routine HIV testing in jails. AIDS Patient Care and STDS. 2007; 21(10): 715–716.
Pai NP, Estes M, Moodie EEM, Reingold AL, Tulsky JP. The impact of antiretroviral therapy in a cohort of HIV infected patients going in and out of the San Francisco County Jail. Plos One. 2009; 4: 1.
Rapp R, Ciomcia R, Zaller N, Draine J, Ferguson A, Cagey R. The role of jails in engaging PLWHA in care: from jail to community. AIDS Behav. 2013; 17(Suppl 2): S89–99.
Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: five essential components. Clin Infect Dis. 2011; 53: 469–79.
Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004; 38(12): 1754–1760.
Stephenson BL, Wohl DA, Golin CE, Tien HC, Stewart P, Kaplan AH. Effect of release from prison and re-incarceration on the viral loads of HIV-infected individuals. Public Health Rep. 2005; 120(1): 84–88.
Palepu A, Tyndall MW, Chan K, Wood E, Montaner JSG, Hogg RS. Initiating highly active antiretroviral therapy and continuity of HIV care: the impact of incarceration and prison release on adherence and HIV treatment outcomes. Antivir Ther. 2004; 9(5): 713–719.
Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of human immunodeficiency virus treatment during incarceration: viral suppression at the prison gate. JAMA Intern Med. 2014; 174: 721–9.
Althoff A, Zelenev A, Meyer J, et al. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS Behav. 2013; 17(Suppl 2): S156–70.
Springer SA, Chen S, Altice FL. Improved HIV and substance abuse treatment outcomes for released HIV-infected prisoners: the impact of buprenorphine treatment. J Urban Health. 2010; 87(4): 592–602.
Binswanger IA. Release from prison—a high risk of death for former inmates (vol 356, pg 157, 2007). N Engl J Med. 2007; 356(5): 536–536.
Krishnan A, Wickersham JA, Chitsaz E, et al. Post-release substance abuse outcomes among HIV-infected jail detainees: results from a multisite study. AIDS Behav. 2013; 17(Suppl 2): S171–180.
Schwarcz SK, Hsu LC, Vittinghoff E, Vu A, Bamberger JD, Katz MH. Impact of housing on the survival of persons with AIDS. BMC Public Health Jul. 2009; 9: 18.
Williams BA, McGuire J, Lindsay RG, et al. Coming home: health status and homelessness risk of older pre-release prisoners. J Gen Intern Med. 2010; 25(10): 1038–1044.
Zelenev A, Marcus R, Kopelev A, et al. Patterns of homelessness and implications for HIV health after release from jail. AIDS Behav. 2013; 17(Suppl 2): S181–194.
Baillargeon J, Giordano TP, Harzke AJ, et al. Predictors of reincarceration and disease progression among released HIV-infected inmates. AIDS Patient Care STDS. 2010; 24: 389–94.
Fu JJ, Herme M, Wickersham JA, et al. Understanding the revolving door: individual and structural-level predictors of recidivism among individuals with HIV leaving jail. AIDS Behav. 2013; 17(Suppl 2): S145–155.
Meyer JP, Wickersham JA, Fu JJ, et al. Partner violence and health among HIV-infected jail detainees. Int J Prison Health. 2013; 9(3): 124–141.
Weir BW, O'Brien K, Bard RS, et al. Reducing HIV and partner violence risk among women with criminal justice system involvement: a randomized controlled trial of two motivational interviewing-based interventions. AIDS Behav. 2009; 13(3): 509–522.
Wu E, El-Bassel N, Gilbert L, Sarfo B, Seewald R. Criminal justice involvement and service need among men on methadone who have perpetrated intimate partner violence. J Crim Justice. 2010; 38(4): 835–840.
Meade CS, Hansen NB, Kochman A, Sikkema KJ. Utilization of medical treatments and adherence to antiretroviral therapy among HIV-positive adults with histories of childhood sexual abuse. AIDS Patient Care STDS. 2009; 23(4): 259–266.
Josephs JS, Fleishman JA, Korthuis PT, Moore RD, Gebo KA, Network HIVR. Emergency department utilization among HIV-infected patients in a multisite multistate study*. HIV Medicine. 2010; 11(1): 74–84.
Masson CL, Sorensen JL, Phibbs CS, Okin RL. Predictors of medical service utilization among individuals with co-occurring HIV infection and substance abuse disorders. AIDS Care. 2004; 16(6): 744–755.
Mauskopf J, Turner BJ, Markson LE, Houchens RL, Fanning TR, McKee L. Patterns of ambulatory care for AIDS patients, and association with emergency room use. Health Services Research. 1994; 29(4): 489–510.
Kidder DP, Wolitski RJ, Campsmith ML, Nakamura GV. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007; 97(12): 2238–2245.
Sohler NL, Wong MD, Cunningham WE, Cabral H, Drainoni ML, Cunningham CO. Type and pattern of illicit drug use and access to health care services for HIV-infected people. AIDS Patient Care STDS. 2007; 21: S68–S76.
Wohl DA, Scheyett A, Golin CE, et al. Intensive case management before and after prison release is no more effective than comprehensive pre-release discharge planning in linking HIV-infected prisoners to care: a randomized trial. AIDS Behav. 2011; 15: 356–64.
Meyer JP, Qiu J, Chen NE, Larkin GL, Altice FL. Emergency department use by released prisoners with HIV: an observational longitudinal study. Plos One. 2012; 7: e42416.
Meyer JP, Qiu JJ, Chen NE, Larkin GL, Altice FL. Frequent emergency department use among released prisoners with human immunodeficiency virus: characterization including a novel multimorbidity index. Acad Emerg Med. 2013; 20(1): 79–88.
Chen NE, Meyer JP, Avery AK, et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2013; 17(8): 2654–2666.
Chitsaz E, Meyer JP, Krishnan A, et al. Contribution of substance use disorders on HIV treatment outcomes and antiretroviral medication adherence among HIV-infected persons entering jail. AIDS Behav. 2013; 17(Suppl 2): S118–127.
Nunn A, Cornwall A, Fu J, Bazerman L, Loewenthal H, Beckwith C. Linking HIV-positive jail inmates to treatment, care, and social services after release: results from a qualitative assessment of the COMPASS program. J Urban Health. 2010; 87: 954–68.
Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000; 34(6): 1273–1302.
Spaulding AC, Messina LC, Kim BI, et al. Planning for success predicts virus suppressed: results of a non-controlled, observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS Behav. 2013; 17(Suppl 2): S203–211.
Williams CT, Kim S, Meyer J, et al. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV-positive clients leaving jail. AIDS Behav. 2013; 17(Suppl 2): S195–202.
Meyer JP, Zelenev A, Wickersham JA, Williams CT, Teixeira PA, Altice FL. Gender disparities in HIV treatment outcomes following release from jail: results from a multicenter study. Am J Public Health. 2014; 104(3): 434–441.
McLellan AT, Luborsky L, Cacciola J, et al. New data from the Addiction Severity Index—reliability and validity in 3 centers. J Nerv Ment Dis. 1985; 173(7): 412–423.
McLellan AT, Kushner H, Metzger D, et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treatment. 1992; 9(3): 199–213.
Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): a review of recent research. Alcohol Clin Exp Res. 2002; 26(2): 272–279.
Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test: an update of research findings. Alcohol Clin Exp Res. 2007; 31(2): 185–199.
Rikoon SH, Cacciola JS, Carise D, Alterman AI, McLellan AT. Predicting DSM-IV dependence diagnoses from Addiction Severity Index composite scores. J Subst Abuse Treat. 2006; 31(1): 17–24.
Calsyn DA, Saxon AJ, Bush KR, et al. The Addiction Severity Index medical and psychiatric composite scores measure similar domains as the SF-36 in substance-dependent veterans: concurrent and discriminant validity. Drug Alcohol Depend. 2004; 76(2): 165–171.
Reelick NF, Wierdsma AI. The addiction severity index as a predictor of the use of mental health care. Psychol Addict Behav. 2006; 20(2): 214–218.
Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003; 54(5): 573–583.
Qualitymetric. SF36v2 Health Survey; 2010.
Huba G ML, Staff of the Measurement Group, HRSA/HAB’s SPNS Cooperative Agreement Steering Committee. Module 46: social support form. The Measurements Group. http://themeasurementgroup.com/modules/mods/module46.htm. Accessed April 20, 2012.
Freburger JK, Callahan LF, Currey SS, Anderson LA. Use of the trust in physician scale in patients with rheumatic disease: psychometric properties and correlates of trust in the rheumatologist. Arthritis Rheum. 2003; 49(1): 51–58.
Springer SA, Qiu J, Saber-Tehrani AS, Altice FL. Retention on buprenorphine is associated with high levels of maximal viral suppression among HIV-infected opioid dependent released prisoners. PLoS One. 2012; 7(5): e38335.
Dupont W. Statistical Modeling for Biomedical Researchers: a Simple Introduction to the Analysis of Complex Data. 2nd ed. New York, NY: Cambridge University Press; 2009.
Gelman A, Hill J. Data Analysis Using Regression and Multilevel/Hierarchical Models. Cambridge, NY: Cambridge University Press; 2007.
Jaeger M. On testing the missing at random assumption. In: Fürnkranz J, Scheffer T, Spiliopoulou M, editors. Machine Learning: ECML 2006. Vol 4212. Berlin: Springer; 2006. p. 671–678.
Honaker J, King G, Blackwell M. Amelia II: a program for missing data. Journal of Statistical Software. 2011; 45(7): 1–47.
Akaike H. Information theory as an extension of the maximum likelihood principle. In: Petrov BN, Csaki F, eds. Second International Symposium on Information Theory. Budapest: Akademiai Kiado; 1973.
Collett D. Modeling Survival Data in Medical Research. 2nd ed. Boca Raton, FL: Champan & Hall/CRC; 2003.
Su Y, Yajima M, Gelman AE, Hill J. Multiple imputation with diagnostics (mi) in R: opening windows into the black box. J Stat Softw. 2011; 45(2): 1–31.
State of Connecticut Office of Policy and Management. 2009 Connecticut Recidivism Study: 2004 Release Cohort. http://www.ct.gov/bopp/lib/bopp/20090215_recidivismstudy.pdf. Accessed May 11, 2013.
Courtenay-Quirk C, Pals SL, Kidder DP, Henny K, Emshoff JG. Factors associated with incarceration history among HIV-positive persons experiencing homelessness or imminent risk of homelessness. J Community Health. 2008; 33(6): 434–443.
Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: imprisonment among the homeless and marginally housed population. Am J Public Health. 2005; 95(10): 1747–1752.
Kim TW, Kertesz SG, Horton NJ, Tibbetts N, Samet JH. Episodic homelessness and health care utilization in a prospective cohort of HIV-infected persons with alcohol problems. BMC Health Serv Res. 2006; 6: 19.
Parashar S, Palmer AK, O'Brien N, et al. Sticking to it: the effect of maximally assisted therapy on antiretroviral treatment adherence among individuals living with HIV who are unstably housed. Aids and Behavior. 2011; 15(8): 1612–1622.
Fontaine JGD, Roman J, Taxy S, Roman C. Supportive Housing for Returning Prisoners: Outcomes and Impacts of the Returning Home—Ohio Pilot Project. Washington, DC: The Urban Institute; 2012.
Frank JW, Linder JA, Becker WC, Fiellin DA, Wang EA. Increased hospital and emergency department utilization by individuals with recent criminal justice involvement: results of a national survey. J Gen Intern Med. 2014 Sep;29(9):1226–33. doi:10.1007/s11606-014-2877-y.
Wang EA, Hong CS, Samuels L, Shavit S, Sanders R, Kushel M. Transitions clinic: creating a community-based model of health care for recently released California prisoners. Public Health Rep. 2010; 125(2): 171–177.
Lincoln T, Kennedy S, Tuthill R, Roberts C, Conklin TJ, Hammett TM. Facilitators and barriers to continuing healthcare after jail: a community-integrated program. J Ambul Care Manage. 2006; 29(1): 2–16.
Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: a randomized trial. Am J Public Health. 2012; 102(9): e22–29.
Kinner SA, Lennox N, Williams GM, et al. Randomised controlled trial of a service brokerage intervention for ex-prisoners in Australia. Contemp Clin Trials. 2013; 36(1): 198–206.
French MT, McGeary KA, Chitwood DD, McCoy CB. Chronic illicit drug use, health services utilization and the cost of medical care. Soc Sci Med. 2000; 50(12): 1703–1713.
McGeary KA, French MT. Illicit drug use and emergency room utilization. Health Serv Res. 2000; 35(1 Pt 1): 153–169.
Pollack HA, Khoshnood K, Blankenship KM, Altice FL. The impact of needle exchange-based health services on emergency department use. J Gen Intern Med. 2002; 17(5): 341–348.
Frank JW, Andrews CM, Green TC, Samuels AM, Trinh TT, Friedmann PD. Emergency department utilization among recently released prisoners: a retrospective cohort study. BMC Emerg Med. 2013; 13: 16.
Altice FL, Bruce RD, Lucas GM, et al. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J Acquir Immune Defic Syndr. 2011; 56(Suppl 1): S22–32.
Schwarz R, Zelenev A, Bruce RD, Altice FL. Retention on buprenorphine treatment reduces emergency department utilization, but not hospitalization, among treatment-seeking patients with opioid dependence. J Subst Abus Treat. 2012; 43(4): 451–457.
Sherman SS, Plitt S, ul Hassan S, Cheng Y, Zafar ST. Drug use, street survival, and risk behaviors among street children in Lahore, Pakistan. J Urban Health. 2005; 82(3): 113–124.
Collaborative AESR. The impact of screening, brief intervention and referral for treatment in emergency department patients' alcohol use: a 3-, 6- and 12-month follow-up. Alcohol Alcohol. 2010; 45(6): 514–519.
Acknowledgments
We would like to thank Ruthanne Marcus for logistical assistance and Maua Herme for data management, as well as Sasha Klein for data collection. We also thank study participants, without whom this work would not be possible. Enhancing Linkages to HIV Primary Care Services Initiative was a HRSA-funded Special Project of National Significance. Funding for this research was also provided through career development grants from the National Institute on Drug Abuse (K24 DA017072, FLA; and K23 DA033858 for JPM). The funding sources played no role in study design, data collection, analysis, or interpretation, writing of the manuscript, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boyd, A.T., Song, D.L., Meyer, J.P. et al. Emergency Department Use among HIV-Infected Released Jail Detainees. J Urban Health 92, 108–135 (2015). https://doi.org/10.1007/s11524-014-9905-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-014-9905-4