Abstract
Background
Palbociclib in combination with endocrine therapy is approved for treatment of hormone receptor-positive (HR+)/human epidermal growth factor receptor 2-negative (HER2−) advanced breast cancer. In addition to clinical trials, several real-world studies have evaluated the effectiveness of palbociclib. With increased life expectancy in the general population, breast cancer in older women is also expected to increase.
Objective
The aim was to systematically review evidence from both clinical trials and real-world studies for palbociclib treatment outcomes in older patients with HR+/HER2− advanced/metastatic breast cancer (a/mBC). Older patients are often underrepresented in clinical trials, and real-world evidence (RWE) will enrich the analysis of palbociclib outcomes in this subgroup of patients.
Design
A systematic literature search in PubMed, EMBASE, and Cochrane Library through May 4, 2023, yielded 2355 unique articles. A total of 52 articles (13 and 39 articles reporting results from seven randomized controlled trials [RCTs] and 37 RWE studies, respectively) were included based on study eligibility criteria.
Results
All RCTs used age cutoffs of ≥ 65 years to define older population (n = 722; 437 received palbociclib); all RWE studies, except one with an age cutoff of > 60 years, had age cutoffs of ≥ 65 years or higher to define older population (n = 9840; 7408 received palbociclib). Overall, in studies that compared efficacy (progression-free survival [seven RCTs, 20 RWE studies], overall survival [four RCTs, 11 RWE studies], tumor response [three RWE studies], and clinical benefit rate [one RCT, two RWE studies]) and safety outcomes (three RCTs, three RWE studies) between older and younger patients, palbociclib showed similar benefits, regardless of age. Results from two RCTs and two RWE studies showed that global quality of life (QoL) was maintained in older patients receiving palbociclib. Overall, palbociclib dose modifications (two RWE studies), dose reductions (one RCT, seven RWE studies), and treatment discontinuation rates (three RCTs, three RWE studies) were higher in older patients compared with younger patients; however, these differences did not appear to adversely impact efficacy outcomes.
Conclusions
In this systematic review, data from RCTs showed that palbociclib was effective, well tolerated, and maintained QoL in older patients with HR+/HER2− a/mBC. Palbociclib treatment in older patients in real-world settings was associated with similar clinical benefit as in RCTs.
PROSPERO Registration
CRD42023444195.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This systematic review assessed all available randomized controlled trial (RCT) and real-world evidence for use and outcomes of palbociclib in older patients with hormone receptor-positive (HR+)/human epidermal growth factor receptor 2-negative (HER2−) metastatic breast cancer. |
In RCTs, palbociclib was effective, well tolerated, and preserved quality of life (QoL) regardless of age in patients with HR+/HER2− metastatic breast cancer. |
Real-world studies complemented findings from RCTs with similar findings; furthermore, real-world studies supplemented efficacy and safety data from clinical trials and demonstrated that QoL remained stable with palbociclib treatment in older patients. |
1 Introduction
Female breast cancer is the most common cancer worldwide, with an estimated 2.3 million new cases diagnosed in 2020 [1]. Age is a known risk factor for many types of cancer, including breast cancer [2]. In 2022, 60% of invasive breast cancers diagnosed in the United States (US) and almost three-quarters of breast cancer-related deaths were among patients aged 60 years or older [3]. With an aging population and increasing cancer incidence with age, cancer incidence in the 65 years or older population in the US is estimated to increase by 67% from 2010 to 2030 [4]. Despite comprising a large proportion of breast cancer patients, older patients have historically been underrepresented in clinical trials for new cancer drugs [5, 6]. Because of this disparity, clinical guidelines for the treatment of breast cancer among older adults are largely based on evidence from younger patients who may have different disease characteristics and prognoses. Also, management of older patients with breast cancer is challenging due to comorbidities and frailty that often overlap with advanced age [7, 8].
Hormone receptor-positive (HR+)/human epidermal growth factor receptor 2-negative (HER2–) breast cancer is the most common molecular subtype overall, and it is also the most common molecular subtype among older patients and those with advanced/metastatic breast cancer (a/mBC). The current recommended first- and second-line treatment for patients with HR+/HER2– a/mBC is a cyclin-dependent kinase (CDK) 4/6 inhibitor (e.g., palbociclib, ribociclib, or abemaciclib) in combination with endocrine therapy (ET). Palbociclib was the first CDK 4/6 inhibitor approved by the US Food and Drug Administration (FDA) in 2015 and by the European Medicines Agency (EMA) in 2016 for the treatment of HR+/HER2– a/mBC; palbociclib is currently approved globally for use in combination with an aromatase inhibitor (AI) as a first-line ET and in combination with fulvestrant for disease progression after ET. Although expert consensus from the International Society of Geriatric Oncology (SIOG) and the European Society of Breast Cancer Specialists (EUSOMA) recommends geriatric assessment-guided care, with recently updated guidelines for the treatment of breast cancer in older adults, the evidence regarding the efficacy and safety of CDK 4/6 inhibitors for these patients is scarce and based primarily on descriptive studies rather than randomized controlled trials (RCTs) [9, 10]. RCTs often have inclusion and exclusion criteria that directly or indirectly limit eligibility of older patients. Data on older patients are often supplemented post approval with additional clinical trial data or data from the real-world setting; evidence from both RCTs and real-world settings complement each other to provide a comprehensive overview of outcomes in this patient population. Since its FDA approval in 2015, palbociclib has accumulated a large body of real-world evidence (RWE). As a comprehensive review of palbociclib outcomes in older adults with HR+/HER2− a/mBC is lacking, we conducted a systematic review of both RCT and real-world studies to understand the totality of evidence for palbociclib treatment in older patients with HR+/HER2− a/mBC.
2 Methods
This systematic review follows the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) collaboration [11] and was prospectively registered with PROSPERO (CRD42023444195).
2.1 Data Sources and Searches
A comprehensive literature search using PubMed, EMBASE, and Cochrane Library was conducted to identify studies that evaluated palbociclib in older patients with HR+/HER2− a/mBC. Metastatic breast cancer is defined as breast cancer that has spread to other parts of the body, such as the liver, brain, bones, or lungs [12]; advanced breast cancer comprises both locally irresectable advanced breast cancer and metastatic breast cancer [13]. Search dates for these three databases ranged from database inception through May 4, 2023. Google Scholar was used for gray literature searches; targeted searches of the following relevant conferences covering the previous 2-year period were also conducted: Academy of Managed Care Pharmacy Nexus, American Society of Clinical Oncology Annual Meeting, European Society for Medical Oncology (ESMO) Congress, ESMO Breast Cancer, ESMO Asia, International Society for Pharmacoeconomics and Outcomes Research (ISPOR), ISPOR European Union, Miami Breast Cancer Conference, National Comprehensive Cancer Network Annual Conference, and San Antonio Breast Cancer Symposium. The following keywords were used: breast cancer, breast carcinoma, palbociclib, and Ibrance. Searches were not restricted by publication date, published language, or type of publication (abstracts from conference proceedings or full-text publications).
2.2 Search Strategy
The following predetermined inclusion criteria were used: (1) phase 2 and phase 3 RCTs and RWE studies evaluating efficacy/effectiveness, safety, health-related quality of life (HRQoL), and patient-reported outcomes of palbociclib treatment in older patients (aged 60 years and older based on the United Nations definition for older population) [14] with HR+/HER2− a/mBC; (2) sample size of ten or more patients who received palbociclib; (3) ≥ 80% of the older patient population received palbociclib as the CDK inhibitor. Preclinical studies, studies in pediatric populations, review articles, case reports, and studies evaluating outcomes other than those listed in the inclusion criteria were excluded. The PubMed search string used was as follows: (“breast cancer”[Title/Abstract] OR “breast carcinoma”[Title/Abstract]) AND (“palbociclib”[Title/Abstract] OR “Ibrance”[Title/Abstract]).
2.3 Study Selection and Data Extraction
Duplicate articles were identified and excluded to obtain a unique list of articles. Two investigators independently screened the titles and abstracts of all articles for inclusion using the study eligibility criteria. Next, full texts of articles included from the title/abstract screening were reviewed and reasons for exclusion recorded. Disagreements on any study selection were discussed and resolved in consensus with one other investigator (VP).
Two reviewers independently extracted data from studies. The following information was extracted: study type (RCT, RWE), study design (study phase; retrospective, prospective), description of the population, study sample size, older population age cutoff, patient demographics, baseline breast cancer characteristics, comorbidities, prior treatment history, efficacy outcomes (progression-free survival [PFS], overall survival [OS], clinical benefit rate [CBR], tumor response, disease control rate, and time to chemotherapy), HRQoL outcomes, and safety outcomes (adverse events [AEs], treatment discontinuations, time to treatment failure, and dose modifications [including dose reductions, dose interruptions, and dose delays]). One other investigator (VP) reviewed the extractions for inconsistencies, and the three investigators reached consensus.
2.4 Evaluation of Study Quality
All full-text publications were evaluated for study quality by two investigators, and discrepancies were resolved in consensus with one other investigator (VP). The modified Jadad scale was used to evaluate quality of RCTs [15]. The evaluation criteria of the modified Jadad scale included four items: randomization, randomization concealment, double blind, and withdrawals and dropouts. A score 0−4 out of 8 was considered to indicate a low-quality study, and a score of > 4−8 was considered to indicate a high-quality study. The Newcastle-Ottawa scale (NOS) was used to assess quality of observational studies [16]. The NOS assigns a maximum of 4 points for study cohort selection, 2 points for comparability of cohorts, and 3 points for assessment of outcome. NOS scores of ≥ 7 were considered to indicate high-quality studies, NOS scores of 4−6 were considered to indicate moderate-quality studies, and NOS scores of < 4 indicated a low-quality study.
2.5 Data Synthesis and Analysis
A high degree of heterogeneity among studies was expected, and therefore, a formal quantitative synthesis (meta-analysis) was not planned. However, heterogeneity was explored using pre-specified subgroups based on type of study (RCTs vs real-word studies) and palbociclib line of therapy (first-line vs any line). All data were summarized descriptively.
3 Results
3.1 Search Results and Study Selection
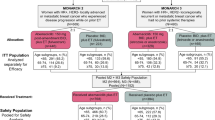
We identified 3603 records through the database search and ten records through other sources; 1258 duplicate articles were removed (Fig. 1). Following the first phase of the screening by article title/abstract, 328 records were selected for full-text review, and among those records, 52 articles (13 publications reporting results from seven RCTs; 39 publications [11 abstracts from conference proceedings; 28 full-text publications] reporting data from 37 RWE studies) were included in the qualitative synthesis. The reasons for exclusion of the remaining 276 articles are listed in Fig. 1.
3.2 Study Characteristics
Supplementary Table 1 in the electronic supplementary material summarizes the main characteristics of the included studies. Of the seven included RCTs, three were phase 2 studies [17,18,19,20] and four were phase 3 studies [21,22,23,24,25,26,27,28,29]; all seven RCTs defined older patients as ≥ 65 years of age and included a total of 722 older patients (as defined in individual studies). Across studies, 437 patients (range 14–181) received treatment with palbociclib. Study quality of the 11 full-text RCT publications assessed using the modified Jadad scale showed a median (range) score of 6 (4.5–8).
Most of the RWE studies were retrospective (n = 32) [30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]; three studies were prospective [60,61,62,63,64,65], and two were ambispective (retrospective and prospective) studies [66, 67]. Three retrospective studies using data from the Flatiron Health longitudinal database had different study time frames and populations (in terms of patient age); however, there remains a possibility of patient overlap across studies [35, 37, 52]. Older patients were defined as ≥ 60 years of age in one study [40], ≥ 65 years in 21 studies [30, 32, 34, 36,37,38,39, 42, 43, 45, 46, 49, 50, 52, 53, 56,57,58, 64, 65, 68], ≥ 70 years in 11 studies [31, 44, 47, 48, 54, 55, 59,60,61,62,63, 66, 67], and ≥ 75 years in four studies [33, 35, 41, 51]. Three studies evaluated CDK 4/6 inhibitors as a class; however, ≥ 80% of the patients received palbociclib as the CDK 4/6 inhibitor [43, 58, 67]. A total of 9840 older patients (as defined in individual studies) were included across RWE studies; 7408 patients (range 11–1415) received treatment with palbociclib. Study quality of the 28 full-text RWE publications assessed using NOS showed a median (range) score of 6 (5–8).
3.3 Patient Characteristics in Included Studies
Older (aged ≥ 65 years) patients comprised 32% (722 of 2228) of the total number of patients in the seven RCTs. In PALOMA-1, PALOMA-2, and PALOMA-3, patients aged ≥ 75 years comprised 9% (83 of 875) of the total patient population [27]. Patient demographics and baseline characteristics in older patients who received palbociclib were presented in only the pooled PALOMA analysis [27]. Among these older patient subgroups (aged 65−74 years and aged ≥ 75 years) in the pooled PALOMA analysis, the proportion of White patients ranged from 75.9 to 100%; the proportions of patients with Eastern Cooperative Oncology Group performance status (ECOG PS) scores of 0, 1, and 2 were 22.2–58.6%, 40.6–77.8%, and 0–4.2%, respectively; patients with de novo metastasis ranged from 0% to 62.5%; and patients with visceral metastasis and bone-only metastasis ranged from 41.4% to 75% and 12.5% to 27.1%, respectively.
Of the included 37 RWE studies, seven included only older patients [37, 41, 43, 59,60,61,62,63]. Among RWE studies including both younger and older patients, six studies provided data on the proportion of patients aged ≥ 75 years (31% [1960 of 6380]) [36, 37, 45, 46, 51, 52]. Data from a total of 12 studies for patient demographics and baseline characteristics in older patients who received palbociclib were limited and heterogeneous (most studies only described the total patient population). The most commonly reported variables were as follows: median age (ten studies; range 72–82.9 years); ECOG PS score (seven studies; score ranges: 0: 23.6–58.1%; 1: 24.1–57%; 2: 6.6–18.5%; and ≥ 2: 9.8–17.9%); location of metastatic sites (seven studies; proportion ranges: visceral metastasis: 33.9–53.1%; bone-only metastasis: 32.1–39.3%); proportion of patients with de novo metastasis (seven studies; range 11.8–63.3%); prior treatment history (six studies); Charlson Comorbidity Index (CCI) score (five studies); breast cancer staging (four studies); number of metastatic sites (four studies); White race (three studies; proportion range 68.4–78.0%); and frailty score (three studies).
3.4 Progression-Free Survival
The PFS data for both older and younger patient subgroups were reported in all seven RCTs (Fig. 2A). In one single-arm phase 2 study evaluating palbociclib plus letrozole in the first-line setting, median PFS was comparable between the older and younger patients, although no test for significance was conducted [17]. In three RCTs, PFS was significantly improved with palbociclib (plus fulvestrant in FLIPPER; plus letrozole in PALOMA-1 and PALOMA-2) in the first-line setting compared with control treatment (fulvestrant in FLIPPER; letrozole in PALOMA-1 and PALOMA-2) in both older and younger patients [18, 19, 24]. In PALOMA-3, PFS was significantly improved with palbociclib plus fulvestrant regardless of line of therapy compared with placebo plus fulvestrant among patients aged < 65 years and 65−74 years but not in those ≥ 75 years; however, there were only 33 patients included in the ≥ 75 years subgroup in that analysis [27]. In PEARL, an RCT with a chemotherapy control arm, palbociclib plus ET (exemestane or fulvestrant) regardless of line therapy showed similar PFS benefit compared to capecitabine in both younger and older patients [22].
Of the 26 RWE studies (nine in first-line setting; 15 regardless of line of therapy; line of therapy not specified in two studies) that reported PFS data, 20 studies compared results between older and younger patients (Table 1). In 16 studies, there was no significant difference in real-world progression-free survival (rwPFS) between younger and older patients who received treatment with palbociclib [34, 38, 39, 46,47,48,49, 51,52,53, 55, 56, 58, 59, 65, 67, 68]. In three studies, rwPFS benefit was comparable between younger and older patients; however, no test for significance was conducted [45, 50, 66]. In one study, rwPFS rate at 12 months was significantly longer in patients ≥ 65 years of age versus patients aged < 65 years [64]. Six studies included only older patients [33, 35, 37, 41, 59, 60]; in one study using multivariable regression, age (as a continuous variable) was not a significant predictor of rwPFS [41]. In all three RWE studies with a control arm (two of these three studies included only older patients [35, 37]), older patients treated with palbociclib had significantly longer rwPFS compared with control treatment [35, 37, 52]. Of note, all three studies were controlled for potential biases by using stabilized inverse probability of treatment weighting or propensity score matching or both [35, 37, 52].
3.5 Overall Survival
The OS data for both older and younger patient subgroups were reported in four RCTs (Fig. 2B). In PALOMA-3, older patients who received palbociclib showed an OS benefit compared with fulvestrant monotherapy control arm, whereas younger patients did not show an OS benefit [25]. In PALOMA-2, the secondary endpoint of OS was numerically longer in patients who received palbociclib compared with the control arm; however, the results were not statistically significant. OS was similar in older patients who received palbociclib versus the control arm (hazard ratio 0.871, 95% confidence interval [CI] 0.624–1.216) [29]. In PALOMA-1, although not statistically significant, OS results were similar in both younger and older patients who received palbociclib [20]. In PEARL, similar OS was seen in younger and older patients, but OS was not different in both age subgroups compared to the control treatment [21].
Of the 15 RWE studies (six in first-line setting; eight regardless of line of therapy; line of therapy not specified in one study) that reported OS data, 11 studies compared results between older and younger patients (Table 2). Nine studies did not show a significant difference in OS between younger and older patients who received treatment with palbociclib [34, 38, 39, 44, 51, 52, 64, 65, 67]. In two studies, OS benefit was comparable between younger and older patients; however, no test for significant differences was conducted [49, 50]. Four studies included only older patients [35, 37, 41, 59]; one study using multivariable regression reported that age as a continuous variable was not a significant predictor of OS [41]. In all three studies with a control arm (two of these three studies included only older patients [35, 37]), older patients treated with palbociclib had significantly longer OS compared with control treatment [35, 37, 52].
3.6 Real-World Tumor Response and Clinical Benefit Rate
Real-world tumor response (rwTR) was reported in five RWE studies [36, 37, 41, 50, 66]. Older versus younger patients had similar rwTR in three studies that compared results between the two age groups [36, 50, 66]. PALOMA-1 showed comparable CBR among younger and older patients who received palbociclib (80.9% and 81.1%, respectively) [19].
Real-world CBR (rwCBR) was reported in three RWE studies; one study did not test for significant differences in rwCBR between younger and older patients [50]. In one RWE study, there was no significant difference in rwCBR between younger (< 65 years) and older (≥ 65 years) patients (P = 0.575) [68]. One other study reported significant rwCBR benefit with palbociclib plus fulvestrant in younger patients (< 70 years; P = 0.002) but not in older patients (≥ 70 years; P = 0.67) compared to fulvestrant [54]. Disease control rate was reported in one RWE study using medical charts data collected from patients in the National Cancer Center database in China [48]. Among patients who received palbociclib-containing therapy, disease control rate varied significantly among different age groups (P = 0.034): < 40 years, 60%; 40–70 years, 77.1%; and > 70 years, 82.3% [48].
3.7 Treatment Discontinuations
Three RCTs reported treatment discontinuation data for older patients who received palbociclib. In PALOMA-1, treatment discontinuation rate due to AEs was 13% (six of 46) in younger patients and 16.2% (six of 37) in older patients [19]. In the pooled PALOMA analysis, treatment discontinuation rate due to treatment-emergent AEs (TEAEs) was 1.6% (nine of 568), 5.4% (12 of 221), and 6.0% (five of 83) in patients aged < 65 years, 65−74 years, and ≥ 75 years, respectively [27].
Treatment discontinuation data for older patients who received palbociclib were reported in seven RWE studies [40, 41, 43, 50, 57, 59, 60, 62]. Of these studies, only three compared data between older and younger patients [40, 50, 57]. In a retrospective medical chart review evaluating clinical outcomes in patients receiving palbociclib, treatment discontinuation rates were 13% in older patients (> 65 years; n = 71) and 17% in younger patients (≤ 65 years; n = 91) [50]. In a study to assess tolerability of palbociclib in younger (< 60 years) and older patients (≥ 60 years), the most common reasons for treatment discontinuation were disease progression (85% vs 66%), intolerance other than neutropenia (6% vs 20%), and neutropenia (4% vs 5%), respectively [40]. In a retrospective study evaluating palbociclib adherence and persistence, older patients (65–74 years and 75+ years) had a significantly increased likelihood of treatment discontinuation compared with younger patients (18–50 years) [57].
In the Gouton et al. and El Badri et al. studies, the most common reasons for treatment discontinuation in older patients (> 70 years and ≥ 75 years, respectively) were disease progression (71% and 47%) followed by toxicity (15% and 26%) [41, 59]. In the PalomAGE study (patients aged ≥ 70 years) cohort B (ET-resistant and/or later lines of advanced breast cancer), the palbociclib discontinuation rate at 6 months was 29% (including 18% due to progression and 4% due to toxicity); the treatment discontinuation rate by palbociclib starting dose 125/100/75 mg was 28%, 31%, and 35%, respectively [62]. In PalomAGE study cohort A (ET-sensitive and first-line treatment for advanced breast cancer), older patients who received palbociclib had an 18-month treatment discontinuation rate of 42% (including 21% due to disease progression and 8% due to toxicity); the treatment discontinuation rate by palbociclib starting dose 125/100/75 mg was 39%, 50%, and 61%, respectively [60]. Median rwPFS was 28.1 months (95% CI 25.6–not reached) [60]. In a SEER-Medicare population-based study, an exploratory subgroup analysis of CDK 4/6 inhibitors (87% received palbociclib) across all lines of therapy showed that patients aged ≥ 65 years had a discontinuation rate (including discontinuations due to progression or toxicity) of 69% during the study period and a time to discontinuation of 9.4 months (standard deviation 8.9) [43].
3.8 Dose Modifications and Dose Reductions
Dose adjustment/modification data for older patients who received palbociclib were reported in three RWE studies [35, 42, 50]. Of these studies, two compared data between older and younger patients [42, 50]. In a chart review study of patients receiving palbociclib plus ET, palbociclib dose modification/delay rate was comparable in older patients (≥ 65 years) versus younger patients (< 65 years) (39% [12 of 31] vs 38% [26 of 69], respectively) [42]. In a retrospective medical chart review evaluating clinical outcomes in patients receiving palbociclib, dose adjustment rate (including dose reduction, increase, interruption, or delay) was 23% (16 of 71) in older patients (> 65 years) and 11% (ten of 91) in younger patients (≤ 65 years) [50]. In a study assessing treatment patterns and effectiveness of palbociclib in patients aged ≥ 75 years (n = 306), palbociclib was initiated at 125 mg/day in 75% of patients, and 40% of patients experienced dose adjustment [35].
Only one RCT reported palbociclib dose reduction data in older patients. In PALOMA-1, dose reduction due to AEs among patients who received palbociclib was reported in 38% of older patients (≥ 65 years) and 39% of younger patients (< 65 years) [19].
Dose reduction data for older patients who received palbociclib were reported in 13 RWE studies. Of these studies, seven compared data between older and younger patients [32, 34, 39, 40, 44, 50, 67]. In five studies, older patients in comparison with younger patients had a higher rate of dose reductions with no detrimental effect on survival outcomes [32, 39, 44, 50, 67]. In a study evaluating the impact of palbociclib dose reductions on rwPFS, 38% of older patients (≥ 65 years) and 31% of younger patients (< 65 years) had dose reductions; however, rwPFS was not inferior in patients whose dose was reduced versus those whose dose was not reduced in either age group [32]. In a study that retrospectively examined toxicities and outcomes of older patients receiving palbociclib, the number of dose reductions was significantly higher in patients aged ≥ 65 years versus < 65 years (P < 0.05) and in patients aged ≥ 70 years versus < 70 years (P < 0.0001) [39]. The ≥ 70 years group had a significantly improved rwPFS compared with the younger group (P = 0.02), but age was no longer a significant variable in the multivariate analysis [39]. In a study evaluating the effect of palbociclib dose reductions on clinical outcomes, older patients had more frequent dose reductions (≥ 70 years, 39%; < 70 years, 30%; P = 0.041), but this did not appear to affect OS [44]. Similarly, an Asian study assessing real-world outcomes from use of CDK4/6 inhibitors (95% of the study population received palbociclib) found that patients aged ≥ 70 years were more likely to require dose reductions; however, a reduced starting dose was not significantly associated with a reduced rwPFS [67]. In a study assessing clinical outcomes in patients receiving palbociclib plus ET, 15% of older patients (> 65 years) and 10% of younger patients (≤ 65 years) had dose reductions; the effectiveness (objective response rate [ORR], rwPFS, and OS) of palbociclib plus ET did not depend on age [50]. In a study examining treatment patterns and outcomes in older patients receiving palbociclib plus ET, palbociclib dose reductions occurred in 40% of the patients, with neutropenia as the most common reason, similar for both age groups (< 65 and ≥ 65 years); there was no statistically significant difference in rwPFS and OS between the two groups [34]. In a study assessing tolerability of palbociclib in older and younger patients with advanced breast cancer, there were no significant differences in dose reductions (≥ 60 years, 51% vs < 60 years, 46%; P = 0.61) [40].
The other six RWE studies that reported dose reductions reported data on palbociclib dose reductions in older patients only [33, 41, 42, 56, 59, 60, 62]. Dose reductions in older patients across these studies ranged from 9% to 60%. In the Zhang et al. study, 9% of the patients aged ≥ 65 years had palbociclib dose reductions from 125 mg/day to 100 mg/day; there was no PFS difference according to dosage reduction of palbociclib (P = 0.361) [56]. In a study of patients aged ≥ 75 years, 51% of patients required a palbociclib dose reduction, of which 54% were due to neutropenia and 21% due to fatigue; on multivariable analysis, dose reductions had no significant effect on rwPFS (P = 0.391), although a significant effect on OS was observed (P = 0.026) [41].
3.9 Dose Delays
Data for palbociclib dose delays in older patients who received palbociclib were reported in six RWE studies. Of these studies, four compared data between older and younger patients [32, 39, 50, 67]. In a study assessing clinical outcomes in patients receiving palbociclib plus ET, dose delays were seen in 4% of older patients (> 65 years) and 1% of younger patients (≤ 65 years); the effectiveness (ORR, rwPFS, and OS) of palbociclib plus ET did not depend on age [50]. In Karuturi et al., older patients had a higher rate of dose delays (≥ 65 years, 58%; < 65 years, 42%); however, patients in either age cohort did not experience a detriment to rwPFS [32]. In a study of a cohort of older patients compared with a younger patient population receiving palbociclib, the number of dose delays was significantly higher in patients aged ≥ 65 years versus < 65 years (P < 0.05) and in patients aged ≥ 70 years versus < 70 years (P < 0.0001); on multivariable analysis, age was not associated with rwPFS [39]. In the Low et al. study, 74% of patients aged ≥ 70 years required at least one dose delay; however, age did not impact rwPFS or OS [67]. In two studies evaluating palbociclib dose delays in patients aged ≥ 75 years, 59% and 73% of patients required at least one dose delay; neutropenia was the primary cause of dose delays in both studies [33, 41].
3.9.1 Safety
AE data by age subgroups (younger vs older patients) were reported from three RCTs [19, 27]. In PALOMA-1, the incidence of grade 3/4 AEs was similar in the two age groups (80.4% in < 65 years vs 73.0% in ≥ 65 years) [19]. In the pooled PALOMA analysis, no new safety concerns were identified in older patients. In older patients, hematological TEAEs occurred more frequently in patients receiving palbociclib versus comparator; however, most of these were grade 1 or 2, except for neutropenia and leukopenia [27]. In patients aged ≥ 75 years, myelosuppression was more common; however, incidence of grade 3 or higher AEs was similar across age groups [27].
Safety outcomes were inconsistently reported in RWE studies, with limited data from eight studies [30, 39, 41, 51, 59,60,61,62,63, 65]. In three studies, no significant differences in toxicities were observed among younger versus older patients [39, 51, 65]. In PalomAGE, no new safety signals were observed in patients aged ≥ 70 years; palbociclib-related grade 3/4 AEs were seen in 40.1% of patients aged < 80 years versus 31.4% in patients aged ≥ 80 years [63]. In a study evaluating hematological toxicities with palbociclib treatment, the risk of palbociclib-induced neutropenia was higher in patients aged > 65 years (P < 0.001) [30]. In a study evaluating palbociclib plus an AI in patients ≥ 75 years, neutropenia was the most frequent AE, with all grade neutropenia and grade ≥ 3 neutropenia occurring in 80.8% and 46.4% of patients, respectively [41]. In a study evaluating palbociclib plus ET in patients > 70 years, neutropenia was the most frequent AE, with all-grade neutropenia and grade 3–4 neutropenia occurring in 73% and 63% of patients, respectively [59]. A study of a French pharmacovigilance database from August 2016 to December 2019 reviewed records of 227 cases of AEs in patients; among patients of ≥ 70 years of age, 58 AEs (54%) were considered serious adverse events (SAEs), with one death and two life-threatening events, compared with 84 SAEs (70%) in patients < 70 years of age, including three deaths and five life-threatening events [59]. The most frequently reported treatment-related SAEs were similar in both age groups (43% in each) and were predominantly hematological in nature. Although no statistical comparisons were performed between older and younger patients, patterns and characteristics of SAEs were similar in both age groups.
3.9.2 Health-Related Quality of Life
Data on HRQoL outcomes by age subgroups (younger versus older patients) were reported in two RCTs (Table 3). Among patients receiving palbociclib in PALOMA-2, there was no significant deterioration in well-being scale or total Functional Assessment of Cancer Therapy – Breast (FACT-B) scores in patients aged 65−74 and ≥ 75 years [27]. Similarly, in PALOMA-3, patients aged 65−74 and ≥ 75 years maintained global quality of life (QoL) and did not show significant differences between treatment arms in functioning or symptoms, except for appetite loss in patients aged ≥ 75 years, for which a greater deterioration was observed in patients who received palbociclib [27].
Two RWE studies reported HRQoL data in older patients who received palbociclib (Table 3). Both of these studies used geriatric assessments and QoL questionnaires to evaluate global health status and QoL over time. In PalomAGE study cohort A, no significant difference was seen across all domains of the Geriatric Core Dataset (DIALOG G-CODE) at baseline between patients who stopped treatment at 18 months and those who did not [60]. Among patients who completed QoL assessment (European Organisation for Research and Treatment of Cancer [EORTC] QLQ-C30 and QLQ-ELD14 questionnaires) at baseline and at 18 months, the scores in both questionnaires appeared to remain stable [60]. In PalomAGE study cohort B, there was an improvement at 6 months in the nutritional and psychological status and a stability over time of the other geriatric domains [62]. The QoL assessments showed that the global QoL remained stable during the first 6 months of the study [62]. In POLARIS, Geriatric8 (G8) and activities of daily living scores were generally maintained during the first 6 months of therapy, indicating functional status was preserved in older patients receiving palbociclib [31].
4 Discussion
To our knowledge, this is the first systematic literature review to summarize all published data from RCTs and RWE for palbociclib in the treatment of older patients with HR+/HER2− a/mBC. Although there is not a consensus for the definition of an “older patient,” those aged ≥ 65 years are usually considered to be older in the context of clinical trials. All RCTs and RWE studies (except for one RWE study with an age cutoff of > 60 years) had age cutoffs of ≥ 65 years or higher to define the older population; the ≥ 65 years age cutoff was used in 57% (21 of 37) of the RWE studies. Although the definition of the older patient is currently being discussed due to the increasing life expectancy in the general population, a broad definition of older patient was employed in this review as it remains in common use.
This review indicated that in RCTs, palbociclib is effective and well tolerated in older patients with HR+/HER2− a/mBC who receive a similar clinical benefit compared to younger patients. RWE studies included more diverse study populations with regard to race, ECOG PS, CCI, and frailty scores, and with varying age cutoffs to define older patients, but overall had studied 14 times more older patients relative to the clinical trials. Patients were older in RWE studies compared with RCTs. In PALOMA-2 and PALOMA-3, the median age of patients who received palbociclib was 62 years and 57 years, respectively, while the largest RWE study population included in this review had a median age of 67 years [23, 52, 69]. In RWE studies, palbociclib plus ET was found to be an effective and well-tolerated treatment in the older patient population, associated with favorable clinical outcomes comparable to younger patients and with no detrimental impact on QoL. Although RWE studies enroll more older adults and are thought to present a more realistic picture of the patient population, there may still be biases toward healthier and more fit participants. In this context, defining older patients by chronological age may not be enough. There is a need to distinguish between biological versus physiological ageing and to identify age- or disease-related frailties that could be better managed in older patients with cancer [70]. Additionally, since chronological age may not accurately reflect physiological and functional status, a geriatric assessment-based approach in treatment decisions may improve outcomes in older patients with cancer [71]. Of note, although 68% of the patients in the PalomAGE study were considered frail (based on G8 scores at baseline), palbociclib was well tolerated with no impact on QoL [60, 62, 63].
Evidence from RCTs shows that patients across age groups derive similar benefit in PFS and OS from palbociclib. Evidence from RWE studies was consistent with that reported in RCTs; older patients had comparable rwPFS and OS outcomes versus younger patients. Findings from RWE studies are especially relevant due to their large pool of patients aged ≥ 70 years who are usually underrepresented in RCTs; only 9% of participants in breast cancer RCTs registered between 1985 and 2012 were aged ≥ 70 years [72].
In this review, the vast majority of studies with data reported for both older and younger patients showed higher rates of dose adjustments in older patients. However, these dose adjustments did not appear to lead to lower survival outcomes, and the magnitude of survival benefit was similar between older and younger patients. Dose modifications with anticancer therapies are common, and frequent dose modifications reflect the current drug development framework; most cancer therapies are developed by identifying their maximum tolerated dose, suggesting that a higher dose leads to better clinical outcomes [73]. Furthermore, the underrepresentation of specific populations in controlled trials such as older adults in cancer clinical trials, limits extrapolation of drug dosage from clinical trial results to these subpopulations. In this context, findings from this review of similar survival benefit in both older and younger patients despite higher rates of dose adjustments in older patients are of particular importance. Given the caveat that RWE studies are subject to selection bias and do not allow causal interpretations, these findings help provide the missing information from clinical trials on highly selected or controlled patient populations.
Safety data are crucial to inform treatment decisions for therapies used over extended time periods, especially in older patients with cancer who often have several comorbidities and take multiple medications [8, 74]. The most robust palbociclib safety data in older patients are from RCTs [27]. In PALOMA trials, higher rates of AEs and those leading to treatment discontinuation in older versus younger patients are not surprising, likely due to a higher prevalence of comorbidities and reduced tolerability in older patients [8]. The safety profile of palbociclib was comparable between older and younger patients in the few RWE studies that reported data from both age groups, and neutropenia was the most common AE. In two RWE studies, among older patients aged > 70 years and ≥ 75 years, respectively, rates of all-grade and grade 3/4 neutropenia ranged from 73% to 80.8% and 46.4% to 63% [41, 59]. These neutropenia rates were comparable or lower than those reported in the pooled PALOMA analysis wherein rates of all-grade and grade 3/4 neutropenia were 76.9% and 63.4%, respectively, in patients aged 65−74 years and 90.4% and 73.5%, respectively, in patients aged ≥ 75 years [27]. The generally similar safety profiles regardless of age group support treatment optimization implementing guidance by geriatric assessment. Geriatric assessment-guided care has been proven as a method to improve safety profiles for systemic treatment, improve treatment delivery, identify geriatric deficits for specific interventions, and ultimately improve QoL for older patients.
Preserving QoL for patients with breast cancer has gained prominence as a key treatment goal, and HRQoL is an important endpoint in breast cancer RCTs. Evaluating the quality of the time gained by delaying disease progression via geriatric assessments and QoL questionnaires is an important component of benefit–risk assessments. This is especially important in older patients with cancer who are more vulnerable to treatment toxicities due to factors such as comorbidities, drug interactions, or general health status. However, HRQoL data from RCTs and RWE studies are scarce. In PALOMA-2 and PALOMA-3, older patients who received palbociclib maintained global QoL, with no significant differences compared to younger patients [27]. HRQoL outcomes from real-world studies reflect how patients react to treatment in routine clinical practice. Given the use of QoL questionnaires that specifically have been validated in older populations to help understand their treatment experience, findings from RWE studies supplement and lend additional weight to HRQoL outcomes from RCTs [31, 60, 62]. Available data from RWE studies confirm that global QoL remained stable, and functional status was preserved in older patients who received palbociclib plus ET [31, 60, 62]. The maintenance of QoL in addition to greater efficacy and a favorable safety profile of palbociclib plus ET as compared to ET further support the use of palbociclib plus ET in older patients with HR+/HER2− a/mBC.
This review has several strengths and limitations. Several systematic reviews have evaluated the evidence for CDK4/6 inhibitors in the treatment of HR+/HER2− a/mBC [75,76,77,78,79]. Two narrative reviews and one systematic review of RCTs have explored the role of CDK4/6 inhibitors in the treatment of older patients with HR+/HER2− a/mBC [80,81,82]; however, there is no comprehensive systematic review on the evidence for palbociclib in older patients with HR+/HER2− a/mBC. This systematic review of the existing literature included both RCTs and observational studies and followed the PRISMA guidelines. Data from a large sample size of older patients (RCTs, n = 437; RWE studies, n = 7408) who received palbociclib for HR+/HER2− a/mBC were summarized in this review. Findings from real-world studies were generally consistent with clinical trials and further support the use of palbociclib plus ET in older patients with HR+/HER2− a/mBC.
Although a wide-ranging literature search for eligible studies was conducted, other studies may exist. Older population age cutoff varied across RWE studies, and not all outcomes of interest were explored by all included studies. As well, despite the SIOG and EUSOMA expert consensus recommendations for geriatric assessment-guided care to improve tolerance, HRQoL, and satisfaction in older patients [9], none of the studies used patients’ physiological age (versus chronological age) to guide treatment decisions. Given the heterogeneity in study designs, data were not synthesized using meta-analyses. Finally, comparisons between age groups in RWE studies should be interpreted with caution due to inherent limitations of observational studies, including biases, confounding factors, and the lack of rigorous outcome assessment as in clinical trials.
5 Conclusion
This review indicated that palbociclib in combination with ET is an effective and well tolerated treatment while preserving QoL for older patients with HR+/HER2− a/mBC; the clinical benefit profile of palbociclib in older patients in real-world settings was consistent with results seen in clinical trials.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
PDQ® Adult Treatment Editorial Board. PDQ Breast Cancer Treatment. Bethesda, MD: National Cancer Institute. Available from: https://www.cancer.gov/types/breast/hp/breast-treatment-pdq. Accessed 27 Nov 2023.
Giaquinto AN, Sung H, Miller KD, Kramer JL, Newman LA, Minihan A, et al. Breast cancer statistics, 2022. CA Cancer J Clin. 2022;72(6):524–41.
Shachar SS, Hurria A, Muss HB. Breast cancer in women older than 80 years. J Oncol Pract. 2016;12(2):123–32.
Singh H, Kanapuru B, Smith C, Fashoyin-Aje LA, Myers A, Kim G, et al. FDA analysis of enrollment of older adults in clinical trials for cancer drug registration: a 10-year experience by the U.S. Food and Drug Administration. J Clin Oncol. 2017;35(15_suppl):10009.
Talarico L, Chen G, Pazdur R. Enrollment of elderly patients in clinical trials for cancer drug registration: a 7-year experience by the US Food and Drug Administration. J Clin Oncol. 2004;22(22):4626–31.
Brain EGC. Systemic therapy in older patients with high-risk disease. Am Soc Clin Oncol Educ Book. 2023;43: e390456.
Extermann M. Measuring comorbidity in older cancer patients. Eur J Cancer. 2000;36(4):453–71.
Biganzoli L, Battisti NML, Wildiers H, McCartney A, Colloca G, Kunkler IH, et al. Updated recommendations regarding the management of older patients with breast cancer: a joint paper from the European Society of Breast Cancer Specialists (EUSOMA) and the International Society of Geriatric Oncology (SIOG). Lancet Oncol. 2021;22(7):e327–40.
ESO-ESMO 7th International Consensus Guidelines for Advanced Breast Cancer (ABC 7). 2023: https://www.abc-lisbon.org/en/abc%2dguidelines/1-415-1. Accessed 27 Nov 2023.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372: n160.
Breastcancer.org. Metastatic Breast Cancer (2022). https://www.breastcancer.org/symptoms/types/recur_metast. Accessed 27 Nov 2023.
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, Andre F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31(12):1623–49.
Swaminathan V, Audisio R. Cancer in older patients: an analysis of elderly oncology. Ecancermedicalscience. 2012;6:243.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Published 2000. Accessed 28 Aug 2023.
Takahashi M, Masuda N, Nishimura R, Inoue K, Ohno S, Iwata H, et al. Palbociclib-letrozole as first-line treatment for advanced breast cancer: Updated results from a Japanese phase 2 study. Cancer Med. 2020;9(14):4929–40.
Albanell J, Martinez MT, Ramos M, O’Connor M, de la Cruz-Merino L, Santaballa A, et al. Randomized phase II study of fulvestrant plus palbociclib or placebo in endocrine-sensitive, hormone receptor-positive/HER2-advanced breast cancer: GEICAM/2014-12 (FLIPPER). Eur J Cancer. 2022;161:26–37.
Finn RS, Crown JP, Ettl J, Schmidt M, Bondarenko IM, Lang I, et al. Efficacy and safety of palbociclib in combination with letrozole as first-line treatment of ER-positive, HER2-negative, advanced breast cancer: expanded analyses of subgroups from the randomized pivotal trial PALOMA-1/TRIO-18. Breast Cancer Res. 2016;18(1):67.
Finn RS, Boer K, Bondarenko I, Patel R, Pinter T, Schmidt M, et al. Overall survival results from the randomized phase 2 study of palbociclib in combination with letrozole versus letrozole alone for first-line treatment of ER+/HER2- advanced breast cancer (PALOMA-1, TRIO-18). Breast Cancer Res Treat. 2020;183(2):419–28.
Martin M, Zielinski C, Ruiz-Borrego M, Carrasco E, Ciruelos EM, Munoz M, et al. Overall survival with palbociclib plus endocrine therapy versus capecitabine in postmenopausal patients with hormone receptor-positive, HER2-negative metastatic breast cancer in the PEARL study. Eur J Cancer. 2022;168:12–24.
Martin M, Zielinski C, Ruiz-Borrego M, Carrasco E, Turner N, Ciruelos EM, et al. Palbociclib in combination with endocrine therapy versus capecitabine in hormonal receptor-positive, human epidermal growth factor 2-negative, aromatase inhibitor-resistant metastatic breast cancer: a phase III randomised controlled trial-PEARL. Ann Oncol. 2021;32(4):488–99.
Finn RS, Martin M, Rugo HS, Jones S, Im SA, Gelmon K, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375(20):1925–36.
Rugo HS, Finn RS, Dieras V, Ettl J, Lipatov O, Joy AA, et al. Palbociclib plus letrozole as first-line therapy in estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer with extended follow-up. Breast Cancer Res Treat. 2019;174(3):719–29.
Turner NC, Slamon DJ, Ro J, Bondarenko I, Im SA, Masuda N, et al. Overall survival with palbociclib and fulvestrant in advanced breast cancer. N Engl J Med. 2018;379(20):1926–36.
Verma S, Bartlett CH, Schnell P, DeMichele AM, Loi S, Ro J, et al. Palbociclib in combination with fulvestrant in women with hormone receptor-positive/HER2-negative advanced metastatic breast cancer: detailed safety analysis from a multicenter, randomized, placebo-controlled, phase III study (PALOMA-3). Oncologist. 2016;21(10):1165–75.
Rugo HS, Turner NC, Finn RS, Joy AA, Verma S, Harbeck N, et al. Palbociclib plus endocrine therapy in older women with HR+/HER2- advanced breast cancer: a pooled analysis of randomised PALOMA clinical studies. Eur J Cancer. 2018;101:123–33.
Xu B, Hu X, Li W, Sun T, Shen K, Wang S, et al. Palbociclib plus letrozole versus placebo plus letrozole in Asian postmenopausal women with oestrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer: primary results from PALOMA-4. Eur J Cancer. 2022;175:236–45.
Finn RS, Rugo HS, Dieras VC, Harbeck N, Im SA, Gelmon KA, et al. Overall survival (OS) with first-line palbociclib plus letrozole (PAL+LET) versus placebo plus letrozole (PBO+LET) in women with estrogen receptor–positive/human epidermal growth factor receptor 2–negative advanced breast cancer (ER+/HER2− ABC): analyses from PALOMA-2. J Clin Oncol. 2022;40:LBA1003-LBA.
Bitca V, Raimondi L, Gozzi L, Mannino A, Pietranera M, Spinelli GP, et al. Haematological toxicity in patients (pts) treated with palbociclib and fulvestrant (P+F): older age and prior adjuvant therapies as predictive factors of palbociclib-induced neutropenia. Tumori. 106:E31.
Karuturi MS, Blum JL, Wallmark J, McCune S, Lakhanpal S, Telivala B, et al. Measures of functional status in adults aged ≥70 years with advanced breast cancer (ABC) receiving palbociclib (PAL) combination therapy in POLARIS. Ann Oncol. 2019;30: v133.
Karuturi M, Katherine C, Kimmel J, Yi M. The impact of dose delays and reductions on progression free survival (PFS) in older patients with metastatic breast cancer receiving palbocilib. Eur J Cancer. 2018;92:S111.
Shah Y, El Badri S. Tolerability of Palbociclib plus aromatase inhibitor (AI) combination in women ≥75 years with oestrogen receptor positive (ER+ve), human epidermal growth factor receptor 2 negative (HER2-ve) advanced breast cancer at Mount Vernon Cancer Centre. J Oncol Pharm Pract. 2022;28:7–8.
Skrobo D, Prior L, Walshe J, Gullo G, Crown J. Patterns of treatment and outcomes in real world elderly patients with metastatic oestrogen receptor positive (ER+) breast cancer receiving the CDK4/6 inhibitor Palbociclib and endocrine therapy. Eur J Cancer. 2020;138:S102–3.
Brufsky A, Liu X, Li B, McRoy L, Chen C, Layman RM, et al. Real-world treatment patterns and effectiveness of palbociclib plus an aromatase inhibitor in patients with metastatic breast cancer aged 75 years or above. In: Miami Breast Cancer Conference® Abstracts Supplement. 2023;37:15.
Brufsky A, Liu X, Li B, McRoy L, Layman RM. Real-world tumor response of palbociclib plus letrozole versus letrozole for metastatic breast cancer in US Clinical Practice. Target Oncol. 2021;16(5):601–11.
Rugo HS, Liu X, Li B, McRoy L, Layman RM, Brufsky A. Real-world comparative effectiveness of palbociclib plus letrozole versus letrozole in older patients with metastatic breast cancer. Breast. 2023;69:375–81.
Carlino F, Diana A, Ventriglia A, Piccolo A, Mocerino C, Riccardi F, et al. HER2-low status does not affect survival outcomes of patients with metastatic breast cancer (MBC) undergoing first-line treatment with endocrine therapy plus palbociclib: results of a multicenter, retrospective cohort study. Cancers (Basel). 2022;14(20):4981.
Clifton K, Min Y, Kimmel J, Litton J, Tripathy D, Karuturi M. Progression-free survival (PFS) and toxicities of palbociclib in a geriatric population. Breast Cancer Res Treat. 2019;175(3):667–74.
Dennison T, Heiling H, Deal A, Brunk K, Kemper R, Crona DJ, et al. Tolerability of palbociclib in younger and older patients with advanced breast cancer. J Oncol Pharm Pract. 2023;29(1):96–104.
El Badri S, Tahir B, Balachandran K, Bezecny P, Britton F, Davies M, et al. Palbociclib in combination with aromatase inhibitors in patients >/= 75 years with oestrogen receptor-positive, human epidermal growth factor receptor 2 negative advanced breast cancer: a real-world multicentre UK study. Breast. 2021;60:199–205.
Gong J, Cho M, Yu KW, Waisman J, Yuan Y, Mortimer J. A single institution experience with palbociclib toxicity requiring dose modifications. Breast Cancer Res Treat. 2018;168(2):381–7.
Goyal RK, Chen H, Abughosh SM, Holmes HM, Candrilli SD, Johnson ML. Overall survival associated with CDK4/6 inhibitors in patients with HR+/HER2- metastatic breast cancer in the United States: a SEER-Medicare population-based study. Cancer. 2023;129(7):1051–63.
Ismail RK, van Breeschoten J, Wouters M, van Dartel M, van der Flier S, Reyners AKL, et al. Palbociclib dose reductions and the effect on clinical outcomes in patients with advanced breast cancer. Breast. 2021;60:263–71.
Law JW, Mitra D, Kaplan HG, Alfred T, Brufsky AM, Emir B, et al. Real-world treatment patterns and clinical effectiveness of palbociclib plus an aromatase inhibitor as first-line therapy in advanced/metastatic breast cancer: analysis from the US Syapse Learning Health Network. Curr Oncol. 2022;29(2):1047–61.
Lee J, Park HS, Won HS, Yang JH, Lee HY, Woo IS, et al. Real-world clinical data of palbociclib in asian metastatic breast cancer patients: experiences from eight institutions. Cancer Res Treat. 2021;53(2):409–23.
Manso L, Hernando C, Galan M, Oliveira M, Cabrera MA, Bratos R, et al. Palbociclib combined with endocrine therapy in heavily pretreated HR(+)/HER2(-) advanced breast cancer patients: results from the compassionate use program in Spain (PALBOCOMP). Breast. 2020;54:286–92.
Mo H, Ma F, Li Q, Zhang P, Yuan P, Wang J, et al. Treatment patterns and clinical outcomes in patients with metastatic breast cancer treated with palbociclib-based therapies: real-world data in the Han population. Chin Med J (Engl). 2022;135(14):1734–41.
Mycock K, Hanson KA, Taylor-Stokes G, Milligan G, Atkinson C, Mitra D, et al. Real-world treatment patterns and clinical outcomes associated with palbociclib combination therapy: a multinational, pooled analysis from the Ibrance Real World Insights Study. Clin Ther. 2022;44(12):1588–601.
Waller J, Mitra D, Mycock K, Taylor-Stokes G, Milligan G, Zhan L, et al. Real-World treatment patterns and clinical outcomes in patients receiving palbociclib for hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced or metastatic breast cancer in Argentina: the IRIS Study. J Glob Oncol. 2019;5:JGO1800239.
Pizzuti L, Giordano A, Michelotti A, Mazzotta M, Natoli C, Gamucci T, et al. Palbociclib plus endocrine therapy in HER2 negative, hormonal receptor-positive, advanced breast cancer: A real-world experience. J Cell Physiol. 2019;234(6):7708–17.
Rugo HS, Brufsky A, Liu X, Li B, McRoy L, Chen C, et al. Real-world study of overall survival with palbociclib plus aromatase inhibitor in HR+/HER2- metastatic breast cancer. NPJ Breast Cancer. 2022;8(1):114.
Sampedro-Gimeno T, Pampin-Sanchez R, Barbazan-Vazquez FJ, Reguero-Cuervo V, Galeazzi-Martinez V, Pelaez-Fernandez I. Observational real world data with palbociclib associated to hormone therapy for advanced breast carcinoma. Farm Hosp. 2021;45(6):329–34.
Seki H, Sakurai T, Maeda Y, Oki N, Aoyama M, Yamaguchi R, et al. Efficacy and safety of palbociclib and fulvestrant in Japanese patients with ER+/HER2- advanced/metastatic breast cancer. In Vivo. 2019;33(6):2037–44.
Shen L, Zhou J, Chen Y, Ding J, Wei H, Liu J, et al. Treatment patterns, effectiveness, and patient-reported outcomes of palbociclib therapy in Chinese patients with advanced breast cancer: a multicenter ambispective real-world study. Cancer Med. 2022;11(22):4157–68.
Zhang Y, Chen W, Chen S, Yang Q, Ouyang Z. Early application of palbociclib plus endocrine therapy in HR+/HER2- metastatic breast cancer: a better choice based on data from the chinese population. Technol Cancer Res Treat. 2022;21:15330338221132926.
Engel-Nitz NM, Johnson MG, Johnson MP, Cha-Silva AS, Kurosky SK, Liu X. Palbociclib adherence and persistence in patients with hormone receptor positive/human epidermal growth factor receptor 2 negative (HR+/HER2-) metastatic breast cancer. Patient Prefer Adherence. 2023;17:1049–62.
Knudsen ES, Schultz E, Hamilton D, Attwood K, Edge S, O’Connor T, et al. Real-world experience with CDK4/6 inhibitors for metastatic HR+/HER2- breast cancer at a single cancer center. Oncologist. 2022;27(8):646–54.
Gouton E, Tassy L, Micallef J, Meskine A, Sabatier R, Cecile-Herry M, et al. The safety and efficacy of palbociclib in older patients with advanced breast cancer in a real-world setting. J Cancer Metastasis Treat. 2022;8:33.
Carola E, Pulido M, Falandry C, Paillaud E, Caillet P, Tassy L, et al. First-line systemic treatment with palbociclib in women aged ≥70 years presenting with hormone receptor-positive advanced breast cancer: Results from the PALOMAGE program. J Clin Oncol. 2023;41:1018.
Bouteiller F, Pulido M, Brain E, Paillaud E, Grosjean J, Mina W, et al. Feasibility of palbociclib in women aged 70 and older with resistant and/or pretreated advanced breast cancer in the PALOMAGE study. Rev Epidemiol Sante Publique. 2022;70:S64–5.
Brain E, Pulido M, Paillaud E, Grosjean J, Mina W, Caillet P, et al. Feasibility of palbociclib in women aged 70 and older with resistant and/or pretreated advanced breast cancer in the PALOMAGE study. Cancer Res. 2022;82:P1-18–04.
Caillet P, Pulido M, Brain E, Falandry C, Desmoulins I, Ghebriou D, et al. PALOMAGE, a French real-world cohort of elderly women beyond age 70 with advanced breast cancer receiving palbociclib: Baseline characteristics and safety evaluation. J Clin Oncol. 2021;39:1012.
Cabel L, Rosenblum D, Lerebours F, Brain E, Loirat D, Bergqvist M, et al. Plasma thymidine kinase 1 activity and outcome of ER+ HER2- metastatic breast cancer patients treated with palbociclib and endocrine therapy. Breast Cancer Res. 2020;22(1):98.
Palumbo R, Torrisi R, Sottotetti F, Presti D, Rita Gambaro A, Collova E, et al. Patterns of treatment and outcome of palbociclib plus endocrine therapy in hormone receptor-positive/HER2 receptor-negative metastatic breast cancer: a real-world multicentre Italian study. Ther Adv Med Oncol. 2021;13:1758835920987651.
Anton FM, Bellet-Ezquerra M, Sanchez LMM, Carrasco FH, TorresMorales AAS, et al. Real-world treatment patterns and outcomes of patients receiving palbociclib plus endocrine therapy in Spain: Subgroup analysis based on age, sites and number of metastatic locations, menopausal status and dose received from PALBOSPAIN study. 2023;8(1): 101422.
Low JL, Lim E, Bharwani L, Wong A, Wong K, Ow S, et al. Real-world outcomes from use of CDK4/6 inhibitors in the management of advanced/metastatic breast cancer in Asia. Ther Adv Med Oncol. 2022;14:17588359221139678.
Zhong B, Zhang J, Wu J, Sun L, Li S, Zeng X, et al. Efficacy and safety of palbociclib plus endocrine therapy for patients with HR(+)/HER2(-) advanced breast cancer in real-world clinical practice. Ann Transl Med. 2022;10(6):362.
Turner NC, Ro J, Andre F, Loi S, Iwata H, Harbeck N, et al. PALOMA3: A double-blind, phase III trial of fulvestrant with or without palbociclib in pre- and post-menopausal women with hormone receptor-positive, HER2-negative metastatic breast cancer that progressed on prior endocrine therapy. J Clin Oncol. 2015;33:LBA502.
Jauhari Y, Gannon MR, Dodwell D, Horgan K, Tsang C, Clements K, et al. Addressing frailty in patients with breast cancer: a review of the literature. Eur J Surg Oncol. 2020;46(1):24–32.
Soto-Perez-de-Celis E, Li D, Yuan Y, Lau YM, Hurria A. Functional versus chronological age: geriatric assessments to guide decision making in older patients with cancer. Lancet Oncol. 2018;19(6):e305–16.
Freedman RA, Foster JC, Seisler DK, Lafky JM, Muss HB, Cohen HJ, et al. Accrual of older patients with breast cancer to alliance systemic therapy trials over time: protocol A151527. J Clin Oncol. 2017;35(4):421–31.
Shah M, Rahman A, Theoret MR, Pazdur R. The drug-dosing conundrum in oncology—when less is more. N Engl J Med. 2021;385(16):1445–7.
Balducci L, Goetz-Parten D, Steinman MA. Polypharmacy and the management of the older cancer patient. Ann Oncol. 2013;247(Suppl 7):36–40.
Li Y, Li L, Du Q, Li Y, Yang H, Li Q. Efficacy and safety of CDK4/6 inhibitors combined with endocrine therapy in HR+/HER-2- ABC patients: a systematic review and meta-analysis. Cancer Invest. 2021;39(5):369–78.
Hu Q, Kang W, Wang Q, Luo T. Role of CDK4/6 inhibitors in patients with hormone receptor (HR)-positive, human epidermal receptor-2 negative (HER-2) metastatic breast cancer study protocol for a systematic review, network meta-analysis and cost-effectiveness analysis. BMJ Open. 2022;12(5): e056374.
Harbeck N, Bartlett M, Spurden D, Hooper B, Zhan L, Rosta E, et al. CDK4/6 inhibitors in HR+/HER2- advanced/metastatic breast cancer: a systematic literature review of real-world evidence studies. Future Oncol. 2021;17(16):2107–22.
Howie LJ, Singh H, Bloomquist E, Wedam S, Amiri-Kordestani L, Tang S, et al. Outcomes of older women with hormone receptor-positive, human epidermal growth factor receptor-negative metastatic breast cancer treated with a CDK4/6 inhibitor and an aromatase inhibitor: an FDA Pooled Analysis. J Clin Oncol. 2019;37(36):3475–83.
Di Lauro V, Barchiesi G, Martorana F, Zucchini G, Muratore M, Fontanella C, et al. Health-related quality of life in breast cancer patients treated with CDK4/6 inhibitors: a systematic review. ESMO Open. 2022;7(6): 100629.
Pacilio C, Rosati G, Crispo A, Bimonte S, Dir F, Nuzzo F, et al. An overview of the roles of CDK4/6 inhibitors in metastatic breast cancer elderly patients. In Vivo. 2023;37(4):1445–9.
Battisti NML, De Glas N, Sedrak MS, Loh KP, Liposits G, Soto-Perez-de-Celis E, et al. Use of cyclin-dependent kinase 4/6 (CDK4/6) inhibitors in older patients with ER-positive HER2-negative breast cancer: Young International Society of Geriatric Oncology review paper. Ther Adv Med Oncol. 2018;10:1758835918809610.
Petrelli F, Dottorini L, Di Menna G, Borgonovo K, Parati MC, Rea CG, et al. The role of CDK4/6 inhibitors in older and younger patients with breast cancer: a systematic review and meta-analysis. Breast. 2023;71:138–42.
Acknowledgments
Editorial/medical writing support was provided by Oxford PharmaGenesis Inc. (Newtown, PA, USA) and was funded by Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This review was funded by Pfizer Inc.
Conflict of Interest
Etienne Brain has served as a consultant/advisor for Daiichi, Menarini, Pfizer Inc., and Sandoz; has received honoraria from Pfizer Inc., Eli Lilly, Incyte, and Seagen; has received travel support from Gilead, Pfizer Inc., AstraZeneca, and Novartis; and served on an advisory board for Daiichi. Connie Chen and Sofia Simon are employees of Pfizer Inc. Vinay Pasupuleti is an employee of Oxford PharmaGenesis Inc. Kathleen Vieira Pfitzer has no conflicts of interest to disclose. Karen A. Gelmon has served on an advisory board for Pfizer Inc, Novartis, Eli Lilly, Merck, Gilead, Seagan, Astra Zeneca, and City of Hope.
Data Availability
No new data were created or analyzed during this study. Data sharing is not applicable to this article.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Author Contributions
EB, CC, SF, VP, and KAG contributed to study conceptualization and design. CC, SF, and VP conducted the literature review and prepared the first draft of the manuscript. All authors reviewed, revised, and provided critical feedback on the manuscript. All authors provided final approval of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Brain, E., Chen, C., Simon, S. et al. Palbociclib in Older Patients with Advanced/Metastatic Breast Cancer: A Systematic Review. Targ Oncol 19, 303–320 (2024). https://doi.org/10.1007/s11523-024-01046-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-024-01046-z