Abstract
Background
Abiraterone acetate plus prednisone with androgen deprivation therapy is a standard treatment option for patients with high-risk metastatic castration-sensitive prostate cancer (mCSPC). However, no data are available on the optimal subsequent treatment option in patients treated with abiraterone acetate plus prednisone for high-risk mCSPC.
Objective
We aimed to compare the clinical outcomes of subsequent therapy after discontinuation of abiraterone acetate plus prednisone in patients with high-risk mCSPC.
Methods
Overall survival and time to treatment failure from initiation of subsequent therapies were estimated by applying a marginal structural Cox proportional hazards model using inverse probability of treatment weighting with a change of time scale to time on treatment.
Results
A total of 217 patients received subsequent therapies: 127 received chemotherapy, 49 received non-chemotherapy, and 41 received other treatments. For overall survival, when adjusted with the marginal structural Cox proportional hazards model using inverse probability of treatment weighting, the hazard ratio was 1.212 (95% confidence interval [CI] 0.742–1.979) for chemotherapy versus non-chemotherapy, 0.534 (95% CI 0.267–1.066) for non-chemotherapy versus other treatments, and 0.635 (95% CI 0.317–1.271) for chemotherapy versus other treatments. For time to treatment failure, the hazard ratio was 1.287 (95% CI 0.832–1.989) for chemotherapy versus non-chemotherapy, 0.785 (95% CI 0.486–1.269) for non-chemotherapy versus other treatments, and 0.898 (95% CI 0.612–1.318) for chemotherapy versus other treatments.
Conclusions
No differences were observed between the treatment effects of chemotherapy and non-chemotherapy in patients with high-risk mCSPC after abiraterone acetate plus prednisone. These findings suggest that life-extending subsequent therapy after abiraterone acetate plus prednisone for mCSPC should be chosen at the physician’s discretion and patient’s preference.
Clinical Trial Registration
ClinicalTrials.gov, NCT01715285, registered 26 October, 2012.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
No data are available on the clinical outcomes of subsequent therapies after discontinuation of abiraterone acetate plus prednisone in patients with metastatic castration-sensitive prostate cancer. |
No difference was observed between the clinical outcomes of different life-extending subsequent therapies in patients treated with abiraterone acetate plus prednisone for high-risk metastatic castration-sensitive prostate cancer who had progressed to metastatic castration-resistant prostate cancer, after applying a statistical adjustment for time-varying confounders. |
Our results show that patients who have previously received abiraterone acetate plus prednisone for metastatic castration-sensitive prostate cancer and who now have metastatic castration-resistant prostate cancer derive similar benefit from life-extending therapies, regardless of the type. |
1 Introduction
Abiraterone acetate plus prednisone (AAP) with androgen deprivation therapy is the standard treatment option for patients with high-risk metastatic castration-sensitive prostate cancer (mCSPC), and it reportedly improves overall survival (OS) [1, 2]. The treatment effects of AAP have been further confirmed in a post hoc analysis performed on LATITUDE (ClinicalTrials.gov, NCT01715285) study data, wherein treatment with AAP was shown to exert a benefit on OS over placebos in patients with high-risk mCSPC, regardless of whether life-extending subsequent therapy was given [3]. In addition, the STAMPEDE study and PEACE-1 study have shown that adding AAP to androgen deprivation therapy confers significant OS benefit in patients with mCSPC, although those enrolled in these studies had received an extensive variety of life-extending subsequent therapies [4, 5]. Optimal subsequent treatment options after AAP for metastatic castration-resistant prostate cancer (mCRPC) have been explored in various studies. For example, a randomized, open-label, phase II, crossover study reported that patients who received AAP followed by enzalutamide had a longer time to prostate-specific antigen (PSA) progression [6]. In another randomized phase III study, a post hoc analysis was conducted on patients who experienced disease progression after treatment with AAP, and patients who received docetaxel as the first subsequent therapy had favorable rates of PSA decline [7]. However, data on the optimal subsequent treatment options after AAP for mCSPC are yet to be reported.
The LATITUDE study was the first phase III study to examine the survival benefit of AAP addition to androgen deprivation therapy in patients with newly diagnosed high-risk mCSPC. This multinational, double-blind, randomized, placebo-controlled study involved 1199 men diagnosed with high-risk mCSPC. The study was unblinded shortly after the first interim analysis when a median follow-up of 30.4 months was completed, as significant and clinically meaningful improvements were observed in OS (hazard ratio, HR 0.62 [95% confidence interval (CI) 0.51–0.76]) and radiographic progression-free survival (HR 0.47 [95% CI 0.39–0.55]) [1]. In the final analysis performed after a median follow-up of 51.8 months, the OS continued to be longer in the AAP group than in the placebo group (HR 0.66 [95% CI 0.56–0.78]) [2]. After discontinuation of the study treatment, subsequent therapy for mCSPC was performed at the investigator’s discretion.
Comparing the treatment effects of each subsequent therapy performed in the LATITUDE study may provide useful information to physicians in selecting treatments for future patients. However, because the treatments to be provided after discontinuation of AAP were not specifically defined in the LATITUDE study, it would not be statistically appropriate to directly compare the treatment effects without any statistical adjustment, as the choice of subsequent therapy would have been affected by the investigators’ discretion and patients’ preference. Moreover, subsequent therapies were most likely chosen based on information not only from immediately before the initiation of subsequent therapies but also in consideration of the patients’ conditions during the treatment with AAP. Thus, adjustments for time-varying confounders are needed to properly estimate the subsequent treatment effects.
To overcome these limitations, we applied the marginal structural Cox proportional hazards model (Cox-MSM), which can estimate the survival time of patients receiving dynamic treatment regimens while adjusting for both baseline and time-varying confounders [8]. The inverse probability of treatment weighting (IPTW) method was used to estimate the weights for Cox-MSM, allowing us to represent a situation in which all patients in the AAP group had received a certain treatment, by weighting each patient by the inverse of his predicted probability of receiving this particular treatment at a given time. In addition, the time origin of the survival curve was shifted from the first day of study treatment to the first day of subsequent therapy, and the time scale was changed to time on treatment from time on study, according to a previous study, to estimate the target treatment duration (see formulas in the Electronic Supplementary Material [ESM]) [9]. This shift in time scale allows us to eliminate the treatment effects of AAP and focus on the treatment effects of subsequent therapies alone. This study aimed to make a statistically valid comparison of the treatment effects of subsequent therapies performed after AAP in the LATITUDE study using OS and time to treatment failure (TTF) by applying Cox-MSM with a change of time scale to time on treatment.
2 Materials and Methods
2.1 Data Sources
For this study, data were obtained from the results of the LATITUDE study. The final analysis datasets were used for the present study.
2.2 Study Population
This study included patients who were newly diagnosed with high-risk mCSPC. High risk was defined as having at least two of the following three factors: a Gleason score (GS) of 8 or more, at least three bone lesions, and presence of measurable visceral metastasis. Patients from 34 countries were enrolled in the LATITUDE study.
2.3 Statistical Analysis
In this study, statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA) in the intention-to-treat population of the AAP group in the LATITUDE study. The treatment variable comprised four categories, and patients were classified into one of the four categories according to the subsequent therapies that they received or did not receive after discontinuation of AAP. Patients treated with docetaxel or cabazitaxel were classified as ‘chemotherapy’, and those treated with enzalutamide, radium-223, or abiraterone as subsequent therapy were classified as ‘non-chemotherapy’. Patients receiving therapies other than those listed above were classified as ‘other treatments’, and those who were still continuing treatment with AAP (as the study treatment of the LATITUDE study) or those who discontinued AAP but did not receive any subsequent therapies were classified as ‘AAP’.
The probability of each patient receiving each of the subsequent therapies at each timepoint was estimated using IPTW (see formulas in the ESM). To estimate the weights, baseline covariates of age, GS, region, visceral metastases, PSA, and lactate dehydrogenase were used along with the time-varying covariates of the number of bone metastases, Brief Pain inventory-Short Form, Brief Fatigue Inventory, and time from study treatment modeled as restricted cubic splines [10]. For the sensitivity analysis, the same analyses were performed using the inverse probability of treatment and censoring (IPTC) weights in the Cox-MSM [8]. These weights for censoring were estimated from the same baseline and time-varying covariates, other than the GS, that were used to estimate the weight for IPTW.
All continuous variables are presented using descriptive statistics, including median/range or mean/standard deviation. All categorical variables are presented as frequency and percentage. Time-to-event endpoints were analyzed using the Nelson–Aalen method to estimate the survival distributions and median time to event [11]. Overall survival was defined as the time from initiation of subsequent therapies to death from any cause. Time to treatment failure was defined as the time from initiation of subsequent therapy to discontinuation of the treatment for any reason. Hazard ratio was estimated as an estimate of the treatment effect using a weighted Cox proportional hazards model. The Cox proportional hazards model was stratified by reason for discontinuation of study treatment and time to study treatment discontinuation (> 2 versus ≤ 2 years). All interval estimations were reported using 95% CIs. The last observation carried forward method was used to impute the missing values of time-varying covariates when the weights were estimated.
3 Results
3.1 Patient Disposition and Characteristics
In the LATITUDE study, 1199 patients were enrolled and randomized; of these, 597 were assigned to the AAP group. Although 380 patients were either undergoing treatment with AAP at the end of the follow-up or had discontinued AAP and were not receiving subsequent therapies, 217 patients had discontinued AAP and were receiving subsequent therapies, 176 patients were receiving one of the life-extending therapies, and 41 patients were receiving other treatments (Fig. 1). The most common reason for discontinuation in all treatments was progression of the disease, as determined by computed tomography/magnetic resonance imaging and bone scan, in accordance with the protocol of the LATITUDE study (89.0% [113/127] in chemotherapy, 57.1% [28/49] in non-chemotherapy, and 65.9% [27/41] in other treatments). Discontinuation because of adverse events was noted in 4.7% (6/127) patients classified as chemotherapy, 18.4% (9/49) patients classified as non-chemotherapy, and 2.4% (1/41) patients classified as other treatments.
Patient disposition. The figure shows patient disposition in the LATITUDE study. Of the 597 patients who were assigned to abiraterone acetate plus prednisone (AAP), 217 patients discontinued AAP and switched to subsequent therapies; 176 patients received one of the life-extending therapies, and 41 patients received other treatments
Patient characteristics are shown in Table 1. Patients who received other treatments were generally older. In terms of the GS, the proportion of patients with a GS above 8 was high in chemotherapy and non-chemotherapy at 61.4% (78/127) and 67.3% (33/49), respectively. A higher proportion of patients in the Western European region was subsequently treated with chemotherapy or non-chemotherapy. The proportion of patients who received other treatments was higher in Eastern Europe. Baseline PSA was higher among patients who received chemotherapy and lower among those who received non-chemotherapy.
3.2 Unadjusted OS and TTF Estimates
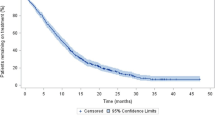
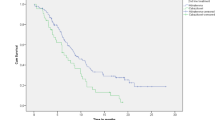
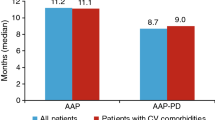
The unadjusted median OS estimated using the Nelson–Aalen method was 14.7 (95% CI 13.1–16.8) months in chemotherapy, 23.3 (95% CI 16.6–31.2) months in non-chemotherapy, and 10.3 (95% CI 4.0–15.4) months in other treatments (Fig. 2a). Regarding differences among the treatments, the unadjusted HR of OS was 1.754 (95% CI 1.162–2.649) for chemotherapy versus non-chemotherapy, 0.528 (95% CI 0.294–0.947) for non-chemotherapy versus other treatments, and 0.820 (95% CI 0.478–1.408) for chemotherapy versus other treatments (Table 2). Similarly, for TTF, the unadjusted median was 7.4 (95% CI 6.5–8.6) months in chemotherapy, 8.5 (95% CI 6.2–19.3) months in non-chemotherapy, and 8.3 (95% CI 3.9–10.9) months in other treatments (Fig. 2c). The unadjusted HR of TTF was 1.689 (95% CI 1.128–2.529) for chemotherapy versus non-chemotherapy, 0.672 (95% CI 0.413–1.093) for non-chemotherapy versus other treatments, and 1.073 (95% CI 0.699–1.649) for chemotherapy versus other treatments (Table 2).
Nelson–Aalen survival estimates, both unadjusted and adjusted for patients who received subsequent therapy in the abiraterone acetate plus prednisone (AAP) group, applying marginal structural Cox proportional hazards model (Cox-MSM) using the inverse probability of treatment weighting (IPTW) with change of time scale to time on treatment for each type of subsequent therapy: a unadjusted overall survival (OS); b adjusted OS; c unadjusted time to treatment failure (TTF); and d adjusted TTF. Patients at risk are presented on the unadjusted curve. Patients at risk are not included for the Cox-MSM using the IPTW curve because of a lack of a clear clinical interpretation of the number of patients at risk associated with the weighted methodology. NR not reached
3.3 OS and TTF Adjusted with Cox-MSM Using IPTW
When adjusted for covariates using the Cox-MSM using IPTW with a change of time scale to time on treatment, the median OS was 15.8 (95% CI 13.5–19.6) months in chemotherapy, 20.7 (95% CI 14.9–30.1) months in non-chemotherapy, and 12.4 (95% CI 4.0–NR) months in other treatments (Fig. 2b). Similarly, for TTF, the adjusted median was 7.2 (95% CI 6.3–8.4) months in chemotherapy, 8.1 (95% CI 5.7–16.7) months in non-chemotherapy, and 8.3 (95% CI 3.9–10.9) months in other treatments (Fig. 2d).
The HRs were also estimated after adjusting with Cox-MSM using IPTW with a change of time scale to time on treatment. The HR of OS was 1.212 (95% CI 0.742–1.979) for chemotherapy versus non-chemotherapy, 0.534 (95% CI 0.267–1.066) for non-chemotherapy versus other treatments, and 0.635 (95% CI 0.317–1.271) for chemotherapy versus other treatments (Table 2). For TTF, the adjusted HR was 1.287 (95% CI 0.832–1.989) for chemotherapy versus non-chemotherapy, 0.785 (95% CI 0.486–1.269) for non-chemotherapy versus other treatments, and 0.898 (95% CI 0.612–1.318) for chemotherapy versus other treatments (Table 2). The adjusted HRs for OS and TTF obtained using Cox-MSM based on the IPTW method for chemotherapy versus non-chemotherapy and chemotherapy versus other treatments were smaller than the unadjusted HR.
3.4 OS and TTF Adjusted with Cox-MSM Using IPTC
When adjusted for informative censoring bias in addition to the treatment switching with the Cox-MSM using IPTC with a change of time scale to time on treatment, the median OS was 15.8 (95% CI 13.5–19.8) months in chemotherapy, 21.1 (95% CI 13.9–30.1) months in non-chemotherapy, and 12.4 (95% CI 4.0–NR) months in other treatments (Fig. 1a of the ESM). The adjusted median TTF was 7.2 (95% CI 6.2–8.1) months in chemotherapy, 8.1 (95% CI 5.7–16.7) months in non-chemotherapy, and 9.4 (95% CI 3.9–10.9) months in other treatments (Fig. 1b of the ESM). The HRs were also estimated after adjusting with Cox-MSM using IPTC (Table 1 of the ESM). The HRs obtained after the Cox-MSM adjustment based on the IPTC method for OS and TTF were similar to those obtained using the IPTW method.
3.5 Association of Subsequent Therapies with Both Baseline and Time-Varying Covariates
When the associations between subsequent therapies and covariates were examined using odds ratios (ORs) estimated from the multinomial logistic regression model, the OR of chemotherapy versus non-chemotherapy was 2.440 (95% CI 1.200–4.959) for the baseline PSA and 0.298 (95% CI 0.120–0.741) for the baseline age. This indicated that patients with a higher baseline PSA and younger patients tended to receive chemotherapy (Table 2 of the ESM) compared with non-chemotherapy.
The estimated stabilized weights for the IPTW method are shown in Fig. 2 of the ESM. The median stabilized weight for chemotherapy was close to one, whereas that for non-chemotherapy and other treatments tended to be lower and higher than one, respectively.
4 Discussion
We compared the effects of subsequent therapies after discontinuation of treatment with AAP in patients with newly diagnosed high-risk mCSPC, using Cox-MSM to adjust time-varying confounders and changing the time scale to time on treatment to estimate time to event from initiation of subsequent therapy. In this study, for OS, the unadjusted HR for chemotherapy versus non-chemotherapy was significantly higher. However, no significant differences were noted when the HRs were adjusted with Cox-MSM using IPTW. Moreover, for TTF, the unadjusted HR for chemotherapy versus non-chemotherapy was significantly high; however, once the HR was adjusted with Cox-MSM using IPTW, no significant difference was observed. In other words, as a result of taking into account the time-varying confounders through the use of Cox-MSM and applying a change of time scale to time on treatment, this study demonstrated no differences in the subsequent treatment effect between chemotherapy and non-chemotherapy that patients with high-risk mCSPC receive after discontinuing AAP. The Cox-MSM and time scale change to time on treatment are commonly used for the estimation of treatment effects of dynamic treatment regimens in observational studies; however, to the best of our knowledge, this study is the first to apply these methods to compare subsequent therapies after study treatment discontinuation in a randomized controlled trial. With the unadjusted results, the subsequent non-chemotherapy seemed to have a better clinical outcome; however, after applying Cox-MSM and adjusting for time-varying confounders, the estimated subsequent treatment effect was smaller. It is assumed that by using Cox-MSM, the potential time-varying confounders could be properly adjusted, allowing for an unbiased estimate to be produced.
Docetaxel has been shown to be effective in symptomatic patients with mCRPC [12]. However, there is evidence of enzalutamide being effective only in minimally symptomatic or asymptomatic patients with mCRPC who have not received chemotherapy [13]. Therefore, physicians might choose docetaxel over enzalutamide for subsequent therapies, especially in symptomatic patients with mCRPC who are expected to have a poor prognosis. Such a result would be plausible when considering the estimates of the multinomial logistic regression model for IPTW in chemotherapy versus non-chemotherapy (OR for PSA, 2.440; OR for Brief Pain inventory-Short Form, 2.497; and OR for Brief Fatigue Inventory, 3.295). Regarding the results of Cox-MSM performed using IPTW, patients receiving other treatments had the shortest OS among those receiving the three treatments. Cumulative evidence has shown that chemotherapy and non-chemotherapy improve OS in patients with mCRPC, and these treatments have been recommended in treatment guidelines [14, 15]. These results suggest that selection of life-extending subsequent therapies is also important in patients treated with AAP for mCSPC who have progressed to mCRPC. Although there is currently no evidence indicating the optimal treatment for such patients, a previous study has reported that life-extending subsequent therapies after AAP for high-risk mCSPC performed on these patients contribute to longer OS [3].
In this study, no significant differences were observed in the treatment effects of life-extending subsequent therapies performed after AAP for high-risk mCSPC. The fact that AAP is the only selective irreversible inhibitor of CYP17 among the treatments available for prostate cancer could be contributing to this observation, as the mechanism of AAP would be different from the mechanism of any of the subsequent therapies. For example, the androgen receptor T878A mutation has been associated with acquired resistance to AAP [16]; however, enzalutamide has been found to be effective against this mutation [17]. Another example is plasma androgen receptor gain that causes resistance to AAP or enzalutamide [18]. Docetaxel has been found to be effective even in patients with androgen receptor gain [19]. These sequences of different mechanisms may have contributed to the favorable results.
In this study, we also examined whether bias occurred in the censoring of OS or TTF performed for each treatment. When Cox-MSM using IPTC was applied, we found that the results were consistent with those of the analysis performed with Cox-MSM using IPTW. This indicated that there was no bias in the censoring that was carried out in the subsequent therapies for OS or TTF (Fig. 2b, d, and Fig. 1 of the ESM). Considering that the LATITUDE study was a randomized controlled trial, the patients were most likely followed up in an appropriate manner as defined in the protocol. This could explain why censoring was balanced between treatments.
The strength of this study is that we were able to estimate the treatment effects of subsequent therapies using the intention-to-treat population of AAP group in the LATITUDE study. If we had applied a propensity score at a secondary baseline analysis, which performs statistical adjustments using baseline covariates from immediately before the initiation of subsequent therapies, then only patients who received subsequent therapies would be included in the analysis [20]. However, Cox-MSM adjusting for time-varying confounders was applied in this study, indicating that all information collected from the time of randomization to the initiation of subsequent therapy contributed to the estimation. This allowed the treatment selection process of physicians to be properly reflected in the model.
The assumption that there are no unmeasured confounders should be met to obtain valid results from a Cox-MSM analysis [21]. Both the baseline and time-varying covariates to be included in the model were chosen based on clinical importance. However, there is no way to confirm whether all the necessary covariates have been included in the IPTW model; only a randomized controlled trial may address this issue, and thus, the results should be carefully interpreted. Furthermore, model misspecification is unable to be confirmed and would be a limitation of our study. In addition, Cox-MSM is unable to incorporate multiple changes in treatment and only works under the assumption that the same treatment is continuing [8]. In other words, even if multiple subsequent therapies were given to the patient, only the first subsequent therapy was accounted for in our analyses, which is another limitation of our study.
5 Conclusions
No difference was observed between the treatment effects of chemotherapy and non-chemotherapy after AAP in patients with high-risk mCSPC. These findings suggest that choosing any life-extending subsequent therapy will contribute to improving clinical outcomes in patients treated with AAP for mCSPC who have progressed to mCRPC. Physicians should choose the most appropriate treatment for these patients based on the patient’s condition and preferences.
References
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N Engl J Med. 2017;377:352–60. https://doi.org/10.1056/NEJMoa1704174.
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone acetate plus prednisone in patients with newly diagnosed high-risk metastatic castration-sensitive prostate cancer (LATITUDE): final overall survival analysis of a randomised, double-blind, phase 3 trial. Lancet Oncol. 2019;20:686–700. https://doi.org/10.1016/S1470-2045(19)30082-8.
Koroki Y, Taguri M, Matsubara N, Fizazi K. Estimation of overall survival with subsequent treatment effect by applying inverse probability of censoring weighting in the LATITUDE study. Eur Urol Open Sci. 2022;36:51–8. https://doi.org/10.1016/j.euros.2021.11.012.
James ND, Clarke NW, Cook A, Ali A, Hoyle AP, Attard G, et al. STAMPEDE Trials Collaborative Group. Abiraterone acetate plus prednisolone for metastatic patients starting hormone therapy: 5-year follow-up results from the STAMPEDE randomised trial (NCT00268476). Int J Cancer. 2022;151:422–34. https://doi.org/10.1002/ijc.34018.
Fizazi K, Foulon S, Carles J, Roubaud G, McDermott R, Fléchon A, et al. PEACE-1 Investigators. Abiraterone plus prednisone added to androgen deprivation therapy and docetaxel in de novo metastatic castration-sensitive prostate cancer (PEACE-1): a multicentre, open-label, randomised, phase 3 study with a 2 × 2 factorial design. Lancet. 2022;399:1695–707. https://doi.org/10.1016/S0140-6736(22)00367-1.
Khalaf DJ, Annala M, Taavitsainen S, Finch DL, Oja C, Vergidis J, et al. Optimal sequencing of enzalutamide and abiraterone acetate plus prednisone in metastatic castration-resistant prostate cancer: a multicentre, randomised, open-label, phase 2, crossover trial. Lancet Oncol. 2019;20:1730–9. https://doi.org/10.1016/S1470-2045(19)30688-6.
de Bono JS, Smith MR, Saad F, Rathkopf DE, Mulders PFA, Small EJ, et al. Subsequent chemotherapy and treatment patterns after abiraterone acetate in patients with metastatic castration-resistant prostate cancer: post hoc analysis of COU-AA-302. Eur Urol. 2017;71:656–64. https://doi.org/10.1016/j.eururo.2016.06.033.
Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11:561–70. https://doi.org/10.1097/00001648-200009000-00012.
Westreich D, Cole SR, Tien PC, Chmiel JS, Kingsley L, Funk MJ, et al. Time scale and adjusted survival curves for marginal structural Cox models. Am J Epidemiol. 2010;171:691–700. https://doi.org/10.1093/aje/kwp418.
Heinzl H, Kaider A. Gaining more flexibility in Cox proportional hazards regression models with cubic spline functions. Comput Methods Programs Biomed. 1997;54:201–8. https://doi.org/10.1016/s0169-2607(97)00043-6.
Hagiwara Y, Shinozaki T, Mukai H, Matsuyama Y. Sensitivity analysis for subsequent treatments in confirmatory oncology clinical trials: a two-stage stochastic dynamic treatment regime approach. Biometrics. 2021;77:702–14. https://doi.org/10.1111/biom.13296.
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12. https://doi.org/10.1056/NEJMoa040720.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33. https://doi.org/10.1056/NEJMoa1405095.
Cornford P, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer. Part II-2020 update: treatment of relapsing and metastatic prostate cancer. Eur Urol. 2021;79:263–82. https://doi.org/10.1016/j.eururo.2020.09.046.
Parker C, Castro E, Fizazi K, Heidenreich A, Ost P, Procopio G, et al. Prostate cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:1119–34. https://doi.org/10.1016/j.annonc.2020.06.011.
Chen EJ, Sowalsky AG, Gao S, Cai C, Voznesensky O, Schaefer R, et al. Abiraterone treatment in castration–resistant prostate cancer selects for progesterone responsive mutant androgen receptors. Clin Cancer Res. 2015;21:1273–80. https://doi.org/10.1158/1078-0432.CCR-14-1220.
Prekovic S, van Royen ME, Voet AR, Geverts B, Houtman R, Melchers D, et al. The effect of F877L and T878A mutations on androgen receptor response to enzalutamide. Mol Cancer Ther. 2016;15:1702–12. https://doi.org/10.1158/1535-7163.MCT-15-0892.
Conteduca V, Wetterskog D, Sharabiani MTA, Grande E, Fernandez-Perez MP, Jayaram A, et al. Androgen receptor gene status in plasma DNA associates with worse outcome on enzalutamide or abiraterone for castration-resistant prostate cancer: a multi-institution correlative biomarker study. Ann Oncol. 2017;28:1508–16. https://doi.org/10.1093/annonc/mdx155.
Conteduca V, Jayaram A, Romero-Laorden N, Wetterskog D, Salvi S, Gurioli G, et al. Plasma androgen receptor and docetaxel for metastatic castration-resistant prostate cancer. Eur Urol. 2019;75:368–73. https://doi.org/10.1016/j.eururo.2018.09.049.
Shiba K, Kawahara T. Using propensity scores for causal inference: pitfalls and tips. J Epidemiol. 2021;31:457–63. https://doi.org/10.2188/jea.JE20210145.
Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550–60. https://doi.org/10.1097/00001648-200009000-00011.
Acknowledgements
We express our gratitude to Karim Fizazi, M.D., Ph.D. (Department of Cancer Medicine, Institut Gustave Roussy, University of Paris Saclay, Villejuif, France) for his work as a contributor; he is a primary investigator of the LATITUDE study, and provided critical advice on data interpretation. We also thank the study participants and their families as well as the investigators, study coordinators, study teams, and nurses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The LATITUDE study was funded by Janssen Research & Development. Editorial support of this study was funded by Janssen Pharmaceutical K.K.
Conflicts of interest/competing interests
YK is an employee of Janssen Pharmaceutical K.K. and holds stock in Johnson & Johnson. MT has nothing to disclose.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the local institutional review boards for each site and conformed with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent, including permission for patient data to be used in post hoc analyses such as the present study, was obtained from all individual participants included in the LATITUDE study (ClinicalTrials.gov, NCT01715285).
Consent for publication
Patients signed informed consent regarding publishing their data.
Code availability
The code used during the current study is available from the corresponding author on reasonable request.
Availability of data and material
The data sharing policy of the study sponsor, Janssen Pharmaceutical Companies of Johnson & Johnson, is available online. Requests for access to the study data can be submitted through the Yale Open Data Access Project site. For Janssen’s data sharing policy, see https://www.janssen.com/clinical-trials/transparency. For the Yale Open Data Access Project, see http://yoda.yale.edu.
Author contributions
YK and MT contributed to the study’s conception and design. Material preparation and analysis were performed by YK. The first draft of the manuscript was written by YK, and all authors commented on previous versions of the manuscript. All authors have read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Koroki, Y., Taguri, M. Clinical Outcomes of First Subsequent Therapies After Abiraterone Acetate Plus Prednisone for High-Risk Metastatic Castration-Sensitive Prostate Cancer in the LATITUDE Study. Targ Oncol 18, 119–128 (2023). https://doi.org/10.1007/s11523-022-00929-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-022-00929-3