Abstract
Background
Vascular endothelial growth factor receptor (VEGFR) tyrosine kinase inhibitors (TKIs) are an essential therapeutic option in the management of various solid tumors, particularly renal cell carcinoma (RCC). However, post-marketing data regarding their potential cardiovascular toxicities are scant.
Objective
To identify and characterize cardiovascular adverse events (CVAEs) of VEGFR-TKIs indicated for RCC.
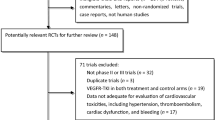
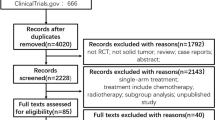
Patients and Methods
Disproportionality analysis of the US Food and Drug Administration adverse event reporting system (July 2014–December 2019) using the reporting odds ratio (ROR) and the lower bound of the Information component (IC) 95% credibility interval (IC025 > 0 is significant).
Results
We identified 51,836 adverse event reports of sunitinib, pazopanib, axitinib, cabozantinib, and lenvatinib in the full database [36% women; median age 65 years (range 57–73)]. CVAEs accounted for 11,784 (23%) of the reports, with hypertension [n = 5548 (11%), ROR = 6.55 (95% CI 6.37–6.74), IC025 = 2.48] and hemorrhages [n = 3710 (7.2%), ROR = 1.28 (1.24–1.32), IC025 = 0.28] being the most frequent types. Additional CVAEs were over-reported with VEGFR-TKIs treatment, including aortic dissection [n = 61 (0.1%), ROR = 3.50 (2.71–4.51)], pericardial diseases [n = 173 (0.3%), ROR = 1.98 (1.70–2.30)], cardiomyopathy [n = 61 (0.1%), ROR = 1.89 (1.47–2.43)], heart failure [n = 868 (1.7%), ROR = 1.35 (1.26–1.44)], and venous thromboembolism [n = 604 (1.2%), ROR = 1.33 (1.23–1.45), all IC025 > 0]. The major pericardial disorder was non-malignant pericardial effusion [n = 134 (77%)]. Aortic dissections were also over-reported in patients without concomitant elevated blood pressure [ROR = 2.68 (1.97–3.63), IC025 = 0.91]. Finally, CVAEs were reported more often following lenvatinib and sunitinib treatment compared to other VEGFR-TKIs.
Conclusions
In post-marketing surveillance data, VEGFR-TKIs are associated with increased reporting of various CVAEs, including pericardial diseases, particularly non-malignant pericardial effusion, and aortic dissections. Moreover, VEGFR-TKIs differ in their CVAE reporting patterns. Clinicians should be conscious of these findings in the care of VEGFR-TKIs recipients.
Graphic Abstract
Cardiovascular toxicities of VEGFR-TKIs in the FDA adverse events reporting system (FAERS) database. Post-marketing data of vascular endothelial growth factor receptor (VEGFR) tyrosine kinase inhibitor (TKI)-associated cardiovascular toxicities are scant. We identified 51,836 safety reports of VEGFR-TKIs (sunitinib, pazopanib, axitinib, cabozantinib, and lenvatinib) in the FAERS database, including 11,784 (23%) cardiovascular adverse events (CVAEs). Hypertension, aortic dissections, and pericardial diseases had the highest reporting odds ratios. While the association of VEGFR-TKIs with hypertension is well established, pericardial diseases were not observed to date, and aortic dissection was reported in a small case series.




Similar content being viewed by others
References
Levitzki A. Tyrosine kinase inhibitors: views of selectivity, sensitivity, and clinical performance. Annu Rev Pharmacol Toxicol. 2013;53:161–85.
Heldin CH, Westermark B. Mechanism of action and in vivo role of platelet-derived growth factor. Physiol Rev. 1999;79:1283–316.
Ferrara N, Adamis AP. Ten years of anti-vascular endothelial growth factor therapy. Nat Rev Drug Discov. 2016;15:385–403.
Moslehi JJ. Cardiovascular toxic effects of targeted cancer therapies. N Engl J Med. 2016;375:1457–67.
Li W, Croce K, Steensma DP, McDermott DF, Ben-Yehuda O, Moslehi J. Vascular and metabolic implications of novel targeted cancer therapies: focus on kinase inhibitors. J Am Coll Cardiol. 2015;66:1160–78.
Herrmann J. Adverse cardiac effects of cancer therapies: cardiotoxicity and arrhythmia. Nat Rev Cardiol. 2020;17(8):474–502.
Totzeck M, Mincu RI, Mrotzek S, Schadendorf D, Rassaf T. Cardiovascular diseases in patients receiving small molecules with anti-vascular endothelial growth factor activity: a meta-analysis of approximately 29,000 cancer patients. Eur J Prev Cardiol. 2018;25:482–94.
Byrne AM, Bouchier-Hayes DJ, Harmey JH. Angiogenic and cell survival functions of Vascular Endothelial Growth Factor (VEGF). J Cell Mol Med. 2005;9:777–94.
Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C, Hutson TE, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet. 2011;378:1931–9.
Hall PS, Harshman LC, Srinivas S, Witteles RM. The frequency and severity of cardiovascular toxicity from targeted therapy in advanced renal cell carcinoma patients. JACC Hear Fail. 2013;1:72–8.
Sonpavde G, Je Y, Schutz F, Galsky MD, Paluri R, Rosenberg JE, et al. Venous thromboembolic events with vascular endothelial growth factor receptor tyrosine kinase inhibitors: a systematic review and meta-analysis of randomized clinical trials. Crit Rev Oncol Hematol. 2013;87:80–9.
Raschi E, Gatti M, Gelsomino F, Ardizzoni A, Poluzzi E, De Ponti F. Lessons to be learnt from real-world studies on immune-related adverse events with checkpoint inhibitors: a clinical perspective from pharmacovigilance. Target Oncol. 2020;15:449–66.
Salem JE, Manouchehri A, Bretagne M, Lebrun-Vignes B, Groarke JD, Johnson DB, et al. Cardiovascular toxicities associated with ibrutinib. J Am Coll Cardiol. 2019;74:1667–78.
Huang J, Meng L, Yang B, Sun S, Luo Z, Chen H. Safety profile of epidermal growth factor receptor tyrosine kinase inhibitors: a disproportionality analysis of FDA adverse event reporting system. Sci Rep. 2020;10(1):4803.
Powles T, Albiges L, Staehler M, Bensalah K, Dabestani S, Giles RH, et al. Updated European Association of Urology Guidelines: recommendations for the treatment of first-line metastatic clear cell renal cancer. Eur Urol. 2018;73:311–5.
Angulo JC, Shapiro O. The changing therapeutic landscape of metastatic renal cancer. Cancers. 2019;11:1–13.
Raschi E, Poluzzi E, Salvo F, Pariente A, De Ponti F, Marchesini G, et al. Pharmacovigilance of sodium-glucose co-transporter-2 inhibitors: what a clinician should know on disproportionality analysis of spontaneous reporting systems. Nutr Metab Cardiovasc Dis. 2018;28:533–42.
Bate A, Evans SJW. Quantitative signal detection using spontaneous ADR reporting. Pharmacoepidemiol Drug Saf. 2009;18:427–36.
Harpaz R, Dumouchel W, Lependu P, Bauer-Mehren A, Ryan P, Shah NH. Performance of pharmacovigilance signal-detection algorithms for the FDA adverse event reporting system. Clin Pharmacol Ther. 2013;93:539–46.
Norén GN, Hopstadius J, Bate A. Shrinkage observed-to-expected ratios for robust and transparent large-scale pattern discovery. Stat Methods Med Res. 2013;22:57–69.
Harpaz R, Odgers D, Gaskin G, Dumouchel W, Winnenburg R, Bodenreider O, et al. A time-indexed reference standard of adverse drug reactions. Sci Data. 2014;1:140043.
Salem JE, Manouchehri A, Moey M, Lebrun-Vignes B, Bastarache L, Pariente A, et al. Cardiovascular toxicities associated with immune checkpoint inhibitors: an observational, retrospective, pharmacovigilance study. Lancet Oncol. 2018;19:1579–89.
Herrmann J. Vascular toxic effects of cancer therapies. Nat Rev Cardiol. 2020;17(8):503–22.
Abdel-Qadir H, Ethier JL, Lee DS, Thavendiranathan P, Amir E. Cardiovascular toxicity of angiogenesis inhibitors in treatment of malignancy: a systematic review and meta-analysis. Cancer Treat Rev. 2017;53:120–7.
Chu TF, Rupnick MA, Kerkela R, Dallabrida SM, Zurakowski D, Nguyen L, et al. Cardiotoxicity associated with tyrosine kinase inhibitor sunitinib. Lancet. 2007;370:2011–9.
Hatem R, Bebawi E, Schampaert E. Potential sunitinib-induced coronary artery and aortic dissections. Can J Cardiol. 2017;33:830.e17-830.e18.
Edeline J, Laguerre B, Rolland Y, Patard JJ. Aortic dissection in a patient treated by sunitinib for metastatic renal cell carcinoma. Ann Oncol. 2009;21:186–7.
Niwa N, Nishiyama T, Ozu C, Yagi Y, Saito S. Acute aortic dissection in a patient with metastatic renal cell carcinoma treated with axitinib. Acta Oncol. 2015;54:567–8.
Oshima Y, Tanimoto T, Yuji K, Tojo A. Association between aortic dissection and systemic exposure of vascular endothelial growth factor pathway inhibitors in the Japanese Adverse Drug Event Report database. Circulation. 2017;135:815–7.
Kust D, Kruljac I, Peternac AŠ, Ostojić J, Prpić M, Čaržavec D, et al. Pleural and pericardial effusions combined with ascites in a patient with severe sunitinib-induced hypothyroidism. Acta Clin Belg. 2016;71(3):175–7.
Krauth MT, Herndlhofer S, Schmook MT, Mitterbauer-Hohendanner G, Schlögl E, Valent P. Extensive pleural and pericardial effusion in chronic myeloid leukemia during treatment with dasatinib at 100 mg or 50 mg daily. Haematologica. 2011;96:163–6.
Kelly K, Swords R, Mahalingam D, Padmanabhan S, Giles FJ. Serosal inflammation (pleural and pericardial effusions) related to tyrosine kinase inhibitors. Target Oncol. 2009;4:99–105.
Quintás-Cardama A, Kantarjian H, O’Brien S, Borthakur G, Bruzzi J, Munden R, et al. Pleural effusion in patients with chronic myelogenous leukemia treated with dasatinib after imatinib failure. J Clin Oncol. 2007;25:3908–14.
Fogli S, Porta C, Del Re M, Crucitta S, Gianfilippo G, Danesi R, et al. Optimizing treatment of renal cell carcinoma with VEGFR-TKIs: a comparison of clinical pharmacology and drug-drug interactions of anti-angiogenic drugs. Cancer Treat Rev. 2020;84:101966.
Aragon-Ching JB, Ning YM, Dahut WL. Acute aortic dissection in a hypertensive patient with prostate cancer undergoing chemotherapy containing bevacizumab. Acta Oncol. 2008;47:1600–1.
Hahn NM, Stadler WM, Zon RT, Waterhouse D, Picus J, Nattam S, et al. Phase II trial of cisplatin, gemcitabine, and bevacizumab as first-line therapy for metastatic urothelial carcinoma: Hoosier oncology group GU 04–75. J Clin Oncol. 2011;29:1525–30.
Pucci G, Milan A, Paini A, Salvetti M, Cerasari A, Vaudo G. Acute blood pressure elevation associated with biological therapies for cancer: a focus on VEGF signaling pathway inhibitors. Expert Opin Biol Ther. 2019;19:433–42.
Shamloo BK, Chhabra P, Freedman AN, Potosky A, Malin J, Smith SW. Novel adverse events of bevacizumab in the US FDA adverse event reporting system database: a disproportionality analysis. Drug Saf. 2012;35:507–18.
Bonnet C, Sibon I. Potential role of anti-VEGF targeted therapies in cervical artery dissection: a case report. Rev Neurol. 2015;171:677–9.
Molina AM, Feldman DR, Voss MH, Ginsberg MS, Baum MS, Brocks DR, et al. Phase 1 trial of everolimus plus sunitinib in patients with metastatic renal cell carcinoma. Cancer. 2012;118:1868–76.
Schlumberger M, Tahara M, Wirth LJ, Robinson B, Brose MS, Elisei R, et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med. 2015;7:621–51.
Mahé J, de Campaigno EP, Chené A-L, Montastruc J-L, Despas F, Jolliet P. Pleural adverse drugs reactions and protein kinase inhibitors: identification of suspicious targets by disproportionality analysis from VigiBase. Br J Clin Pharmacol. 2018;84:2373–83.
Patras de Campaigno E, Bondon-Guitton E, Laurent G, Montastruc F, Montastruc J-L, Lapeyre-Mestre M, et al. Identification of cellular targets involved in cardiac failure caused by PKI in oncology: an approach combining pharmacovigilance and pharmacodynamics. Br J Clin Pharmacol. 2017;83:1544–55.
Hazell L, Shakir SAW. Under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2006;29:385–96.
Bégaud B, Martin K, Haramburu F, Moore N. Rates of spontaneous reporting of adverse drug reactions in France. J Am Med Assoc. 2002;288:1588.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this article.
Conflict of interest
AG, DB, RD, DF, BB, MA, and EM declare that they have no conflicts of interest that might be relevant to the contents of this article.
Availability of data and material
The FAERS is a publicly available and anonymized database.
Author contributions
A.G. and D.B. conceived the idea. All authors contributed to the design of the study. A.G. and D.B. acquired the data for the study and performed the analyses. E.M. supervised the study. A.G. wrote the manuscript. All authors interpreted the results and made manuscript revisions. All authors have read and agreed to the published version of the manuscript.
Ethics approval
Since the FAERS is a publicly available and anonymized database, Institutional review board approval and informed consent were waived.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Goldman, A., Bomze, D., Dankner, R. et al. Cardiovascular Toxicities of Antiangiogenic Tyrosine Kinase Inhibitors: A Retrospective, Pharmacovigilance Study. Targ Oncol 16, 471–483 (2021). https://doi.org/10.1007/s11523-021-00817-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-021-00817-2