Abstract
Different care networks in Spain evaluate the co-occurrence of substance use disorders (SUD) and other mental disorders (OMDs). This study aimed to explore the differences in prevalence, sociodemographic and clinical profile, pharmacological treatment, and gender perspective of the co-occurrence of SUD and OMD between specific addiction treatment networks and mental health networks. This is an observational, cross-multicenter study with a randomized sample of patients under treatment for SUD or OMDs in different autonomous communities of Spain (N = 1783). Sixty-seven health professionals completed an ad hoc online questionnaire, collecting sociodemographic variables with patients diagnosed with SUD and OMDs, and their pharmacological treatments. The findings revealed a high prevalence of OMD in patients treated for SUD (71%) and those for OMD diagnosed with SUD (59%). Specific relationships between the SUDs and OMDs were identified. In networks treating SUDs, the increase in treatment for OMDs was widespread. However, the addition of SUD treatments in mental health networks was less frequent than expected. In addition, an elevated benzodiazepine prescription was detected in both settings. Some possible gender biases in treatments were found. This study provides preliminary information on the coexistence in routine clinical practice of addictive disorders and other mental disorders in Spain. The results revealed that the treatments provided are inefficient for SUDs in patients treated in mental health settings. Furthermore, a high prescription of anxiolytics and differences by sex are shown. These findings may contribute to adapting the treatment response with greater precision and effectiveness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A high prevalence of comorbidity occurs between substance use disorder (SUD) and other mental disorders (OMD) (Hunt et al., 2018; Pascual-Pastor, Fernández-Miranda, Díaz-Fernández, & Sala-Añó, 2017). Among the general population, the odds ratio of substance users suffering from a psychiatric condition is higher, at around 3 or 4, than among the non-using population (Hasin & Grant, 2015; Pascual-Pastor et al., 2017; Torrens et al., 2015). More than a third of people diagnosed with a mental disorder abuse are addicted to psychoactive substances, especially alcohol (Arias et al., 2013b; Hasin & Grant, 2015; Hunt et al., 2018; Pascual-Pastor et al., 2017; Torrens et al., 2015). The prevalence is higher in the population undergoing treatment compared to the general population (Torrens et al., 2015). This comorbidity is essential due to its clinical and social severity, the difficulties in tackling it, and its association with worse treatment results for those affected (Daigre et al., 2017; Hasin & Grant, 2015; Pascual-Pastor et al., 2017; Priester et al., 2016; Spivak et al., 2020; Torrens et al., 2015).
Although the co-occurrence of substance use disorders and other mental disorders is high in Spain, the details are uncertain (Arias et al., 2013b; Gual, 2007; Roncero et al., 2001). In 2007, Gual showed that 33.8% of addicts in Spain presented a dual pathology, mainly alcoholics abusing other drugs (48.5%), with depression being the most prevalent disorder (Gual, 2007). The main problem is that the treatment of these patients is managed by various health networks and units, which causes significant variability (Arias Horcajadas et al., 2020; Fernandez Miranda et al., 2001; Torrens et al., 2012). Since the 1980s, there have been two networks in Spain to treat a single patient with an addictive disorder and other mental disorders. As a result, the comorbidity is handled in parallel or sequential care, leading to deficits that increase morbidity and mortality and the abandonment of treatment (Pascual-Pastor et al., 2017; Roncero et al., 2001) as in other countries (Mangrum et al., 2006; Mueser et al., 2003; Priester et al., 2016; Torrens et al., 2015). There are differences regarding sociodemographic and clinical characteristics of this comorbidity depending on the populations in which the studies are made (Arias et al., 2013a, 2013b; Calvo et al., Carbonell, 2021; Hasin & Grant, 2015; Hunt et al., 2018; Palomo et al., 2017; Priester et al., 2016; Torrens et al., 2015).
From the end of the 1990s, several studies have been published on the co-occurrence of SUDs and OMDs in treatment populations, with the majority of them developed in specific care units for drug addiction and in autonomous communities with different care models (parallel or integrated) (Arias et al., 2013b; Fernandez Miranda et al., 2001; Roncero et al., 2001). Several studies in Madrid analyzed different sociodemographic data in patients with SUD and OMD served in various care networks (Arias et al., 2013a, 2013b; Palomo et al., 2017). The study by Arias et al., (2013a, 2013b) showed that of 61.8% of patients with dual pathology, 36.1% are managed in the mental health network and 70.3% in the drug network (Arias et al., 2013b). It has also been reported that patients with dual pathology, especially those consuming alcohol and cocaine, present a higher risk of suicide (Arias et al., 2013b). In addition, 73.4% of cocaine addicts had a dual diagnosis highlighting the prevalence of mood, anxiety and personality disorders (Arias et al., 2013a; Palomo et al., 2017). Another study carried out in Huelva showed that there is a higher prevalence of patients with psychotic disorders in the mental health units (66%) and with a higher cannabis dependence compared to the addiction center (37.5%) (Mancheño-Barba et al., 2019). However, it is essential to point out that most studies have analyzed samples exclusively of patients treated in psychiatric-mental centers or drug addiction centers. To date, no studies have been carried out at the national level in Spain comparing the similarities and differences between dual patients in the mental health system versus the addictive disorders network and the type of treatment they receive in each of them.
On the other hand, the proper use of medication is an essential element in treating patients with comorbidity since it significantly affects the stabilization of both psychiatric and addictive symptoms, thereby helping to increase the effectiveness of other treatments, such as psychosocial (Arias Horcajadas et al., 2020; Iqbal et al., 2019; Substance Abuse and Mental Health Services Administration, 2006).
In recent years, specific pharmacological measures have been established concerning the specific comorbidity of SUD and other mental disorders such as psychotic (Azorin et al., 2016; Crockford & Addington, 2017; Werner & Covenas, 2017), affective (Hillemacher & Frieling, 2019; Maremmani et al., 2013; Salloum & Brown, 2017; Tirado Muñoz, Farre, Mestre-Pinto, Szerman, & Torrens, 2018), and anxiety disorders (Saiz Martinez et al., 2014; Smith & Randall, 2012). Similar measures also exist to study the specific substance causing the disease together with other comorbid mental disorders, whether legal, such as alcohol and anxiolytics (Florez-Menendez et al., 2018; Hillemacher & Frieling, 2019; Sanchez-Peña et al., 2012; Vitali et al., 2018) or illicit, such as cocaine (Alvarez et al., 2013; Ochoa-Mangado et al., 2018), cannabis (Arias et al., 2017; Cuenca-Royo et al., 2013) or opiates (Fernández-Miranda at al., 2019; Maremmani et al., 2013).
Women suffer from psychiatric comorbidity more frequently than men, mainly depression and PTSD, and treatment response is also different for women and men. For instance, women present a greater risk for relapse and face more barriers to accessing services if they have addictive disorders, including higher stigma. No apparent differences have been described in pharmacological treatment response (Fonseca et al., 2021; Tirado-Munoz et al., 2018).
This study intends to establish differences between samples of mental health and specific addiction networks in sociodemographic and clinical profiles, SUD and OMD diagnoses, and prescribed psychotropic drugs for treating both disorders, adding the component of gender and comparing populations cared for in mental health or addiction settings. Since the aim is to provide an overall picture of each of these treatment networks, the design tries to ensure that the sample’s composition reaches the highest representativeness of the universe from which it is drawn.
Method
This was an observational, cross-sectional, multicenter study with a randomized sample of patients undergoing treatment for addictive disorders or other mental disorders throughout Spain (N = 1783). Sixty-seven health professionals completed a questionnaire designed by the study authors on substance use and their patients’ diagnoses and treatments in specific addiction and mental health treatment networks. These networks include outpatient addiction treatment programs, mental health or addiction hospitals/day centers, mental health units/centers, and prisons, guaranteeing the highest confidentiality and anonymity levels. Of a total of 1783 patients, 322 were from mental health resources (180 in mental health centers and 42 subjects in mental health day centers) and 1461 were from addictive disorder care resources (32 in prison, 570 in ambulatory addiction centers, and 859 subjects from addiction treatment day centers).
A survey was hosted on a website (www.socidrogalcohol.org) with the variables to be collected, which could be accessed by professionals (physicians, mainly psychiatrists but also general practitioners with specific training in addiction and its comorbidities, and clinical psychologists) to fill in the data for each patient, always complying with the maximum guarantees of confidentiality and anonymity. The patients were anonymized from the beginning. The variables studied were sociodemographic (age, sex/gender, employment status, living arrangements), related to somatic pathologies (HBV, HCV, HIV), substance use disorders, other mental disorders, and medications prescribed both for the SUD (opioid agonists/opioid antagonists/interdictors) and for the OMD (antipsychotics/mood stabilizers/antidepressants), and anxiolytics. Differences between males/females were searched.
Except for 32 subjects in prison (considered in the SUD group), all studied were outpatients in mental health or addiction treatment networks, both receiving pharmacological and psychological facilities. The study population consisted of people receiving treatment (at least for a year) in mental health or addiction care networks in Spain, over 18 years of age, with a diagnosis of substance use disorder or another mental disorder at the time of the survey, and with a pharmacological prescription.
The diagnoses were performed following the ICD-10 or DSM-5 criteria and were already in their medical records or were made by the professionals treating them and participating in the study. Diagnosis not due to substance use (not substance-induced) was performed following the standard of a “window period” of at least 4 weeks. Diagnoses were consistent and reliable when the subjects studied were in treatment for at least a year.
All the variables, including diagnoses, were collected from medical records by treating professionals: physicians (mainly psychiatrists but also general practitioners with specific training in addiction and its comorbidities) and clinical psychologists.
A non-probabilistic, convenient, and consecutive sampling was designed. Randomization was performed by surveying the patients attending the professional’s consultation on the same day of the week for 4 weeks. Data was collected in fifteen of Spain’s seventeen Autonomous Communities (regions).
Descriptive and inferential statistics were performed. Pearson’s chi-square (bilateral asymptotic significance) was used for inferential statistics, and Fisher’s exact test (exact bilateral significance) for qualitative and dichotomized quantitative variables. The confidence interval was set at 95%. The SPSS program (version v. 23) was used for data processing.
This research received an external methodological and ethical evaluation by the National Plan on Addiction (Spanish Ministry of Health). The study was carried out following the ethical principles of the Declaration of Helsinki. Patients gave consent for their data to be collected by their health professionals and were informed that they were anonymized. The study was performed by interviewing professionals about patients and not the patients themselves, always maintaining their anonymity. Furthermore, it is a retrospective study since the treatments were already in place.
Results
A total of 1783 surveys were correctly completed out of the 2,000 planned in fifteen autonomous communities. Of these, 322 were from mental health network resources and the rest from addictive disorder care resources.
The results showed a significant concurrence of SUD and OMD diagnoses (in more than 60% of the patients). A high prevalence of OMD was found in patients receiving treatment for their SUD (71%) and also diagnosed with any SUD (68.9%) and active substance use (50%, except tobacco) in people receiving treatment for diagnoses of OMD. Significant relationships were also found between addiction to certain substances and specific mental disorders (personality disorders with all SUDs, psychotic disorders with cannabis use disorder but not cocaine use disorder, affective disorders with cocaine use disorder, and anxiety disorders with cannabis use disorder).
Sociodemographic and Clinical Profile
The addiction network includes more men and more young people. Patients undergoing treatment in the addiction network often had more jobs and previous treatments and were more frequently diagnosed with infectious diseases (HIV, HCV). Alcohol use was linked to HBV and the presence of neurological disease, opioids and cannabis to hepatitis C, B and HIV, tobacco to hepatitis C and neurological disorders, cocaine to HCV, and the use of anxiolytics with HCV and HIV.
The sociodemographic and clinical somatic characteristics are summarized in Table 1.
Substance Use Disorder Diagnoses
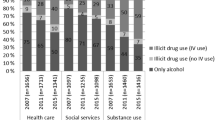
In the mental health network, 68.9% of patients present a current diagnosis of SUD, lower than in the addictions network. The use disorders (UD) of alcohol, tobacco, cocaine, and cannabis stand out in the total. In the addiction network, alcohol, tobacco, and cocaine UDs were the most common, while in the mental health network, these were tobacco, alcohol, and cannabis UDs (Fig. 1). The SUDs in the mental health and addictions networks are shown in Table 2. Furthermore, and not specified in Table 2, there was a significant co-occurrence of several current diagnoses for substance use, the most frequent being those tobacco and alcohol UDs (10.6%) and cocaine and alcohol UDs (5.3%).
Diagnoses of Other Mental Disorders
The diagnoses of mental disorders not due to substance use (not F10–19, ICD-10) in both treatment networks are summarized in Table 3. The most common diagnoses in the mental health network were psychotic and affective disorders. A significant difference in diagnosis between both networks was found regarding psychotic disorders (Fig. 2). There was a high prevalence of comorbid diagnoses in the addiction network, especially affective and personality disorders. Furthermore, and not specified in Table 3, comorbidity also exists between several diseases in one patient (in 23.7% of them), mainly between personality disorder (PD) and other mental disorders (in 16.6% of subjects).
Relationships Between SUDs and Other Mental Disorders
The relationships between the different SUDs and other mental disorder diagnoses, grouped by significant syndromes, are shown in Table 4.
The relationships found between the UD of specific substances and the different most relevant specific mental disorders were as follows: alcohol UD with the affective disorder, opioid UD with personality disorder, cannabinoid UD with psychotic disorder, TP and anxiety disorder, UD sedatives with personality disorder, anxiety disorder and sleep disorder, cocaine UD with affective disorder and personality disorder, not related to psychotic disorders, stimulant UD (amphetamines) with psychotic illness and personality disorder, and tobacco UD with psychotic disorder and personality disorder.
Concerning non-SUD mental disorders, the most significant relationships were psychotic disorders with cannabis, other stimulants and tobacco UDs, and to a lesser extent with alcohol UD, affective disorder especially with cocaine UD and less with alcohol UD, anxiety disorder with cannabis UD and less significantly with sedative UD. Personality disorders are related to all UDs, especially opioid UD, cannabis UD, sedative UD, cocaine UD, and tobacco UD.
Prescribed Treatments
The pharmacological treatments prescribed by the two care networks are summarized in Table 5.
The most relevant results concerning the addiction treatments revealed that interdictors were relatively little used in both networks and opiate antagonists were hardly ever used in either healthcare network. The use of opiate agonists to treat opioid dependence occurred almost exclusively in the addiction network; strikingly, a low percentage of patients was treated for SUDs in the mental health network, despite their high prevalence. On the other hand, in the treatment of OMDs, psychotropic drugs were used similarly for their treatment in both networks, with considerable use of antipsychotics and frequent prescription of antidepressants and mood stabilizers in both. Finally, a very high percentage of patients were prescribed anxiolytics/hypnotics in both treatment networks.
Gender Differences
All subjects in the sample were identified as either male or female. The findings differentiated by gender are specified in Table 6. Differences in pharmacological prescriptions by gender are reflected in Table 7.
In our sample, women were less frequently diagnosed with alcohol, opioid, cannabis, and cocaine use disorders. However, other UDs were equal to men. In OMDs, they had fewer psychotic disorders and more affective, anxiety, sleep, and eating disorders, with the rest resulting the same, including personality disorders.
The results also revealed that women received more treatments with anxiolytics and antidepressants and similar antipsychotics, interdictors and mood stabilizers treatments than men. Moreover, they were treated proportionally with fewer agonists and more antagonists compared to men.
Discussion
Sociodemographic and Clinical Profile
In the addiction network, the sociodemographic characteristics of our sample did not differ significantly from what was already known in previous studies in Spain (Arias et al., 2013b; Fernandez Miranda et al., 2001; Pereiro et al., 2013; Roncero et al., 2001). The fact that the addiction network includes a significant number of young people is not striking since it reflects the well-known fact that the average age of patients in this network is lower than in the mental health network. According to the 2022 Spanish Addiction Observatory report, substance consumption occurs very early, starting at 14 years of age, and alcohol is the most consumed psychoactive substance (Brime et al., 2022). The same can be said of finding more men than women in the addiction network, which is not the case in the mental health network. Nevertheless, this does not coincide with the usual profile found in the addiction networks in previous studies (Arias et al., 2013b; Gual, 2007; Pereiro et al., 2013). It is possible that in our sample, women were less frequently diagnosed with alcohol, opioid, cannabis, and cocaine use disorders.
A higher prevalence of HCV and HIV infections was found in the addiction network. Hepatitis B and C, and HIV, were more common in men than in women and may reflect riskier behaviors on the part of men. In the case of hepatitis C and HIV, there was a relationship with heroin, prescription opioids and also with cannabis and anxiolytics. This could be explained by polydrug use (Arias et al., 2013a; Fernandez Miranda et al., 2001).
The most commonly used substances in both networks were alcohol, tobacco, cocaine, cannabis, and opioids, corresponding to what is known about the general population and the populations in treatment in Spain (Gual, 2007; Pascual-Pastor et al., 2017; Pereiro et al., 2013; Roncero et al., 2001). A relationship was also found between the UD of specific substances and the most relevant mental disorders.
SUD and OMD Diagnoses. Comorbidity
In the mental health network, 68.9% of patients presented a current SUD diagnosis (59% excluding tobacco). Of the total sample, the most prevalent substance use disorders were tobacco, alcohol, cannabis, and cocaine, which is similar to what is already known from previous research (Daigre et al., 2017; Gual, 2007; Hunt et al., 2018; Roncero et al., 2001).
Regarding diagnoses for other mental disorders, the essential finding is that 71% of patients in the addiction network were diagnosed with a mental disorder other than addiction, a very high prevalence. The frequent co-occurrence of affective (32.3%), personality (26.6%), anxiety (17.3%), and psychotic disorders (13.8%) is consistent with previous studies in Spain (Fernández-Miranda, 2002; Gual, 2007; Iqbal et al., 2019; Roncero et al., 2001).
It should be noted that, except for psychotic disorders, which were somewhat less frequent, the percentages of the different mental diseases treated were similar to those of the mental health network. Regarding the relationships between SUDs and OMDs, it can be highlighted that psychotic disorders were related to cannabis UD but not cocaine UD. It is also reasonable since there is an association between cannabis use and the development of psychosis (Ortiz-Medina et al., 2018). However, they were related to other stimulants, which is not in line with the previous findings (Arias et al., 2013b; Hunt et al., 2018). The relationship with tobacco UD is more common and, to a lesser extent, with alcohol (Arias et al., 2013b; Florez-Menendez et al., 2018; Pascual-Pastor et al., 2017). Affective disorders were significantly related to cocaine UD, which is common, especially in bipolar disorders (Arias et al., 2017), although it is less common that a weaker link to alcohol UD (Arias et al., 2013b; Florez-Menendez et al., 2018). The relationship between cannabis UD in anxiety disorders is less clearly explained (Cuenca-Royo et al., 2013; Saiz Martinez et al., 2014). It is also striking that the relationship was less significant with sedative UD, even though this disorder is conditioned and overlaps with the prescription of these drugs. It is not possible to clarify the extent to which there was abuse or dependence on them (Florez-Menendez et al., 2018; Guardia Serecigni & Flórez Menéndez, 2018; Pereiro et al., 2013; Saiz Martinez et al., 2014). It is interesting to find how personality disorders were significantly related to all SUDs, especially opioid UD (Fernández-Miranda, 2002; Fernández-Miranda et al., 2019), cannabis UD, sedative UD, cocaine UD (Pascual-Pastor et al., 2017; Pereiro et al., 2013), and tobacco UD, and to a lesser extent with alcohol UD and other stimulants UD (Arias et al., 2013b; Pereiro et al., 2013). The relationship between a PD and problematic drug use is confirmed in our study. Additionally, this use involved very different substances, although it was not possible to link a particular one to this disorder (Arias et al., 2013b; Fernández-Miranda, 2002; Gual, 2007).
Gender Perspective
Women had fewer diagnoses of all SUDs. The fact that women live in a higher percentage with their own family and less with a family of origin than men and that they are pensioners at a lower rate coincides with the profiles usually shown in both networks (Arias et al., 2013b; Gual, 2007; Pascual-Pastor et al., 2017). Hepatitis B, C, and HIV are more frequent in men than in women. This could be a consequence of their habitual risk behaviors, which has also been pointed out by different authors (Fernandez Miranda et al., 2001; Pereiro et al., 2013).
As for other mental disorders diagnosed at the time of the survey, women present fewer psychotic disorders and more affective, anxiety, sleep, and eating disorders, with the rest being the same, including personality disorders. The higher prevalence of affective and anxiety disorders in women is a common finding (Arias et al., 2013b; Fernández-Miranda, 2002; Pereiro et al., 2013). However, it is not expected that PDs are just as usual in men as in women since the balance of these disorders has always been tilted towards women (Florez-Menendez et al., 2018; Guardia Serecigni & Flórez Menéndez, 2018; Saiz Martinez et al., 2014).
Treatment of Co-occurring Diagnoses
Since the 1980s, there have been two networks in Spain to treat a single patient with an addictive disorder and other mental disorders. This approach has continued in many cases to the present day, with a very differentiated treatment network persisting in some autonomous communities for patients with addictions and with little coordination with the mental health network. As a result, the comorbidity is managed in parallel or sequential care, leading to deficits that increase morbidity and mortality and the abandonment of treatment (Pascual-Pastor et al., 2017; Roncero et al., 2001) as in other countries (Mangrum et al., 2006; Mueser et al., 2003; Priester et al., 2016; Torrens et al., 2015). It is important to emphasize not so much the effectiveness of individual interventions on each aspect or disorder occurring in the same patient but instead an integrated treatment as an approach strategy. This model was more effective than approaching each disease with separate treatment plans. (Arias Horcajadas et al., 2020; Donald et al., 2005; Drake et al., 1998; Mueser et al., 2003; Spivak et al., 2020; Torrens et al., 2012).
Several studies assessing pharmacological interventions were encouraging and could guide clinical practice (Arias Horcajadas et al., 2020; Iqbal et al., 2019; Murthy et al., 2019). Psychosocial interventions should take place as early as possible in the course of treatment. They should be highly intense and based on established SUD therapies (Arias Horcajadas et al., 2020; Hunt et al., 2019; Iqbal et al., 2019; Spivak et al., 2020; Tiet & Mausbach, 2007). The treatments used in patients with dual disorders are similar to those used when a single disease is present. Treatments for certain mental illnesses are also effective in dual-diagnosis patients. Therapies for substance use disorders are also suitable for addicted patients with psychiatric comorbidity (Alvarez et al., 2013; Crockford & Addington, 2017; Grau-Lopez et al., 2014; Saiz Martinez et al., 2014; Tirado Muñoz et al., 2018). No drugs are contraindicated (Arias Horcajadas et al., 2020; Azorin et al., 2016; Grau-Lopez et al., 2014; Iqbal et al., 2019; Murthy et al., 2019).
Treatments by Type of Care Network and Gender
Our study shows how in addition to addiction, treatments for OMDs are prevalent in addiction treatment networks, reflecting the critical awareness within them of psychiatric comorbidity and the need to treat this as soon as possible without the need for referral to another healthcare network. However, it is remarkable that, despite their high prevalence, the treatment of substance use disorders in patients receiving treatment in mental health networks is lower than expected. This could suggest the opposite of the addiction network: insufficient concern and attention to SUDs in patients initially treated for OMD.
A relevant issue is the high prescription of sedatives in both networks, despite the known risk of abuse and dependence (Guardia Serecigni & Flórez Menéndez, 2018; Saiz Martinez et al., 2014). The treatment and the duration of the prescription of these drugs in patients with dual diagnoses should be carried out by professionals, mainly when its indication is established. (Saiz Martinez et al., 2014; Smith & Randall, 2012).
The co-occurrence of OMDs is treated similarly in addictions and mental health networks. This indicates more awareness of the need to detect and treat comorbidity in the addiction network than in the mental health network (Arias et al., 2013b; Fernandez Miranda et al., 2001; Pascual-Pastor et al., 2017; Roncero et al., 2001).
In treating comorbidity, some studies show better results in attracting addicted women for treatment and higher adherence rates when differentiated treatments for women (Ashley et al., 2003; Coughey et al., 1998; Orwin et al., 2001). In our research, although the prevalence of opioid use disorder is significantly lower among women, they receive proportionally more treatment with antagonists than with agonists compared to men (4.7/11.5% vs. 2.7/20.4%), which may show a bias towards inclusion in programs that are less demanding for women. Women received more treatments with anxiolytics and antidepressants, in line with the use of these drugs and their prescription in the general population by gender. Interdictors, mood stabilizers, and antipsychotics were prescribed to the same extent as men, suggesting a lack of bias in prescribing these families of psychoactive drugs.
Strengths and Limitations of the Study
This research has been carried out in Spain with an objective national scope, involving almost all the autonomous communities and reflecting the diversity of healthcare networks. A descriptive approach and an inclusive definition of comorbidity were used. The sample is of significant size and was also subjected to randomization. However, the professionals’ approach is not randomized, and there is no certainty on the representativeness of the health professionals across the type of institutes. We are aware that there is a risk that only those professionals with a genuine interest in the topic preferentially responded.
In contrast, the sample is instead representative of the overall treatment centers and patients in Spain (including prisons). Furthermore, the scope is extensive. Given the above, it can be considered representative of many people with diagnoses of SUD and other concurrent mental disorders in routine treatment throughout Spain. Thus, the main strengths of this study are the size of the sample, the national scope, and the variety of treatment settings to avoid biases as far as possible, thereby ensuring an acceptable level of representativeness. Indeed, the origin of the participants seen in each treatment network is heterogeneous and could lead to biases, considering that different SUD and mental health facilities serve similar patients. An overrepresentation of subjects treated in a specific treatment center would misrepresent reality. However, the treatments are in both cases of the outpatient type, and there is a certain homogeneity in the services provided and their intensity and in the profile of the patient treated.
A possible limitation of this study is that the inclusion of cases was not carried out uniformly and could have resulted in bias in sample collection, especially given that patients treated in the mental health network are less represented than those with addictions. A bias in the patient sample may result not only from the low profile of the mental health network but also from the heterogeneity of the care structures in the different autonomous communities. Nevertheless, it reflects the reality of care for SUDs in Spain. A further possible limitation may be the randomization method chosen for its ease of application.
Additionally, instead of validated questionnaires, the one used was constructed ad hoc, easy to fill out, and collected the most relevant variables for the study’s objective. Another limitation could be that no screening or diagnostic instrument was implemented in the research to reduce diagnostic errors or variability. However, this allows reality to be reflected in the usual practice of using or not using diagnostic support tools.
Only pharmacological treatments were chosen for the study. This was due to methodological difficulties in registering the types of psychological treatments as they are not registered with the same precision as drugs. Moreover, the categories of pharmacotherapy can be potentially misleading (e.g., in many addictions and mental health centers, antipsychotics and antidepressants are used as sleep medication, not as a treatment for an additional psychiatric disorder).
Although alcohol interdictors and opioid antagonists are usually relatively time-limited prescription medications, the sample’s composition concerning the length of time each patient was on treatment at the point of evaluation is relatively homogeneous since the study population consisted of people receiving treatment at least for a year.
Finally, it should be pointed out that comparison with other studies is limited since there are hardly any studies of such a general nature in our setting. It is essential to point out that there are previous precedents where studies have been carried out at a national level in Spain with larger samples than the one presented here; however, there are several differences between them. The work presented here shows not only the comorbidity with psychiatric pathology in addiction centers but also in the network of mental disorders with addiction problems to some substances. In addition, it shows the different types of treatments that are given, differentiating them by gender in each of the care networks. To date, no studies have been carried out at the national level in Spain comparing the similarities and differences between dual patients in the mental health system versus the addictive disorders network and the type of treatment they receive in each of them.
Conclusions
Considering the characteristics of its design (implementation in different autonomous communities-regions and diversity of care settings and networks) and notwithstanding its limitations (especially the case selection method), this research can provide indicative, valuable, and updated preliminary information on the prevalence and treatment of SUD and OMD co-occurrence in both the mental health and the addiction networks throughout Spain. The design reveals that the sample composition reaches the highest representativeness to establish differences between samples of mental health and specific addiction networks in sociodemographic and clinical characteristics and prescribed psychotropic drugs for treating both disorders, adding the component of gender.
The results suggest a significant co-occurrence of diagnoses (in more than 60% of patients), low intervention in SUDs in mental health facilities, a high prescription of benzodiazepines in both networks, and certain biases related to gender. These findings should help adapt the treatment response with greater precision and effectiveness.
The study provides information on the genuine coexistence of addictive disorders and other mental disorders in Spain and on the treatment provided, reflecting the comorbidity in routine clinical practice conditions and the possible distortions in the drugs prescribed. It highlights the presence of other mental disorders in those patients in treatment for their addictive disorder. It reveals a very high prevalence of both diagnoses of SUD in those under treatment for diagnoses of other mental disorders in mental health facilities. It could also help to adapt treatment resources for people with addictive disorders and other psychiatric disorders.
Further research is needed to deepen our understanding of the problem and thus adapt the healthcare response to reality more efficiently. Adapting treatment resources for people with addictive disorders and other psychiatric disorder is a major challenge for the Spanish National Health System.
Data Availability
The data supporting this study may be available upon request from the corresponding author [J.M.].
References
Alvarez, Y., Perez-Mana, C., Torrens, M., & Farre, M. (2013). Antipsychotic drugs in cocaine dependence: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 45(1), 1–10. https://doi.org/10.1016/j.jsat.2012.12.013
Arias, F., Szerman, N., Vega, P., Mesias, B., Basurte, I., Morant, C., Babin, F. (2013a). Cocaine abuse or dependency and other psychiatric disorders. Madrid study on dual pathology. Revista de Psiquiatria y Salud Mental, 6(3), 121–128. https://doi.org/10.1016/j.rpsm.2012.09.002.
Arias, F., Szerman, N., Vega, P., Mesias, B., Basurte, I., Morant, C., & Babin, F. (2013). Madrid study on the prevalence and characteristics of outpatients with dual pathology in community mental health and substance misuse services. Adicciones, 25(2), 118–127.
Arias, F., Szerman, N., Vega, P., Mesias, B., Basurte, I., & Rentero, D. (2017). Bipolar disorder and substance use disorders. Madrid study on the prevalence of dual disorders/pathology. Adicciones, 29(3), 186–194. https://doi.org/10.20882/adicciones.782.
Arias Horcajadas, F., Cortés Tomás, M., Fernández Artamendi, S., Fernández Miranda, J. J., Flórez Menéndez, G., & Ochoa Mangado, E. (2020). Tuo + tm. Resumen de intervenciones vademecum & árboles de decisiones lógicas. Comorbilidad psiquiátrica en adicciones. Guías clínicas basadas en la evidencia científica. (Socidrogalcohol Ed.). Barcelona.
Ashley, O. S., Marsden, M. E., & Brady, T. M. (2003). Effectiveness of substance abuse treatment programming for women: A review. American Journal of Drug and Alcohol Abuse, 29(1), 19–53. https://doi.org/10.1081/ada-120018838
Azorin, J. M., Simon, N., Adida, M., & Belzeaux, R. (2016). Pharmacological treatment of schizophrenia with comorbid substance use disorder. Expert Opinion on Pharmacotherapy, 17(2), 231–253. https://doi.org/10.1517/14656566.2016.1114101
Brime, B., García, N., León, L., Llorens, N., Tristán, N., & Sánchez, E. (2022). Spanish Observatory on Drugs and Addictions. REPORT 2022 (M. d. Sanidad Ed.). Madrid.
Calvo, F., Rived-Ocana, M., Font-Mayolas, S., & Carbonell, X. (2021). Homelessness and mental health during the Great Recession (2008-2017): the effect of immigration. Revista Española de Salud Pública, 95(e1-15). Article e202106079.
Coughey, K., Feighan, K., Cheney, R., & Klein, G. (1998). Retention in an aftercare program for recovering women. Substance Use and Misuse, 33(4), 917–933. https://doi.org/10.3109/10826089809056249
Crockford, D., & Addington, D. (2017). Canadian schizophrenia guidelines: Schizophrenia and other psychotic disorders with coexisting substance use disorders. Canadian Journal of Psychiatry, 62(9), 624–634. https://doi.org/10.1177/0706743717720196
Cuenca-Royo, A. M., Torrens, M., Sanchez-Niubo, A., Suelves, J. M., & Domingo-Salvany, A. (2013). Psychiatric morbidity among young-adults cannabis users. Adicciones, 25(1), 45–53.
Daigre, C., Grau-Lopez, L., Rodriguez-Cintas, L., Ros-Cucurull, E., Sorribes-Puertas, M., Esculies, O., & Roncero, C. (2017). The role of dual diagnosis in health-related quality of life among treatment-seeking patients in Spain. Quality of Life Research, 26(12), 3201–3209. https://doi.org/10.1007/s11136-017-1668-4
Donald, M., Dower, J., & Kavanagh, D. (2005). Integrated versus non-integrated management and care for clients with co-occurring mental health and substance use disorders: A qualitative systematic review of randomised controlled trials. Social Science and Medicine, 60(6), 1371–1383. https://doi.org/10.1016/j.socscimed.2004.06.052
Drake, R. E., Mercer-McFadden, C., Mueser, K. T., McHugo, G. J., & Bond, G. R. (1998). Review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophrenia Bulletin, 24(4), 589–608. https://doi.org/10.1093/oxfordjournals.schbul.a033351
Fernández-Miranda, J. J. (2002). Trastornos de personalidad y adicción: Relaciones etiológicas y conscuencias terapeúticas. An Pediatría, 18, 6.
Fernández-Miranda, J. J., Orengo-Caus, T., & Díaz-Fernández, S. (2019). Comorbilidad psiquiátrica en adicciones. Trastorno por uso de opioides y otro trastorno mental comórbido. Guías clínicas basadas en la evidencia. Valencia. (Socidrogalcohol Ed.).
Fernandez Miranda, J., Gonzalez Garcia-Portilla, M., Saiz Martinez, P., Gutierrez Cienfuegos, E., & Bobes Garcia, J. (2001). Influence of psychiatric disorders in the effectiveness of a long-term methadone maintenance treatment. Actas Españolas De Psiquiatría, 29(4), 228–232.
Florez-Menendez, G., Balcells-Oliveró, M., & Uzal-Fernández, C. (2018). Comorbilidad psiquiátrica en adicciones. Trastorno por uso de alcohol y otro trastorno mental comórbido. Guías clínicas basadas en la evidencia científica. Valencia (Socidrogoalcohol Ed.).
Fonseca, F., Robles-Martinez, M., Tirado-Munoz, J., Alias-Ferri, M., Mestre-Pinto, J. I., Coratu, A. M., & Torrens, M. (2021). A gender perspective of addictive disorders. Current Addiction Reports, 8(1), 89–99. https://doi.org/10.1007/s40429-021-00357-9
Grau-Lopez, L., Roncero, C., Daigre, C., Miquel, L., Barral, C., Gonzalvo, B., & Casas, M. (2014). Observational study on medications prescribed to dual-diagnosis outpatients. Journal of Addiction Medicine, 8(2), 84–89. https://doi.org/10.1097/ADM.0000000000000024
Gual, A. (2007). Dual diagnosis in Spain. Drug and Alcohol Review, 26(1), 65–71. https://doi.org/10.1080/09595230601037000
Guardia Serecigni, J., & Flórez Menéndez, G. (2018). Comorbilidad psiquiátrica en adicciones. Trastorno por uso de ansiolíticos e hipnóticos y otro trastorno mental comórbido. Guías clínicas basadas en la evidencia científica. Valencia (Socidrogalcohol Ed.).
Hasin, D. S., & Grant, B. F. (2015). The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: Review and summary of findings. Social Psychiatry and Psychiatric Epidemiology, 50(11), 1609–1640. https://doi.org/10.1007/s00127-015-1088-0
Hillemacher, T., & Frieling, H. (2019). Pharmacotherapeutic options for co-morbid depression and alcohol dependence. Expert Opinion on Pharmacotherapy, 20(5), 547–569. https://doi.org/10.1080/14656566.2018.1561870
Hunt, G. E., Large, M. M., Cleary, M., Lai, H. M. X., & Saunders, J. B. (2018). Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: Systematic review and meta-analysis. Drug and Alcohol Dependence, 191, 234–258. https://doi.org/10.1016/j.drugalcdep.2018.07.011
Hunt, G. E., Siegfried, N., Morley, K., Brooke-Sumner, C., & Cleary, M. (2019). Psychosocial interventions for people with both severe mental illness and substance misuse. Cochrane Database of Systematic Reviews, 12(12), 1–198. CD001088. https://doi.org/10.1002/14651858.CD001088.pub4
Iqbal, M. N., Levin, C. J., & Levin, F. R. (2019). Treatment for Substance Use Disorder With Co-Occurring Mental Illness. Focus (American Psychiatric Publishing), 17(2), 88–97. https://doi.org/10.1176/appi.focus.20180042
Mancheño-Barba, J.J., Navas-León, S., Gutiérrez-López, M. L., De la Rosa-Cáceres, A., Cáceres-Pachón, P., & Martín Lozano, O. (2019). Analysis of the profiles of patients with dual pathology attending addiction centers, mental health centers, and a coordinated service. Anal Psicol, 35(2), 233–241. https://doi.org/10.6018/analesps.35.2.345721
Mangrum, L. F., Spence, R. T., & Lopez, M. (2006). Integrated versus parallel treatment of co-occurring psychiatric and substance use disorders. Journal of Substance Abuse Treatment, 30(1), 79–84. https://doi.org/10.1016/j.jsat.2005.10.004
Maremmani, A. G. I., Rovai, L., Bacciardi, S., Rugani, F., Pacini, M., Paolo Pani, P., & Maremmani, I. (2013). The long-term outcomes of heroin dependent-treatment-resistant patients with bipolar 1 comorbidity after admission to enhanced methadone maintenance. Journal of Affective Disorders, 151(2), 582–589. https://doi.org/10.1016/j.jad.2013.06.054
Mueser, K. T., Noordsy, D. L., Drake, R. E., & Fox, L. (2003). Integrated treatment for dual disorders: A guide to effective practice. (D. H. Barlow Ed.). New York.
Murthy, P., Mahadevan, J., & Chand, P. K. (2019). Treatment of substance use disorders with co-occurring severe mental health disorders. Current Opinion in Psychiatry, 32(4), 293–299. https://doi.org/10.1097/YCO.0000000000000510
Ochoa-Mangado, E., Molins-Pascual, S., & Seijo-Ceballos, P. (2018). Comorbilidad psiquiátrica en adicciones. Trastorno por uso de cocaína y otro trastorno mental comórbido. Guías clínicas basadas en la evidencia científica. Valencia. (Socidrogalcohol Ed.).
Ortiz-Medina, M. B., Perea, M., Torales, J., Ventriglio, A., Vitrani, G., Aguilar, L., & Roncero, C. (2018). Cannabis consumption and psychosis or schizophrenia development. International Journal of Social Psychiatry, 64(7), 690–704. https://doi.org/10.1177/0020764018801690
Orwin, R. G., Francisco, L., & Bernichon, T. (2001). Effectiveness of women’s substance abuse treatment programs: A meta-analysis. Center for Substance Abuse Treatment. Arlington, Virginia: SAMHSA.
Palomo, J. L., Arias, F., Szerman, N., Vega, P., Basurte, I., & Mesías, B. (2017). Dual disorders in individuals under treatment for both alcohol and cocaine: Madrid study on the prevalence of dual disorders. Salud Mental, 40(6), 257–264. https://doi.org/10.17711/SM.0185-3325.2017.033
Pascual-Pastor, F., Fernández-Miranda, J. J., Díaz-Fernández, S., & Sala-Añó, C. (2017). Comorbilidad psiquiátrica en adicciones. Concepto, epidemiología y diagnóstico. Marco general de tratamiento. Guías clínicas basadas en la evidencia científica. Valencia (Socidrogoalcohol Ed.).
Pereiro, C., Pino, C., Florez, G., Arrojo, M., & Becona, E. (2013). Psychiatric comorbidity in patients from the addictive disorders assistance units of Galicia: The COPSIAD study. PLoS ONE, 8(6), e66451. https://doi.org/10.1371/journal.pone.0066451
Priester, M. A., Browne, T., Iachini, A., Clone, S., DeHart, D., & Seay, K. D. (2016). Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: An integrative literature review. Journal of Substance Abuse Treatment, 61, 47–59. https://doi.org/10.1016/j.jsat.2015.09.006
Roncero, C., Fuste, G., Barral, C., Rodríguez-Cintas, L., Martinez-Luna, N., Eiroa-Orosa, F., & Casas, M. (2001). Therapeutic management and comorbidities in opiate-dependent patients undergoing a replacement therapy programme in Spain: The PROTEUS study. Heroin Addiction and Related Clinical Problems, 21, 5–16.
Saiz Martinez, P. A., Jimenez Trevino, L., Diaz Mesa, E. M., Garcia-Portilla Gonzalez, M. P., Marina Gonzalez, P., Al-Halabi, S., & Ruiz, P. (2014). Dual diagnosis in anxiety disorders: Pharmacologic treatment recommendations. Adicciones, 26(3), 254–274.
Salloum, I. M., & Brown, E. S. (2017). Management of comorbid bipolar disorder and substance use disorders. American Journal of Drug and Alcohol Abuse, 43(4), 366–376. https://doi.org/10.1080/00952990.2017.1292279
Sanchez-Peña, J. F., Alvarez-Cotoli, P., & Rodriguez-Solano, J. J. (2012). Psychiatric disorders associated with alcoholism: 2 year follow-up of treatment. Actas Españolas De Psiquiatría, 40(3), 129–135.
Smith, J. P., & Randall, C. L. (2012). Anxiety and alcohol use disorders: Comorbidity and treatment considerations. Alcohol Research, 34(4), 414–431.
Spivak, S., Strain, E. C., Spivak, A., Cullen, B., Ruble, A. E., Parekh, V., & Mojtabai, R. (2020). Integrated dual diagnosis treatment among United States mental health treatment facilities: 2010 to 2018. Drug and Alcohol Dependence, 213, 108074. https://doi.org/10.1016/j.drugalcdep.2020.108074
Substance Abuse and Mental Health Services Administration, S. (2006). Substance abuse treatment for persons with co-occurring disorders treatment improvement protocol (TIP) series, No, 42. (-. HHS Publication No Ed. Substance Abuse and Mental Health Services Administration. ed.). Rockville.
Tiet, Q. Q., & Mausbach, B. (2007). Treatments for patients with dual diagnosis: A review. Alcoholism, Clinical and Experimental Research, 31(4), 513–536. https://doi.org/10.1111/j.1530-0277.2007.00336.x
Tirado-Munoz, J., Gilchrist, G., Fischer, G., Taylor, A., Moskalewicz, J., Giammarchi, C., & Torrens, M. (2018). Psychiatric comorbidity and intimate partner violence among women who inject drugs in Europe: A cross-sectional study. Archives of Women’s Mental Health, 21(3), 259–269. https://doi.org/10.1007/s00737-017-0800-3
Tirado Muñoz, J., Farre, A., Mestre-Pinto, J., Szerman, N., & Torrens, M. (2018). Dual diagnosis in depression: Treatment recommendations. Adicciones, 30(1), 66–76. https://doi.org/10.20882/adicciones.868.
Torrens, M., Mestre-Pintó, J., & Domingo-Salvany, A. (2015). Comorbidity of substance use and mental disorders in Europe (EMCDDA Ed. Vol. 19).
Torrens, M., Rossi, P. C., Martinez-Riera, R., Martinez-Sanvisens, D., & Bulbena, A. (2012). Psychiatric co-morbidity and substance use disorders: Treatment in parallel systems or in one integrated system? Substance Use and Misuse, 47(8–9), 1005–1014. https://doi.org/10.3109/10826084.2012.663296
Vitali, M., Mistretta, M., Alessandrini, G., Coriale, G., Romeo, M., Attilia, F., Interdisciplinary Study Group, C. S. S. S. S. (2018). Pharmacological treatment for dual diagnosis: A literature update and a proposal of intervention. Rivista di Psichiatria, 53(3), 160-169. https://doi.org/10.1708/2925.29419
Werner, F. M., & Covenas, R. (2017). Long-term administration of antipsychotic drugs in schizophrenia and influence of substance and drug abuse on the disease outcome. Current Drug Abuse Reviews, 10(1), 19–24. https://doi.org/10.2174/1874473710666171020104524
Acknowledgements
The authors thank the “Plan Nacional Sobre Drogas” (National Plan on Addiction- Spanish Ministry of Health) for economic and scientific support. We thank all the professionals that participated in the survey from almost all the autonomous communities, many of them Socidrogalcohol members, for their time and dedication, especially during intense professional activity due to the COVID pandemic.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This study was funded by the PNSD (National Plan on Addiction- Spanish Ministry of Health) in the call for subsidies for developing Community Programs for 2019–2020.
Author information
Authors and Affiliations
Contributions
Material preparation, data collection, and analysis were performed by Juan José Fernández Miranda, Francisco Pascual Pastor, and Silvia Díaz Fernández. Juan José Fernández Miranda wrote the first draft of the manuscript; Francisco Pascual Pastor and Silvia Díaz Fernández and all authors commented on previous versions of the manuscript. Juan José Fernández Miranda, Francisco Pascual Pastor, Silvia Díaz Fernández, Daniela Navarro, and Jorge Manzanares participated in the manuscript writing. All authors reviewed the sections and contents of the manuscript. All authors read and approved the final version of the manuscript. All authors have directly participated in the study (conceptualization, methodology, data analysis, and writing).
Corresponding author
Ethics declarations
Informed Consent
All procedures followed the ethical standards and the Helsinki Declaration of 1975, revised in 2000. This research study was conducted retrospectively from data obtained for clinical purposes, and our study did not need specific ethical approval.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fernández-Miranda, J.J., Pascual-Pastor, F., Díaz-Fernández, S. et al. Differences in Substance Use Disorders and Other Mental Disorders in Mental Health and Addiction Settings: Sociodemographic, Clinical, Drug Treatment, and Gender Differences. Int J Ment Health Addiction (2022). https://doi.org/10.1007/s11469-022-00989-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-022-00989-6