Abstract
The COVID-19 pandemic holds widespread implications for global public health, economies, societies, and the practice of orthopedic surgery. As our knowledge of the transmissibility of SARS-CoV-2 and the symptomatology and management of COVID-19 expands, orthopedic surgeons must remain up to date on the latest medical evidence and surgical perspectives. While COVID-19 primarily manifests with pulmonary symptoms, cardiovascular, neurologic, and other major organ systems may also be affected and present with hallmark imaging findings. This article reviews initial and emerging literature on clinical characteristics and imaging findings of COVID-19.
Similar content being viewed by others
Introduction
Since December 2019, infections with severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2), a novel betacoronavirus strain responsible for coronavirus disease 2019 (COVID-19), rapidly progressed from an isolated cluster of cases in the Hubei province of east central China to a pandemic, with significant global health and economic repercussions [4, 5, 10, 24, 25, 27, 28, 44, 58, 80, 91]. By mid-June 2020, the World Health Organization (WHO) had declared over 4.3 million people infected worldwide, with nearly 300,000 deaths. In the USA, despite unprecedented social distancing and public health measures, over 1.3 million people were infected, with more than 100,000 deaths [21]. Musculoskeletal chief complaints account for 18% of all healthcare visits in the USA [59], with nearly 23 million orthopedic procedures performed annually worldwide, of which five orthopedic procedures comprise 17% of all operations in the USA [4]. Public safety restrictions on semi-elective and elective office visits and surgical procedures during the COVID-19 pandemic have created a tremendous backlog (estimated at more than 1 million cases in 2 years) for orthopedic practices and have taken many practices to a tenuous economic precipice [4, 39].
As restrictions are eased nationally [1], it is critical that orthopedic surgeons remain aware of the clinical and radiographic findings associated with COVID-19 to best evaluate surgical patients. In addition to the widely known pulmonary symptoms, COVID-19 patients may initially present with atypical neurologic, gastrointestinal, cardiac, and musculoskeletal imaging findings (Table 1), which are more likely to be undiagnosed. We summarize the most recent literature describing the clinical and imaging findings in order to assist orthopedic surgeons in navigating a clinical and practice management landscape permanently transformed by the pandemic.
Pulmonary Manifestations
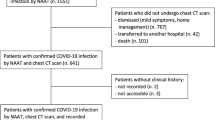
The most common symptoms of patients presenting with COVID-19 are cough, dyspnea, and fever, while the most common reasons for admission are pneumonia and hypoxemia [12, 27, 36, 80, 91]. Approximately 14% of patients develop more severe symptoms, including acute hypoxic respiratory failure and acute respiratory distress syndrome (ARDS), while the mortality rate for patients requiring invasive mechanical ventilation is high (24.7% in New York City) [68, 81]. In a recent retrospective review of chest radiographic findings in 64 patients with COVID-19, Wong et al. reported consolidation (47%) and ground glass opacities (GGO) (33%) as the most common findings, usually in a peripheral (41%) or lower lobe (51%) distribution, with bilateral lung involvement in 50% (Fig. 1) [72]. Pulmonary nodules, pleural effusions, lymphadenopathy, and lung cavitation (thick-walled abnormal gas-filled spaces within the lung) were usually absent [16]. Chest computed tomography (CT) is the gold imaging standard for diagnosing COVID-19. In a retrospective cohort study from Wuhan, including some of the earliest diagnosed patients, CT scans were reviewed sequentially from prior to symptom onset to 3 weeks after onset [72]. The authors found that even before symptom onset, CT scans demonstrated unilateral GGO that progressed to bilateral diffuse GGO, with or without consolidation [57, 72].
Early reports from China described the most common imaging findings on CT as GGO (56.4%) and bilateral patchy shadowing (51.8%) [27]. In another recent review, Pan et al. correlated time course of lung changes on CT scans with COVID-19 disease progression [61]. In the “early stage” of the disease (0 to 4 days after onset of symptoms), GGOs in subpleural locations unilaterally or bilaterally were observed (Fig. 2). During the “progressive stage” (days 5 to 8), CT scans demonstrated multilobe distribution of diffuse GGOs and crazy-paving pattern (GGOs with superimposed inter- and intralobular septal thickening), and consolidation was observed, without mediastinal lymphadenopathy (Fig. 3) [70]. In the “peak stage” (9 to 13 days), consolidations became denser, with worsening diffuse GGOs, crazy-paving, and residual parenchymal bands (Fig. 4). If patients clinically improved, they entered the “absorption stage” (usually more than 14 days after symptom onset). In this stage, GGOs persisted, but the crazy-paving resolved, and consolidations improved. If the patient worsened, with increased oxygen requirements, need for more invasive ventilation, and other intensive care unit (ICU) care, a transition to a denser alveolar consolidation pattern on radiographic imaging was noted. At this point, acute respiratory distress syndrome was likely to occur, and a low clinical threshold was necessary for transfer to an ICU for advanced respiratory support [70].
Peak stage COVID-19 (9 to 13 days): a Axial CT scan of the chest in a positive 49-year-old man with COVID-19 demonstrates ground glass opacities (GGO) in a multilobe distribution (red arrows) and bibasilar consolidations (blue arrows). b Diffuse crazy-paving pattern (GGO with superimposed inter- and intralobular septal thickening), consolidations, and residual parenchymal bands (green arrows).
There is a characteristic change in imaging of the chest, not only temporally from symptom onset but also with increasing disease severity. In a retrospective study of 83 patients, patients with more severe manifestations of COVID-19 had higher thin section CT score, incidence of consolidation, mediastinal lymph node enlargement, septal thickening, pleural effusion, and pericardial effusion than those with less severe presentations [47, 77]. Salehi et al. reviewed the imaging findings of 919 patients and corroborated this progression of severity [70]. Other uncommon findings that occur later in the progression of COVID-19 may also include bronchiectasis, pleural thickening, enlargement of intralesional pulmonary vessels greater than 3 mm in diameter, cavitation, or CT halo signs (GGOs surrounding a pulmonary nodule or mass) [66, 70]. Finally, as mentioned, disease resolution is seen with the gradual disappearance of consolidative opacities and decreased number of lesions and/or involved lobes. A recent meta-analysis of 68 articles [42] found that chest CT has a sensitivity and specificity of 94% and 37%, respectively, in detecting COVID-19 [3, 22]. Imaging characteristics of COVID-19 are distinctive enough that Chinese and American radiologists were able to differentiate COVID-19 (n = 219) from respiratory viral pneumonia (n = 205) when presented with respective imaging [6].
Cardiovascular Manifestations
Early reports from Italy and China indicated that although pulmonary diseases including ARDS and diffuse pneumonia comprise the predominant lethal complications of COVID-19, patients have also presented with or developed significant cardiac signs and symptoms [50]. In one of the first series of COVID-19 patients from Wuhan, Huang et al. [36] found that five of 41 (12%) had some form of acute cardiac injury, determined either by elevated cardiac biomarkers above the 99th percentile or new abnormalities/arrhythmias on electrocardiography or echocardiography as seen in patients with myopericarditis (Fig. 5) or myocardial infarction (Fig. 6) [50, 89]. A larger retrospective cohort study of 187 patients with laboratory positive COVID-19 demonstrated that 27.8% patients had some form of myocardial injury as defined by elevated cardiac biomarkers. Mortality rates were nearly doubled in those with preexisting cardiovascular disease (CVD) (13.33% vs. 7.62%), but mortality rates increased dramatically if acute cardiac injury occurred during hospitalization (37.5% for those without concomitant CVD and 69.44% for those with concomitant CVD) [29]. A study of 416 patients with COVID-19 found a 19.7% incidence of cardiac injury; these patients had worse laboratory markers, a higher proportion requiring advanced airway management, and higher mortality rate from symptom onset (hazard ratio (HR): 4.26 [95% CI: 1.92–9.49]) [73]. A case report from Italy described a COVID-19 patient without a CVD history who presented with electrocardiographic and biomarker changes indicative of acute cardiac injury [38]. Transthoracic echocardiography (TTE) and gadolinium-enhanced cardiac magnetic resonance imaging (Gd-cardiac MRI) demonstrated increased wall thickness, diffuse biventricular hypokinesis, severe left ventricular dysfunction, biventricular myocardial interstitial edema (on short-tau inversion and T2-mapping sequences), acute myocarditis, and pericardial effusion, especially around the right cardiac chambers.
Myopericarditis in a patient with chest pain, ST elevation, and elevated cardiac troponins: a Two chamber view and b four chamber view post-contrast cardiac MRI demonstrate curvilinear delayed enhancement in the subepicardial lateral mid and apical wall of the left ventricle and the adjacent pericardium (blue arrows).
The above suggests that COVID-19 may be related to cardiac injury of undetermined pathophysiology. Cardiac injury in the context of viral infections has been studied in the past. In a self-controlled case series involving 365 admissions in Ontario, Canada, laboratory-confirmed respiratory viral infections were associated with 6.05% increase in the incidence of acute myocardial infarction within 7 days of viral detection [45]. Viral respiratory tract infections may lead to complications such as acute coronary syndrome (ACS) or venothrombotic events (VTEs) secondary to immune system hyperactivation and generation of a thrombogenic state [18, 43].
Thromboembolic Complications
Global reports of COVID-19-associated coagulopathy with multifocal thromboembolic disease are rapidly growing and include pulmonary emboli, limb ischemia, and cerebral infarct; often associated with poorer prognosis [19, 51, 54, 75, 87, 88]. Several European studies have demonstrated higher rates of VTE in the COVID-19 population [32, 49]. In a study of 150 COVID-19 ICU patients, nearly 64 (43%) had a thrombotic event, including pulmonary embolism (Fig. 7) and continuous renal replacement therapy (CRRT) circuit clotting [32]. In a study of 48 COVID-19 ICU patients at two institutions, an alarming 85% were positive for DVTs, despite almost all being on prophylactic anticoagulation [67]. Another study of 26 ICU patients screened for DVTs using duplex ultrasonography found that 69% were positive, with 56% positive despite being on therapeutic anticoagulation [48]. Up to 30% of COVID-19 patients with pulmonary symptoms were diagnosed with acute pulmonary embolus on pulmonary CT angiogram over a 1-month period in a tertiary care center and all with higher levels of D-dimer (2660 μg/L) and C-reactive protein (CRP) than usually encountered, suggesting an independent association between D-dimer level and disease severity [46, 65]. Antiphospholipid antibodies in the setting of multifocal cerebral infarct have also been observed in COVID-19 patients [88]. While noted in other infections, antiphospholipid antibodies have not been associated with thrombotic events in these circumstances [71, 88].
Early stage COVID-19 (0 to 4 days) with acute pulmonary embolism: a Coronal CT scan of the chest (lung window) in a 79-year-old man with COVID-19 demonstrates peripheral ground glass opacities in subpleural distribution (blue arrows). b Coronal CT scan of the chest with IV contrast (soft tissue window) demonstrates filling defects within the right and left pulmonary arteries (green arrows), indicating acute pulmonary embolism.
Neurologic Manifestations
COVID-19 musculoskeletal and neurologic manifestations are being reported with increased frequency, particularly in patients with more severe respiratory disease, indicating coronavirus neurotropism possibly directly related with higher viral loads, which are now detectable in cerebrospinal fluid [20]. Angiotensin-converting enzyme 2 (ACE-2) receptors may be responsible for COVID-19 cerebral involvement via entry through the cribriform plate [56].
Reportedly, up to 84% of ICU COVID-19 patients demonstrate neurologic symptoms [31, 41]. Neuroimaging findings beyond those of acute infarction, hemorrhage, and vessel thrombosis include meningoencephalitis and acute necrotizing encephalopathy (ANE). There is mounting evidence of increased leptomeningeal enhancement, fluid-attenuated inversion recovery (FLAIR) cortical signal abnormalities, cortical diffusion restriction, and cortical blooming artifact, suggesting either infectious, autoimmune, or critical illness-related encephalitis, hypoxia, hypoglycemia, and seizure [41]. In a limited series over a 2-week period in March 2020 at a single institution, five patients under the age of 50 years suffered large vessel arterial cerebral infarct (with preferential involvement of the middle cerebral artery), a dramatic increase compared with a pre-COVID-19 average of 0.79 strokes per 2 weeks in patients younger than 50 years (Fig. 8) [60]. In a study by Mao et al. of 214 patients with COVID-19, 36.4% had neurologic symptoms, including acute ischemic stroke, intra-cranial hemorrhage (Fig. 9), impaired consciousness, and skeletal muscle injury defined as pain with elevated serum creatinine kinase levels [53, 64].
Acute thromboembolic infarction in a 57-year-old: Axial non-contrast CT scan demonstrates left hyperdense middle cerebral artery (MCA) sign (blue arrow), with increased density in the M1 segment of the left MCA, consistent with acute thromboembolic occlusion. There is subtle loss of gray-white matter differentiation, hypodensity, and engorgement along the left insular ribbon and temporal operculum (loss of insular ribbon sign), reflecting acute infarction (green arrow).
From Italy, of an estimated 1200 COVID-19 patients admitted over 1 month, five developed rapidly progressive Guillain-Barré syndrome (Fig. 10) that began with lower extremity paresis that progressed to flaccid tetraparesis and tetraplegia [76]. Mahammedi et al. reported that 108 of 725 (15%) consecutive hospitalized COVID-19 patients had neurologic symptoms requiring neuroimaging in Italy, and of those, 64 (59%) had altered mental status, and 34 (31%) had ischemic stroke; 47% of those patients had acute neuroimaging abnormalities that included acute ischemic stroke, intracranial hemorrhage (possibly due to cerebrovascular endothelial rupture), cerebral venous thrombosis, multiple sclerosis plaque exacerbation, encephalopathy, Guillain-Barré syndrome, Miller-Fisher Syndrome, and posterior reversible encephalopathy syndrome [7, 52]. In an observational study of 58 encephalopathic COVID-19 patients with ARDS, 38 had upper motor neuron signs, while eight of 13 who underwent MRI demonstrated leptomeningeal enhancement (Fig. 11), two of 13 had focal acute ischemic strokes, and 11 of 11 displayed frontotemporal hypoperfusion abnormalities on profusion studies [31]. Anosmia, possibly related to ACE-2 involvement, has also been reported [33].
Leptomeningeal enhancement and encephalitis in a 39-year-old with neurologic impairment: a Axial post-contrast MRI demonstrates leptomeningeal enhancement along the left middle cerebral artery (MCA) distribution (blue arrow). b Axial post-contrast MRI demonstrates leptomeningeal enhancement along the left MCA, as well as the basal cisterns and superior cerebellum (blue arrows).
Musculoskeletal Manifestations
Limited reports of COVID-19 isolated musculoskeletal manifestations are currently available. Similar low incidence case series of critical illness myopathy or myositis (Fig. 12) [55] and critical illness polyneuropathy following Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) have also been reported, at times with an association with concurrent myocarditis [9, 14, 74]. In all of these cases, patients typically present with myalgia and muscle weakness, with rhabdomyolysis and elevated creatine kinase (CK) levels representing more severe manifestations [27, 78, 86]. Elevated CK levels are associated with increased rates of mortality and interstitial pneumonia in COVID-19 patients [90].
Cytokine Storm
Evidence suggests that some patients with severe COVID-19 might have a cytokine storm syndrome, which can be seen by testing for serum cytokine levels [37]. Recently, ANE, a rare complication of viral infections related to intracranial cytokine storms that result in blood-brain barrier breakdown without direct viral invasion or demyelination, has been reported as a result of COVID-19 [65]. The most common findings of ANE include hypoattenuating lesions on CT and T2/FLAIR hyperintense lesions on MRI, in a bilateral symmetric multifocal distribution predominantly involving the thalami and to a lesser extent the brain stem, cerebral white matter, and cerebellum. In addition, findings of leukoencephalopathy, including CT hypoattenuation of the bilateral cerebral hemispheric white matter and corpus callosum, as well as MRI diffuse confluent white matter T2/FLAIR hyperintensities, scattered micro-hemorrhage in the corpus callosum, and posterior circulation hyperperfusion without diffusion restriction or abnormal enhancement have been reported [69]. It is uncertain if COVID-19-related white matter injury findings are the result of ICU anesthesia-related toxicity, COVID-19-associated cytokine release syndrome, or COVID-19-related endotheliitis with thrombotic microangiopathy [69].
Beyond neurologic manifestations, cytokine storm also has pulmonary manifestations, namely, pulmonary and interstitial damage caused by nonspecific inflammatory cell infiltration [83]. For COVID-19, in addition to the previously described radiographic findings, this syndrome may lead to the development of bilateral pneumonia or ARDS much faster in thus subgroup of patients, as well increased rates of ICU admission, mechanical ventilation, and subsequent mortality [83].
Even without pulmonary or neurologic manifestations, cytokine storm can lead to multi-organ system failure, which explains reports of elevated liver enzymes, creatine, and other important markers in COVID-19 patients who do not present with the above manifestations [83]. This is due to the systemic exposure to large amounts of pro-inflammatory cytokines that leads to the immune system “attacking” the body, particularly interstitial and parenchymal spaces [17]. Vascular compromise due to extensive endothelial damage is also possible [79].
Gastrointestinal and Hepatic Manifestations
Though not as severe, gastrointestinal symptoms have been reported in up to 20% of COVID-19 patients [15]. This may be due to the increased gastrointestinal wall permeability to viral pathogens, which promote malabsorption by infected enterocytes [26]. The most common symptoms include diarrhea, abdominal pain, or vomiting, though preliminary data suggests that patients with these symptoms tend to have an improved prognosis independent of patient age or sex [2]. Constipation, melena, and anorexia have also been reported but less commonly [34, 85]. More severe manifestations of gastroenteritis can be seen on CT scan and can be the only presenting symptom (Fig. 13) [30, 62]. Patients can have pertinent laboratory findings, namely, elevated lipase and/or alkaline phosphatase levels, which are associated with poor prognosis as they reflect a greater systemic inflammatory response [2].
The most common abdominal imaging findings in COVID-19 ICU patients include small and large bowel wall thickening, non-enhancing bowel, pneumatosis, portal venous gas, and bowel perforation, all related to bowel and mesenteric ischemia, infarction, and necrosis (Fig. 14) [11]. Portal vein thrombosis and distended gallbladder containing sludge suggestive of cholestasis have also been observed. In addition, evidence of inflammation and infarction in other solid organs, including the pancreas, liver, kidneys, and spleen, have been reported, particularly in ICU COVID-19 patients. Although the exact pathophysiology is uncertain, these findings are thought to be multifactorial in origin, resulting from a combination of direct SARS-CoV-2 infection and indirect systemic derangements associated with critical illness, including small vessel thrombosis related to ICU hypercoagulopathy and nonocclusive ischemia related to an ICU hyperinflammatory effect [11, 35].
Though preliminary in nature, current findings may suggest that SARS-CoV-2 can be detectable in both hepatic tissue and cholangiocytes due to ACE-2 expression [13]. Elevated liver enzymes have been found in blood samples of COVID-19 patients, but it is important to note that elevated liver enzymes do not necessarily mean liver damage is present [23]. Imaging is currently not indicated for evaluation of hepatic pathology in COVID-19 patients, but hepatic steatosis and mild lobular and portal inflammation may be seen. Whether these are indeed due to COVID-19 or the consequence of drug-induced hepatic injury is still unknown [82].
Renal Dysfunction
Recent studies suggest that COVID-19 may cause acute renal failure, as both podocytes and proximal convoluted tubular cells express certain genes (ACE-2 and transmembrane serine protease 2 [TMPRSS2]) that increase the host viability for SARS-CoV-2 [63]. The viral cytopathic effect on these cells has been linked as the cause of acute renal failure, which is secondary to ARDS as one of the more common fatal presentations in patients with COVID-19 [82]. Separately, a case report found that patients who developed rhabdomyolysis throughout the course of their disease are also at risk for acute renal failure, with manifestations of lower extremity pain and fatigue (separate from generalized myositis) followed by rising plasma creatine level [40].
Renal imaging studies currently have little to no diagnostic role in COVID-19 patients, though one would theoretically expect to note increased parenchymal echogenicity via ultrasound [8]. In fact, it is more important to keep in mind that while COVID-19 patients primarily present with respiratory findings, acute renal injury should be suspected until proven otherwise, as contrast-induced nephropathy secondary to contrast-enhanced CT or MRI imaging studies may exacerbate already present renal damage secondary to COVID-19 [84].
Clinical and basic science research, as well as national public health guidance, regarding COVID-19 is rapidly and continuously evolving. It has been described as a novel, “once-in-a-century” disease. Along with our medicine and public health colleagues, orthopedic surgeons and orthopedic care providers should remain up to date on the latest COVID-19 peer-reviewed evidence, not only to better respond to changes in our clinical practice and to accurately counsel surgical patients but also to ultimately practice safe and efficacious surgery for patients in a new and changing clinical environment. In addition to the widely known pulmonary symptoms, COVID-19 may affect the neurologic, gastrointestinal, cardiac, and musculoskeletal systems (Table 1). Musculoskeletal issues remain underrecognized at this point, which may be due to the low prevalence of this disease at this time. Overall, it is imperative that all healthcare professionals have a broader understanding of all of the possible clinical and imaging manifestations of this global pandemic to improve patient and community outcomes.
Change history
12 October 2020
The published article listed an incorrect credential for Jose Rodriguez, MD. It is corrected here.
References
Opening Up America Again. The White House. 05/07/2020. Available at www.whitehouse.gov/openingamerica/. Accessed 05/14, 2020.
Aghemo A, Piovani D, Parigi TL, et al. COVID-19 digestive system involvement and clinical outcomes in a large academic hospital in Milan, Italy [published online ahead of print, 2020 May 11]. Clin Gastroenterol Hepatol. 2020;S1542-3565(20)30646-7. https://doi.org/10.1016/j.cgh.2020.05.011
Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases [published online ahead of print, 2020 Feb 26]. Radiology. 2020;200642. https://doi.org/10.1148/radiol.2020200642
Anoushiravani AA, O’Connor CM, DiCaprio MR, Iorio R. Economic impacts of the COVID-19 crisis: an orthopedic perspective. J Bone Joint Surg Am. 2020;102(11):937–941. https://doi.org/10.2106/JBJS.20.00557
Atkeson A. What will be the economic impact of COVID-19 in the US? Rough estimates of disease scenarios: National Bureau of Economic Research; 2020. 0898-2937.
Bai HX, Hsieh B, Xiong Z, et al. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT [published online ahead of print, 2020 Mar 10]. Radiology. 2020;200823. https://doi.org/10.1148/radiol.2020200823
Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–998. https://doi.org/10.1021/acschemneuro.0c00122
Behzad S, Aghaghazvini L, Radmard AR, Gholamrezanezhad A. Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview [published online ahead of print, 2020 May 18]. Clin Imaging. 2020;66:35–41. https://doi.org/10.1016/j.clinimag.2020.05.013
Beydon M, Chevalier K, Al Tabaa O, et al. Myositis as a manifestation of SARS-CoV-2 [published online ahead of print, 2020 Apr 23]. Ann Rheum Dis. 2020;annrheumdis- 2020-217573. https://doi.org/10.1136/annrheumdis-2020-217573
Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle Region: Case Series. N Engl J Med. 2020;382(21):2012–2022. https://doi.org/10.1056/NEJMoa2004500
Bhayana R, Som A, Li MD, et al. Abdominal imaging findings in COVID-19:preliminary observations [published online ahead of print, 2020 May 11]. Radiology. 2020;201908. https://doi.org/10.1148/radiol.2020201908
Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment coronavirus (COVID-19). Statpearls [internet]: StatPearls Publishing; 2020.
Chai X, Hu L, Zhang Y, et al. Specific ACE2 Expression in cholangiocytes may cause liver damage after 2019-nCoV infection [preprint]. bioRxiv. 2020:2020.2002.2003.931766.
Chao CC, Tsai LK, Chiou YH, et al. Peripheral nerve disease in SARS: report of a case. Neurology. 2003;61(12):1820–1821. https://doi.org/10.1212/01.wnl.0000099171.26943.d0
Cheung KS, Hung IFN, Chan PPY, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis [published online ahead of print, 2020 Apr 3]. Gastroenterology. 2020;S0016-5085(20)30448-0. https://doi.org/10.1053/j.gastro.2020.03.065
Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020;295(1):202–207. https://doi.org/10.1148/radiol.2020200230
Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in COVID-19: An overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev. 2020;53:25–32. https://doi.org/10.1016/j.cytogfr.2020.05.003
Corrales-Medina VF, Madjid M, Musher DM. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10(2):83–92. https://doi.org/10.1016/S1473-3099(09)70331-7
Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J. 2020;41(19):1858. https://doi.org/10.1093/eurheartj/ehaa254
Desforges M, Le Coupanec A, Dubeau P, et al. Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses. 2019;12(1):14. https://doi.org/10.3390/v12010014
Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time [published correction appears in Lancet Infect Dis. 2020 Jun 12]. Lancet Infect Dis. 2020;20(5):533–534. https://doi.org/10.1016/S1473-3099(20)30120-1
Fang Y, Zhang H, Xie J, et al. Sensitivity of Chest CT for COVID-19: comparison to RTPCR [published online ahead of print, 2020 Feb 19]. Radiology. 2020;200432. https://doi.org/10.1148/radiol.2020200432
Feng G, Zheng KI, Yan QQ, et al. COVID-19 and liver dysfunction: current insights and emergent therapeutic strategies. J Clin Transl Hepatol. 2020;8(1):18–24. https://doi.org/10.14218/JCTH.2020.00018
Fernandes N. Economic effects of coronavirus outbreak (COVID-19) on the world economy. Available at SSRN 3557504. 2020.
Goyal P, Choi JJ, Pinheiro LC, et al. Clinical Characteristics of Covid-19 in New York City. N Engl J Med. 2020;382(24):2372–2374. https://doi.org/10.1056/NEJMc2010419
Gu J, Han B, Wang J. COVID-19: Gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158(6):1518–1519. https://doi.org/10.1053/j.gastro.2020.02.054
Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. https://doi.org/10.1056/NEJMoa2002032
Gudbjartsson DF, Helgason A, Jonsson H, et al. Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med. 2020;382(24):2302–2315. https://doi.org/10.1056/NEJMoa2006100
Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) [published online ahead of print, 2020 Mar 27]. JAMA Cardiol. 2020;e201017. https://doi.org/10.1001/jamacardio.2020.1017
Han C, Duan C, Zhang S, et al. Digestive symptoms in covid-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020;115(6):916–923. https://doi.org/10.14309/ajg.0000000000000664
Helms J, Kremer S, Merdji H, et al. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med. 2020;382(23):2268–2270. https://doi.org/10.1056/NEJMc2008597
Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–1098. https://doi.org/10.1007/s00134-020-06062-x
Hopkins C, Surda P, Kumar N. Presentation of new onset anosmia during the COVID-19 pandemic. Rhinology. 2020;58(3):295–298. https://doi.org/10.4193/Rhin20.116
Hormati A, Shahhamzeh A, Afifian M, Khodadust F, Ahmadpour S. Can COVID-19 present unusual GI symptoms? J Microbiol Immunol Infect. 2020;53(3):384–385. https://doi.org/10.1016/j.jmii.2020.03.020
Hossain R, Lazarus MS, Roudenko A, et al. CT scans obtained for nonpulmonary indications: associated respiratory findings of COVID-19 [published online ahead of print, 2020 May 11]. Radiology. 2020;201743. https://doi.org/10.1148/radiol.2020201743
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China [published correction appears in Lancet. 2020 Jan 30]. Lancet. 2020;395(10223):497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Huang Q, Deng X, Li Y, et al. Clinical characteristics and drug therapies in patients with the common-type coronavirus disease 2019 in Hunan, China. Int J Clin Pharm. 2020;42(3):837–845. https://doi.org/10.1007/s11096-020-01031-2
Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) [published online ahead of print, 2020 Mar 27]. JAMA Cardiol. 2020;10.1001/jamacardio.2020.1096. https://doi.org/10.1001/jamacardio.2020.1096
Jain A, Jain P, Aggarwal S. SARS-CoV-2 impact on elective orthopaedic surgery: implications for post-pandemic recovery [published online ahead of print, 2020 May 12]. J Bone Joint Surg Am. 2020;10.2106/JBJS.20.00602. https://doi.org/10.2106/JBJS.20.00602
Jin M, Tong Q. Rhabdomyolysis as potential late complication associated with COVID-19. Emerg Infect Dis. 2020;26(7):1618–1620. https://doi.org/10.3201/eid2607.200445
Kandemirli SG, Dogan L, Sarikaya ZT, et al. Brain MRI findings in patients in the intensive care unit with COVID-19 infection [published online ahead of print, 2020 May 8]. Radiology. 2020;201697. https://doi.org/10.1148/radiol.2020201697
Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptasepolymerase chain reaction for coronavirus disease 2019: a meta-analysis [published online ahead of print, 2020 Apr 17]. Radiology. 2020;201343. https://doi.org/10.1148/radiol.2020201343
Kreutz RP, Bliden KP, Tantry US, Gurbel PA. Viral respiratory tract infections increase platelet reactivity and activation: an explanation for the higher rates of myocardial infarction and stroke during viral illness. J Thromb Haemost. 2005;3(9):2108–2109. https://doi.org/10.1111/j.1538-7836.2005.01474.x
COVID-19 Investigation Team. Clinical and virologic characteristics of the first 12 patients with coronavirus disease 2019 (COVID-19) in the United States. Nat Med. 2020;26(6):861–868. https://doi.org/10.1038/s41591-020-0877-5
Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378(4):345–353. https://doi.org/10.1056/NEJMoa1702090
Leonard-Lorant I, Delabranche X, Severac F, et al. Acute pulmonary embolism in COVID-19 patients on CT angiography and relationship to D-dimer levels [published online ahead of print, 2020 Apr 23]. Radiology. 2020;201561. https://doi.org/10.1148/radiol.2020201561
Li K, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55(6):327–331. https://doi.org/10.1097/RLI.0000000000000672
Llitjos JF, Leclerc M, Chochois C, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020;18(7):1743–1746. https://doi.org/10.1111/jth.14869
Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. https://doi.org/10.1016/j.thromres.2020.04.024
Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38(7):1504–1507. https://doi.org/10.1016/j.ajem.2020.04.048
Lushina N, Kuo JS, Shaikh HA. Pulmonary, cerebral, and renal thromboembolic disease associated with covid-19 infection [published online ahead of print, 2020 Apr 23]. Radiology. 2020;201623. https://doi.org/10.1148/radiol.2020201623
Mahammedi A, Saba L, Vagal A, et al. Imaging in neurological disease of hospitalized covid-19 patients: an Italian multicenter retrospective observational study [published online ahead of print, 2020 May 21]. Radiology. 2020;201933. https://doi.org/10.1148/radiol.2020201933
Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China [published online ahead of print, 2020 Apr 10]. JAMA Neurol. 2020;77(6):1–9. https://doi.org/10.1001/jamaneurol.2020.1127
Mei H, Hu Y. Zhonghua Xue Ye Xue Za Zhi. 2020;41(3):185–191. https://doi.org/10.3760/cma.j.issn.0253-2727.2020.0002
Nascimento FA, Gatto LA, Lages RO, Neto HM, Demartini Z, Koppe GL. Diffuse idiopathic skeletal hyperostosis: A review. Surg Neurol Int. 2014;5(Suppl 3):S122–S125. Published 2014 Apr 16. https://doi.org/10.4103/2152-7806.130675
Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82(15):7264–7275. https://doi.org/10.1128/JVI.00737-08
Ng MY, Lee EYP, Yang J, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2(1):e200034. Published 2020 Feb 13. https://doi.org/10.1148/ryct.2020200034
Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020;78:185–193. https://doi.org/10.1016/j.ijsu.2020.04.018
Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States. United States Census Bureau, Economics and Statistics Administration; 2014.
Oxley TJ, Mocco J, Majidi S, et al. Large-vessel stroke as a presenting feature of covid-19 in the young. N Engl J Med. 2020;382(20):e60. https://doi.org/10.1056/NEJMc2009787
Pan F, Ye T, Sun P, et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology. 2020;295(3):715–721. https://doi.org/10.1148/radiol.2020200370
Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766–773. https://doi.org/10.14309/ajg.0000000000000620
Pan XW, Xu D, Zhang H, Zhou W, Wang LH, Cui XG. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: a study based on single-cell transcriptome analysis. Intensive Care Med. 2020;46(6):1114–1116. https://doi.org/10.1007/s00134-020-06026-1
Pleasure SJ, Green AJ, Josephson SA. The spectrum of neurologic disease in the severe acute respiratory syndrome coronavirus 2 pandemic infection: neurologists move to the frontlines [published online ahead of print, 2020 Apr 10]. JAMA Neurol. 2020;10.1001/jamaneurol.2020.1065. https://doi.org/10.1001/jamaneurol.2020.1065
Poyiadji N, Cormier P, Patel PY, et al. Acute pulmonary embolism and COVID-19 [published online ahead of print, 2020 May 14]. Radiology. 2020;201955. https://doi.org/10.1148/radiol.2020201955
Qanadli SD, Beigelman-Aubry C, Rotzinger DC. Vascular changes detected with thoracic CT in coronavirus disease (COVID-19) might be significant determinants for accurate diagnosis and optimal patient management. AJR Am J Roentgenol. 2020;215(1):W15. https://doi.org/10.2214/AJR.20.23185
Ren B, Yan F, Deng Z, et al. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID-19 in Wuhan [published online ahead of print, 2020 May 15]. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.120.047407
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area [published online ahead of print, 2020 Apr 22] [published correction appears in 10.1001/jama.2020.7681]. JAMA. 2020;323(20):2052–2059. https://doi.org/10.1001/jama.2020.6775
Sachs JR, Gibbs KW, Swor DE, et al. COVID-19-Associated Leukoencephalopathy [published online ahead of print, 2020 May 14]. Radiology. 2020;201753. https://doi.org/10.1148/radiol.2020201753
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. https://doi.org/10.2214/AJR.20.23034
Sène D, Piette JC, Cacoub P. Anticorps antiphospholipide, syndrome des anticorps antiphospholipides et infections virales [Antiphospholipid antibodies, antiphospholipid syndrome and viral infections]. Rev Med Interne. 2009;30(2):135–141. https://doi.org/10.1016/j.revmed.2008.05.020
Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. https://doi.org/10.1016/S1473-3099(20)30086-4
Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China [published online ahead of print, 2020 Mar 25]. JAMA Cardiol. 2020;e200950. https://doi.org/10.1001/jamacardio.2020.0950
Stainsby B, Howitt S, Porr J. Neuromusculoskeletal disorders following SARS: a case series. J Can Chiropr Assoc. 2011;55(1):32–39.
Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. https://doi.org/10.1111/jth.14768
Toscano G, Palmerini F, Ravaglia S, et al. Guillain-Barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020;382(26):2574–2576. https://doi.org/10.1056/NEJMc2009191
Valette X, du Cheyron D, Goursaud S. Mediastinal lymphadenopathy in patients with severe COVID-19 [published online ahead of print, 2020 Apr 21]. Lancet Infect Dis. 2020;S1473-3099(20)30310-8. https://doi.org/10.1016/S1473-3099(20)30310-8
Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China [published online ahead of print, 2020 Feb 7]. JAMA. 2020;323(11):1061–1069. https://doi.org/10.1001/jama.2020.1585
Wang H, Ma S. The cytokine storm and factors determining the sequence and severity of organ dysfunction in multiple organ dysfunction syndrome. Am J Emerg Med. 2008;26(6):711–715. https://doi.org/10.1016/j.ajem.2007.10.031
Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China [published correction appears in Nature. 2020 Apr;580(7803):E7]. Nature. 2020;579(7798):265–269. https://doi.org/10.1038/s41586-020-2008-3
Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention [published online ahead of print, 2020 Feb 24]. JAMA. 2020;10.1001/jama.2020.2648. https://doi.org/10.1001/jama.2020.2648
Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome [published correction appears in Lancet Respir Med. 2020 Feb 25]. Lancet Respir Med. 2020;8(4):420–422. https://doi.org/10.1016/S2213-2600(20)30076-X
Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J Infect. 2020;80(6):607–613. https://doi.org/10.1016/j.jinf.2020.03.037
Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and multiorgan response. Curr Probl Cardiol. 2020;45(8):100618. https://doi.org/10.1016/j.cpcardiol.2020.100618
Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China [published online ahead of print, 2020 Feb 19]. Allergy. 2020;10.1111/all.14238. https://doi.org/10.1111/all.14238
Zhang Q, Shan KS, Minalyan A, O'Sullivan C, Nace T. A rare presentation of coronavirus disease 2019 (COVID-19) induced viral myositis with subsequent rhabdomyolysis. Cureus. 2020;12(5):e8074. Published 2020 May 12. https://doi.org/10.7759/cureus.8074
Zhang Y, Cao W, Xiao M, et al. Zhonghua Xue Ye Xue Za Zhi. 2020;41(0):E006. https://doi.org/10.3760/cma.j.issn.0253-2727.2020.0006
Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19. N Engl J Med. 2020;382(17):e38. https://doi.org/10.1056/NEJMc2007575
Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260. https://doi.org/10.1038/s41569-020-0360-5
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020 Mar 28;395(10229):1038] [published correction appears in Lancet. 2020 Mar 28;395(10229):1038]. Lancet. 2020;395(10229):1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3
Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. https://doi.org/10.1056/NEJMoa2001017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest: Gireesh B. Reddy, MD, Dylan N. Greif, BA, Jose Rodriguez, MD, Thomas M. Best, MD, PhD, Harry G. Greditzer IV, MD, and Jean Jose, DO declare that they have no conflicts of interest.
Human/Animal Rights: N/A
Informed Consent: N/A
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reddy, G.B., Greif, D.N., Rodriguez, J. et al. Clinical Characteristics and Multisystem Imaging Findings of COVID-19: An Overview for Orthopedic Surgeons. HSS Jrnl 16 (Suppl 1), 112–123 (2020). https://doi.org/10.1007/s11420-020-09775-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-020-09775-3