Abstract
Background
The most common modes of failure of cemented unicompartmental knee arthroplasty (UKA) designs are aseptic loosening and unexplained pain at short- to mid-term follow-up, which is likely linked to early fixation failure. Determining these modes of failure remains challenging; conventional radiographs are limited for use in assessing radiolucent lines, with only fair sensitivity and specificity for aseptic loosening.
Questions/Purposes
We sought to characterize the bone-component interface of patients with symptomatic cemented medial unicompartmental knee arthroplasty (UKA) using magnetic resonance imaging (MRI) and to determine the relationship between MRI and conventional radiographic findings.
Methods
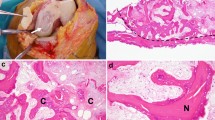
This retrospective observational study included 55 consecutive patients with symptomatic cemented UKA. All underwent MRI with addition of multiacquisition variable-resonance image combination (MAVRIC) at an average of 17.8 ± 13.9 months after surgery. MRI studies were reviewed by two independent musculoskeletal radiologists. MRI findings at the bone-cement interface were quantified, including bone marrow edema, fibrous membrane, osteolysis, and loosening. Radiographs were reviewed for existence of radiolucent lines. Inter-rater agreement was determined using Cohen’s κ statistic.
Results
The vast majority of symptomatic UKA patients demonstrated bone marrow edema pattern (71% and 75%, respectively) and fibrous membrane (69% and 89%, respectively) at the femoral and tibial interface. Excellent and substantial inter-rater agreement was found for the femoral and tibial interface, respectively. Furthermore, MRI findings and radiolucent lines observed on conventional radiographs were poorly correlated.
Conclusion
MRI with the addition of MAVRIC sequences could be a complementary tool for assessing symptomatic UKA and for quantifying appearances at the bone-component interface. This technique showed good reproducibility of analysis of the bone-component interface after cemented UKA. Future studies are necessary to define the bone-component interface of symptomatic and asymptomatic UKA patients.



Similar content being viewed by others
References
Abu-Amer Y, Darwech I, Clohisy JC. Aseptic loosening of total joint replacements: mechanisms underlying osteolysis and potential therapies. Arthritis Res Ther. 2007;9(Suppl 1):S6.
Agten CA, Del Grande F, Fucentese SF, Blatter S, Pfirrmann CWA, Sutter R. Unicompartmental knee arthroplasty MRI: impact of slice-encoding for metal artefact correction MRI on image quality, findings and therapy decision. Eur Radiol. 2015;25(7):2184–2193.
Berkowitz JL, Potter HG. Advanced MRI techniques for the hip joint: focus on the postoperative hip. Am J Roentgenol. 2017;209(3):534–543.
Chou DTS, Swamy GN, Lewis JR, Badhe NP. Revision of failed unicompartmental knee replacement to total knee replacement. Knee. 2012;19(4):356–359.
Citak M, Dersch K, Kamath AF, Haasper C, Gehrke T, Kendoff D. Common causes of failed unicompartmental knee arthroplasty: a single-centre analysis of four hundred and seventy one cases. Int Orthop. 2014;38(5):961–965.
van der List JP, Zuiderbaan HA, Pearle AD. Why do medial unicompartmental knee arthroplasties fail today? J Arthroplasty. 2016;31(5):1016–1021.
Epinette J-A, Brunschweiler B, Mertl P, Mole D, Cazenave A, French Society for Hip and Knee. Unicompartmental knee arthroplasty modes of failure: wear is not the main reason for failure: a multicentre study of 418 failed knees. Orthop Traumatol Surg Res. 2012;98(6 Suppl):S124–30.
Fritz J, Lurie B, Potter HG. MR Imaging of knee arthroplasty implants. RadoiGraphics. 2015;35(5):1483–1501.
Goodfellow JW, Kershaw CJ, Benson MK, O’Connor JJ. The Oxford Knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg Br. 1988;70(5):692–701.
Gulati A, Chau R, Pandit HG, et al. The incidence of physiological radiolucency following Oxford unicompartmental knee replacement and its relationship to outcome. J Bone Joint Surg Br. 2009;91(7):896–902.
Halawa M, Lee AJ, Ling RS, Vangala SS. The shear strength of trabecular bone from the femur, and some factors affecting the shear strength of the cement-bone interface. Arch Orthop Trauma Surg. 1978;92(1):19–30.
Hayashi D, Englund M, Roemer FW, et al. Knee malalignment is associated with an increased risk for incident and enlarging bone marrow lesions in the more loaded compartments: The MOST study. Osteoarthr Cartil. 2012;20(11):1227–1233.
Hayter CL, Koff MF, Shah P, Koch KM, Miller TT, Potter HG. MRI after arthroplasty: Comparison of MAVRIC and conventional fast spin-echo techniques. Am J Roentgenol. 2011;197(3):405–411.
Hayter CL, Gold SL, Koff MF, et al. MRI findings in painful metal-on-metal hip arthroplasty. Am J Roentgenol. 2012;199(4):884–893.
Heyse TJ, Chong LR, Davis J, Boettner F, Haas SB, Potter HG. MRI analysis of the component-bone interface after TKA. Knee. 2012;19(4):290–294.
Heyse TJ, Figiel J, Hähnlein U, et al. MRI after unicondylar knee arthroplasty: the preserved compartments. Knee. 2012;19(6):923–926.
Hooper GJ, Maxwell AR, Wilkinson B, et al. The early radiological results of the uncemented Oxford medial compartment knee replacement. J Bone Joint Surg Br. 2012;94(3):334–338.
Hooper N, Snell D, Hooper G, Maxwell R, Frampton C. The five-year radiological results of the uncemented Oxford medial compartment knee arthroplasty. Bone Joint J. 2015;97–B(10):1358–1363.
Jacobs CA, Christensen CP, Karthikeyan T. Subchondral bone marrow edema had greater effect on postoperative pain after medial unicompartmental knee arthroplasty than total knee arthroplasty. J Arthroplasty. 2016;31(2):491–494.
Kalra S, Smith TO, Berko B, Walton NP. Assessment of radiolucent lines around the Oxford unicompartmental knee replacement: sensitivity and specificity for loosening. J Bone Joint Surg Br. 2011;93(6):777–781.
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD. Regional femoral and tibial radiolucency in cemented unicompartmental knee arthroplasty and the relationship to functional outcomes. J Arthroplasty. 2017;32(11):3345–3351.
Koff MF, Shah P, Potter HG. Clinical implementation of MRI of joint arthroplasty. Am J Roentgenol. 2014;203(1):154–161.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159.
Li AE, Sneag DB, Iv HGG, Johnson CC, Miller TT, Potter HG. Total Knee Arthroplasty: diagnostic accuracy of patterns of synovitis at MR imaging 1. Radiology. 2016;281(2):1–8.
Malcherczyk D, Figiel J, Hahnlein U, Fuchs-Winkelmann S, Efe T, Heyse TJ. MRI following UKA: The component-bone interface. Acta Orthop Belg. 2015;81(1):84–89.
Mandalia V, Eyres K, Schranz P, Toms AD. Evaluation of patients with a painful total knee replacement. J Bone Jt Surg Br. 2008;90–B(3):265–271.
Mukherjee K, Pandit H, Dodd CAF, Ostlere S, Murray DW. The Oxford unicompartmental knee arthroplasty: a radiological perspective. Clin Radiol. 2008;63(10):1169–1176.
Park CN, Zuiderbaan HA, Chang A, Khamaisy S, Pearle AD, Ranawat AS. Role of magnetic resonance imaging in the diagnosis of the painful unicompartmental knee arthroplasty. Knee. 2015;22(4):341–346.
Potter HG, Foo LF. Magnetic resonance imaging of joint arthroplasty. Orthop Clin North Am. 2006;37(3):361–373.
Small SR, Berend ME, Rogge RD, Archer DB, Kingman AL, Ritter MA. Tibial loading after UKA: Evaluation of tibial slope, resection depth, medial shift and component rotation. J Arthroplasty. 2013;28(9 SUPPL):179–183.
Sofka CM, Potter HG, Figgie M, Laskin R. Magnetic resonance imaging of total knee arthroplasty. Clin Orthop Relat Res. 2003;(406):129–135.
Talbot BS, Weinberg EP. MR imaging with metal-suppression sequences for evaluation of total joint arthroplasty. Radiographics. 2015;36(1):209–225.
Temmerman OPP, Raijmakers PGHM, Berkhof J, Hoekstra OS, Teule GJJ, Heyligers IC. Accuracy of diagnostic imaging techniques in the diagnosis of aseptic loosening of the femoral component of a hip prosthesis: a meta-analysis. J Bone Joint Surg Br. 2005;87(6):781–785.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Laura J. Kleeblad, MD, Hendrik A. Zuiderbaan, MD, PhD, Alissa J. Burge, MD, Mark J. Amirtharaj, BS, declare that they have no conflicts of interest. Hollis G. Potter, MD, reports receiving grants from GE Healthcare, during the conduct of the study. Andrew D. Pearle, MD, reports receiving personal fees from Stryker Corporation and Exactech and personal fees from Zimmer Biomet, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Additional information
Level of Evidence: IV
Rights and permissions
About this article
Cite this article
Kleeblad, L.J., Zuiderbaan, H.A., Burge, A.J. et al. MRI Findings at the Bone-Component Interface in Symptomatic Unicompartmental Knee Arthroplasty and the Relationship to Radiographic Findings. HSS Jrnl 14, 286–293 (2018). https://doi.org/10.1007/s11420-018-9629-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-018-9629-1