Abstract
Purpose
The primary objective of this study was to evaluate the environmental impact and financial cost of repairing surgical scissors.
Methods
We used life cycle assessment (LCA) and life cycle cost analysis to estimate environmental impacts and financial cost of repairing surgical scissors. The functional unit was one use of a reusable surgical scissor (manufactured in Germany and used in the UK), and three baseline scenarios were compared: no repair, onsite (hospital), and offsite (external contract) repair. This ‘cradle-to-grave’ analysis included raw material extraction, manufacture of scissors and materials within primary and secondary packaging, transportation, decontamination, repair (where relevant), and waste disposal. Primary activity data was sourced from the instrument manufacturer, supplier, and from UK repair centres (both onsite and offsite), whilst the Ecoinvent database was used as a secondary data source for the manufacture of scissors. The World ReCiPe Midpoint and Endpoint Hierarchist method (Version 1.1) was used for environmental impact assessment. Scenario analysis was used to evaluate the impact of altering different assumptions, including number of uses, reducing number of repairs, increasing distance to offsite repair centre, and alternative electricity sources and waste handling processes. Life cycle cost analysis was calculated based on purchase cost, and cost of decontamination, repair, and waste disposal.
Results and discussion
The carbon footprint of reusable scissors was 70 g CO2e per use, assuming scissors were used 40 times before replacement. This was reduced by 19% through use of offsite repair every 40 uses (57 g CO2e/scissor use), with small additional reductions associated with onsite repair (56 g CO2e/scissor use). Similar patterns of reduction were calculated for eighteen midpoint environmental impact categories (mean impact reduction of 30% for those repaired offsite relative to no repair) and also across three endpoint categories. Decontamination made the biggest contribution to the carbon footprint across all baseline scenarios (76% where no repair, 95–97% where repaired offsite and onsite respectively). Findings were robust to alternative scenario analyses. Life cycle cost was GBP £1.43 per use of reusable scissors, and when repaired either on- or offsite this decreased by 32% to GBP £0.97 per use.
Conclusion
Repairing surgical scissors rather than replacing them with a new pair can reduce environmental and financial cost. The extent to which repair may play a role in mitigating the environmental impact of other surgical instruments requires further research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The Sixth Assessment Report of the Intergovernmental Panel on Climate Change concluded that human activity is the unequivocal cause of rapid global warming of the atmosphere, land, and oceans, and driven largely by anthropogenic (man-made) emissions of greenhouse gases (GHG) such as carbon dioxide (CO2), methane, nitrous oxide, halogenated gases, volatile organic compounds, and carbon monoxide (IPCC 2021). Climate change threatens public health, for example through heat stress and extreme weather events, poor air quality, food and water insecurity, and transmission of climate-sensitive infectious disease (Romanello et al. 2021). Vulnerable populations are at greatest risk of climate-related health risks, and are often least able to adapt, exacerbating health inequalities (Romanello et al. 2021). For example, coastal communities (commonly experiencing higher levels of socioeconomic deprivation and greater burdens of disease compared with those inland) (Asthana and Gibson 2021) are at greatest risk of forced migration relating to rising sea levels associated with global warming (Shukla et al. 2021). The IPCC report indicates that rapid and sustained reductions in GHG emissions are required to limit future climate change (IPCC 2021), and this will require globalised action across all industries. The contribution of the healthcare sector to national GHG emissions (measured in million metric tonnes of carbon dioxide equivalents, Mt CO2e) has been evaluated in a variety of settings, including the USA (655 Mt CO2e, 10% of national total; Eckelman and Sherman 2016), China (315 Mt CO2e, 3%; Wu 2019), and Australia (36 Mt CO2e, 7%; Malik et al. 2018). Whilst the National Health System (NHS) in England was the first to pledge to reach Net Zero carbon emissions by 2045 (NHS England, NHS Improvement 2020), 46 countries recently committed to developing low carbon, sustainable health systems at the 26th United Nations Climate Change Conference (World Health Organisation 2021).
Every aspect of the healthcare system will need to be examined to deliver against these ambitious targets. Metrics can be used to support this, providing a baseline against which interventions can be judged. Life cycle assessment (LCA) can be used to estimate environmental impacts of different products or processes, with the results used to evaluate reduction strategies. This is typically undertaken through a ‘cradle-to-grave’ approach that accounts for all stages of the product life cycle: from raw material extraction to disposal. One major component of most LCAs is the carbon footprint which estimates the GHG emissions associated with a given product or process, which can be summated and equated to carbon dioxide equivalents (CO2e).
Medical equipment was estimated to contribute 10% of NHS emissions in England (which includes products used directly for delivery of healthcare such as surgical instruments, syringes for administering medications, and medical gloves), with a further 8% from non-medical equipment (which may include products which support the delivery of healthcare services such as furniture, computers, and office supplies) (Tennison et al. 2021). Two systematic reviews of studies evaluating carbon footprint of surgical operations found the main sources of emissions related to single-use equipment, anaesthetic gases, and electricity usage, although the relative contribution will depend on the setting and operation, alongside methodological choices including assumptions and system boundaries (Rizan et al. 2020, Drew et al. 2021). For example, procurement of medical equipment was responsible for around 45% (UK)–75% (India) of GHG emissions associated with a cataract operation (Thiel et al. 2017). This study focuses specifically on repair of surgical scissors (which are surgical instruments, in turn an example of surgical equipment, and classified under the general category of medical equipment), and is contextualised within wider strategies which may be used to mitigate the carbon footprint of surgical equipment used within the operating theatre.
The benefit of reducing or eliminating use of surgical equipment on associated environmental impact is self-evident. In the surgical context, gloves are clearly appropriate where there is risk of contact with bodily fluids or hazardous chemicals, but there are many instances where hand washing alone is sufficient (such as when moving patients), and whilst hand washing is required before and after glove use, overuse of gloves wastes resources. We have modelled the environmental impact of rationalising glove use as personal protective equipment (PPE) in healthcare settings, finding this could reduce carbon footprint of PPE by ≤ 45% (Rizan et al. 2021a). Previous LCA analyses indicate carbon footprint can be reduced when switching a variety of items of equipment used in the operating theatre from single-use to reusables, including surgical scissors (Ibbotson et al. 2013), laryngoscopes (Sherman et al. 2018), laryngeal mask airways (Eckelman et al. 2012), peri-operative linens, (including surgical gowns and drapes) (Overcash 2012), and laparotomy pads (Kummerer et al. 1996). However, contrasting findings were reported in a study comparing six reusable instrument sets used for spinal fusion surgery (each containing multiple instruments, weighing 45 kg in total) versus two much smaller single-use instrument sets (2 kg total) containing just a few instruments (Leiden et al. 2020). It is likely that development of a consolidated reusable set (containing similarly few instruments) would confer a lower carbon footprint. Other notable exceptions include several LCA studies conducted in Australia which found that the carbon footprint of a single-use ureteroscope was similar to reusable equivalents (Davis et al. 2018), and the carbon footprints of single-use central venous catheter kits (McGain et al. 2012) and anaesthetic equipment (McGain et al. 2017) were lower than of reusable equivalents. Australian electricity uses predominantly coal-based non-renewable energy sources, and where these studies remodelled processes using European and USA energy sources, the carbon footprint of reusables was lower (McGain et al. 2012, 2017).
The majority of evidence supports lower carbon footprints associated with using reusable surgical equipment instead of single-use (Drew et al. 2021), but where it is not possible to switch to fully reusable equipment, an alternative is to use hybrid equipment (alternatively termed ‘modular systems’; or ‘Resposables™’) which in this context refers to items which are mainly reusable, with a small single-use component. An LCA of laparoscopic instruments indicated that switching from single-use to hybrid equivalents reduced the environmental impact across 17 out of 18 categories by a mean average of 60%, with projected cost savings of £11 million if adopted for all laparoscopic cholecystectomies (Rizan and Bhutta 2021). Where items marketed as ‘single-use’ cannot be avoided, it is possible to gain an additional use through reprocessing (also known as remanufacturing), involving decontamination, testing, and repairing, after which they are re-sold and intended to be used just once again. LCA studies have demonstrated reductions in carbon footprint associated with use of reprocessing single-use medical devices compared with purchasing new equivalents across a range of products including endoscopic trocars, deep vein thrombosis compression devices, pulse oximeters, scissor tips, arthroscopic shavers, diathermy clips, ultrasonic scalpels (Unger and Landis 2016), and cardiac electrophysiology catheters (Schulte et al. 2021), with 45% (Schulte et al. 2021)–50% (Unger and Landis 2016) reductions in cost. Finally, it is possible to extend use of materials within either single-use or reusable surgical equipment at the end of their functional life through recycling, resulting in a 50-fold reduction in the carbon footprint of the waste component of a product’s lifecycle when compared with high temperature incineration (Rizan et al. 2021b). Recycling stainless steel surgical instruments into surgical instrument mesh baskets has been shown to be both feasible and cost-effective (van Straten et al. 2021).
Repair is another mechanism that can be used to extend the lifespan of surgical equipment already in circulation, and which may result in net reduction in resource use. The importance of maintenance and repair of surgical instruments has previously been emphasised in resource-poor settings, where maximising lifespan of devices is necessary due to difficulty in obtaining and funding replacements (Haddad and Worst 2002; Munakomi et al. 2018). The reduction in environmental impact associated with repair instead of replacement has been demonstrated in other contexts, for example for household electric and electronic items (Bovea et al. 2020) to vehicles (Wursthorn et al. 2010), but has not previously been evaluated for surgical equipment. Maintenance and repair are especially important for items such as surgical instruments because intra-operative failure or instrument breakage impacts on the safety of care. Poor quality instruments have been associated with patient safety incidents (Dominguez and Rocos 2019), whilst repair of instruments was associated with reduced rates of surgical site infections in caesarean sections (Stutler et al. 2013).
Common problems with surgical instruments amenable to repair include sharpness (e.g. cutting edges of scissors, osteotomes, levers, scrapers), setting issues (e.g. misalignment and/or ratchet defects of needle holders, artery forceps, tissue forceps), and missing components (e.g. screws). In the UK, very few hospitals have surgical instrument repair centres onsite, and repair is more commonly provided offsite by a small number of external contractors which typically receive instruments from across the country. We are aware of only five such companies in the UK, which either contract directly with hospital sites or subcontract through industry partners. Alternatively, repair may be performed by instrument manufacturers, or end users (Medicines and Healthcare products Regulatory Agency 2021).
The benefits of repairing surgical instruments include potential cost savings (Munakomi et al. 2018) and improved safety including reduced surgical site infection rates (Stutler et al. 2013). However, the environmental impact of repairing reusable equipment has not previously been evaluated in a surgical context, and financial implications have not been formally analysed. In this study, we use LCA methods and life cycle costing to estimate environmental and financial impact of repairing reusable surgical scissors. Our data showed that general surgical scissors were the most commonly repaired instrument at our study site (comprising 52% of all surgical instruments repaired at the Royal London Hospital, UK, between 2008 and 2019; Supplementary Table 1). Examples of general surgical scissors which are commonly used across a variety of surgical specialties include Mayo, McIndoe, and Metzenbaum (each can be curved or straight), and 17-cm straight Mayo scissors were pragmatically chosen for this study following discussion with two surgical instrument manufacturers who both indicate that these scissors held the highest volume sales.
The primary objective of this study was to evaluate the environmental impact and financial cost of repairing surgical scissors, comparing onsite versus offsite repair. The secondary objective was to model alternative scenarios to determine the generalisability of findings, including altering the number of uses of scissors, number of repairs, and distance to offsite repair centre, and alternative electricity sources and waste handling processes.
2 Methods
2.1 Life cycle assessment of reusable surgical scissors and repair
An LCA was conducted using ISO 14040/14044 guidelines (International Organization for Standardization 2006a, 2006b), and modelled using SimaPro Version 9.10 (PRé Sustainability, Amersfoort, Netherlands). The Ecoinvent database (version 3.6) was used for all processes aside from production of steam, which was modelled using the European Life Cycle Database. Three base scenarios were modelled for reusable scissors: (1) no repair, (2) onsite repair, and (3) offsite repair.
2.1.1 Functional unit
The functional unit chosen was one use of a 17-cm, straight Mayo reusable surgical scissor (the term ‘use’ is used in this study to refer to the scissors being used for a single surgical procedure), manufactured in Germany and supplied by Ream Surgical Ltd. (Dartford, UK; AS1116017).
In determining the reference flows (amount of products and processes required to fulfil this functional unit), the following assumptions were made: that scissors were used for 40 surgical procedures before disposal or repair was required; that each repair would provide a further 40 uses; and that scissors could be repaired up to nine times before disposal (giving total 400 uses of scissors repaired nine times). These assumptions were based upon the experience of co-author TB (lead technologist at the Royal London Hospital) and expert opinion (surgical instrument industry personnel, and staff at the Royal Sussex County Hospital sterilisation services department). The LCA inventory was built based upon 400 uses of surgical scissors as this was the lowest common denominator across scenarios using these reference flows, and all results were reported based upon one use of a pair of scissors in a single surgical procedure. Providing 400 uses of surgical scissors could be achieved through using one reusable scissor replaced nine times (total ten scissors, used 40 times each, no repair); or one reusable scissor repaired nine times (enabling 400 uses for an individual reusable scissor), with repair either onsite at the hospital or offsite with an external contractor. Scissors must be decontaminated before each use, and so 400 uses of scissors required 400 decontaminations. An additional decontamination cycle was required after repair work (Working Group Instrument Reprocessing 2017), and so 400 uses of scissors repaired nine times required a total of 409 decontaminations.
2.1.2 System boundary
This was a ‘cradle-to-grave’ analysis, starting with raw material extraction and manufacture of materials used within the scissors and their primary and secondary packaging (Fig. 1). The manufacture of scissors themselves was included, alongside transport associated with distributing the packaged scissors from the manufacturing site to the hospital. We included energy and materials used by decontamination and repair machines (used for grinding and buffing), and transportation to the offsite repair site. We also included raw material extraction and production of materials within packaging involved in the decontamination and repair processes, alongside transport of such raw materials to the packaging manufacturer. We accounted for waste disposal of all items used throughout the life cycle. Emissions to air and water were included for all processes where these were built into the life cycle inventory database. Capital goods and building infrastructure were excluded for both the decontamination and repair site.
2.1.3 Life cycle inventory
Parameters for the manufacture and distribution of surgical scissors are outlined in Table 1. For each included material, we used manufacturer information to determine the material composition, or expert knowledge where such information was not available. Each component was weighed using precision balance scales (Fisherbrand FPRS4202, Fisher Scientific, Loughborough, UK). The inventory was developed through matching these materials with closest materials included within the Ecoinvent database (materials and processes selected are outlined in Supplementary Table 2), which provided material specific global average values associated with the raw material extraction, production, and transport to the ‘end user’ (in this case the manufacturer).
Manufacture of scissors was modelled using Ecoinvent data, which includes global average energy and auxiliary inputs for the metal working factory, metal working machine, construction of the metal working factory, manufacture of the metal working machine, and chromium steel lost within the process. We adapted Ecoinvent data on chromium steel production in Europe to German specific electricity, water, and natural gas sources.
We modelled transportation of scissors from the site of raw material extraction to the distributor based on the locations and mode of travel specified by the supplier (Table 1), with travel distances estimated using the online Pier2Pier tool (Pier2Pier 2020). For road travel, the first and last 8 km was assumed to be via courier, and the remaining distance via heavy goods vehicles. The distance between both the distributor and hospital, and between offsite repair site and the hospital was assumed to be 80 km.
Scissors were assumed to be integrated into a reusable instrument set alongside other instruments (instrument weight totalling 2 kg), with the set contained within single-use tray wrap. Reusable scissors were decontaminated at the hospital site before each use, including the first use as scissors were not sterilised by the manufacturer. Energy and material inputs for decontamination of reusable equipment were modelled using our own data published elsewhere (Rizan et al. 2022) (Supplementary Table 3), with environmental impact of decontaminating scissors allocated according to weight (65.67 g scissor, within a set containing 2 kg of instruments).
The repair of reusable scissors was modelled based upon onsite repair at The Royal London Hospital (London, UK), and offsite repair at Ream Surgical (Dartford, UK). The repair process is summarised in Supplementary Fig. 1. Materials and inputs were determined through direct observation and discussion with repair site personnel (Table 2). Electricity consumption of repair equipment was estimated using the power rating (highest power allowed to flow through the device) and the duration of use. This method potentially overestimates electricity consumption but would have negligible impact on results because electricity was responsible for only a small proportion of the overall environmental impact of the repair process itself. All waste was assumed to be disposed of via high temperature incineration.
2.1.4 Life cycle impact assessment
We used characterization factors within the World ReCiPe Midpoint Hierarchist method (Version 1.1) to characterise emissions from the lifecycle inventory assessment and combine these into midpoint impact categories. Our primary outcome was global warming impact, with total greenhouse gases summated and expressed as carbon dioxide equivalents (CO2e), so providing a ‘carbon footprint’. Seventeen additional midpoint impact categories were considered within the ‘scope’ of the LCA: stratospheric ozone depletion, ionising radiation, ozone formation (on human health and terrestrial ecosystems), fine particulate matter formation, terrestrial acidification, eutrophication (freshwater and marine), ecotoxicity (terrestrial, freshwater, marine), toxicity (human carcinogenic, human non-carcinogenic), land use, resource scarcity (mineral and fossil), and water consumption. We weighted the results using aggregated midpoint impact categories via the ReCiPe Endpoint Hierarchist method (Version 1.1) to provide endpoint estimates for damage to human health, the natural environment, and resource scarcity. Midpoint and endpoint results were normalised using Hierarchist normalisation factors, providing mean average contributions to each of those impacts with respect to a global average person’s daily routine activity (Sleeswijk et al. 2008).
2.1.5 Sensitivity analysis
To evaluate the generalisability of our findings, we modelled eight alternative scenarios, changing just one parameter in each scenario.
-
1.
Scenario 1 modelled the impact of reducing the number of reuses of scissors to 10, since in practice some reusable scissors may be used or repaired less often, for example due to scissors being lost, damaged beyond repair, or placed on infrequently used instrument sets.
-
2.
Scenario 2 modelled the impact of increasing the number of reuses of scissors to 400.
-
3.
Scenario 3 assumed that scissors were repaired just once before disposal and replacement.
-
4.
Scenario 4 examined the impact of increasing the distance from the hospital to offsite repair centre from 80 to 800 km, assuming this was fulfilled by heavy goods vehicle, with the first and last 8 km assumed to be via courier.
-
5.
Scenario 5 modelled the impact of decontaminating reusable scissors using an Australian source of electricity, which has a high proportion of electricity sourced from fossil fuels.
-
6.
Scenario 6 assumed that all waste was recycled. Here we applied the open-loop ‘recycled content method’, which allocates emissions and environmental impacts associated with the recycling process and net reduction of virgin material acquisition to the production of the recycled goods (World Resources Institute 2011). For example where the construction industry uses stainless steel sourced from recycled surgical scissors, the reduced requirement for raw materials is assigned to the constructed building.
-
7.
Scenario 7 assumed enhanced waste segregation, with sharps waste (scissors) sent for high temperature incineration (as per base model), cardboard and paper sent for recycling, and all other waste sent to landfill.
-
8.
Scenario 8 was the same as 7 but with ‘other’ waste sent for municipal (low temperature) incineration. Alternative waste handling processes are outlined in Supplementary Table 4.
2.2 Life cycle financial cost of reusable surgical scissors and repair
The purchase cost of the reusable scissors indicated by the supplier was used as the cost of manufacture and distribution. Cost of decontamination was based on the rate charged by our local sterilisation services department (GBP £25.53 per reusable instrument set), apportioned according to the weight of reusable scissors (65.67 g/2 kg). The cost of repairing a pair of scissors was based on information provided by repair sites. End of life waste disposal was assumed to be £617 per tonne, based on the average price of clinical waste incineration in the UK (NHS Digital 2020).
3 Results
3.1 Environmental impact of repairing surgical scissors
3.1.1 Base scenario midpoint and endpoint environmental impact assessment results
The carbon footprint of using a pair of reusable scissors once was 70.3 g CO2e/use, assuming scissors were replaced with new reusable scissors after 40 uses. This was reduced by 20% through use of onsite repair every 40 uses instead of replacement (56.3 g CO2e/use), and by 19% for offsite repair (57.0 g CO2e/use). Reusable scissors repaired offsite were associated with reductions (when compared with no repair) across all 18 midpoint environmental impact categories (Table 3), with mean average reductions across categories of 30% relative to no repair (range: 2% for marine eutrophication to 73% for mineral resource scarcity). There were notable reductions through use of offsite repair (compared with no repair) in mineral resource scarcity, marine ecotoxicity, freshwater ecotoxicity, and fine particulate matter, with the difference driven mainly by use of ferronickel (for all four impact categories), and ferrochromium (for fine particulate matter generation) within the manufacture of chromium steel for replacement scissors (Supplementary Figs. 2, 3, 4 and 5). Notable reductions were also seen in human carcinogenic impacts through use of scissors that were repaired offsite, as this reduced the need for manufacture of chromium steel, with human carcinogenic impacts driven by the generation of dust by furnaces used in the steelmaking process and treatment of associated waste (Supplementary Fig. 6).
There were small additional reductions associated with onsite repair, with a mean additional reduction in environmental impact (compared with offsite repair) of 1.6% across impact categories (range: 0.1% for marine eutrophication to 2.4% for land use). The reduction in land use and carbon footprint associated with switching from offsite to onsite repair was driven by differences in quantity of paper and low-density polyethylene respectively used within packaging used to send scissors for repair. Scissors were individually packaged when sent for offsite repair, whilst bulk packaging across multiple scissors was used where repair was conducted onsite.
Normalised results (Supplementary Table 5) indicated that the carbon footprint of using a pair of reusable scissors once (no repair) equated to the GHG emissions generated in around 4 min and 38 s by a global average person, whilst switching to a pair that undergoes repair instead of replacement saves the equivalent of around 1 min of a global average person’s GHG emissions. The impact of using scissors (no repair) relative to a global average person’s environmental impact was greatest for freshwater ecotoxicity (equating to equivalent impact generated in 14 h by a global average person), human carcinogenic toxicity (15 h), and marine ecotoxicity (23 h), whilst repair reduced these impacts to 8, 7, and 13 h respectively (Supplementary Fig. 7).
Total damage to human health from one use of reusable scissors (no repair) was 1.46e−7 DALYs (disability adjusted life years) equating to five disability adjusted life seconds (endpoint environmental impact results: Table 4). The impact on ecosystems was 3.12e−10 species.year (loss of local species per year), and the impact on resource depletion equated to US $ 0.007 (GBP £0.0059, all currency conversions based upon exchange rate 13th December 2021) involved in future mineral and fossil resource extraction. These three endpoint environmental impacts were reduced by 32%, 19%, and 8% respectively through use of scissors repaired offsite, whilst those that were repaired onsite were associated with a further 1–2% reduction across the three endpoint categories relative to offsite repair. Normalised endpoint results indicated that use of surgical scissors had greatest impact on the human health endpoint impact category across all base scenarios, relative to activities of a global average person (Supplementary Table 6).
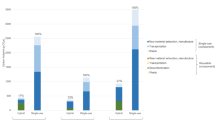
3.1.2 Base scenarios process contributions
Figure 2 provides a breakdown of processes contributing to the carbon footprint of one use of surgical scissors, and Supplementary Figs. 8, 9, and 10 demonstrate the drivers of the carbon footprint of each baseline scenario in more detail. Decontamination was the largest contributor to the carbon footprint, whether the reusable scissors were repaired or not. For non-repaired reusable scissors, decontamination constituted the majority of the carbon footprint (76%, 53 g CO2e/use). The carbon footprint of decontamination increased to 54 g CO2e/use for those repaired either offsite (95% of impact) or onsite (97%), as the scissors required decontamination both before and after repair, although this was apportioned across the additional uses afforded by repair. The impact of repair was 1.5% of the total carbon footprint of scissors for those repaired offsite (0.9 g CO2e/use, which included associated transport associated with offsite repair), and 0.4% of the total for scissors repaired onsite (0.2 g CO2e/use). The carbon footprint of raw material extraction, manufacture, packaging, transportation, and waste (in relation to scissors) totalled 17 g CO2e/use for reusable scissors which were not repaired, and use of repair instead of replacement reduced this by 90% (2 g CO2e/use).
Contribution of processes to carbon footprint of one use of surgical scissors. Legend: Stainless steel: raw material extraction of stainless steel; manufacturing: production of surgical scissor from stainless steel; packaging: primary and secondary packaging of scissors; transportation: transport from raw material extraction through to delivery of scissors to hospital; decontamination: washing, followed by steam sterilisation within single-use tray wrap; repair: processes involved in repair including associated packaging and transportation; waste: high temperature incineration of all waste throughout life cycle
Analysis of the repair process itself indicated that where this was conducted offsite, the majority of GHGs generated were associated with use of low-density polyethylene (62%) and paper (14%) relating mainly to packaging (Supplementary Fig. 11), whilst use of bulk packaging at the onsite repair site reduced the relative contributions of these to 39% and 9% respectively (Supplementary Fig. 12).
3.1.3 Sensitivity analysis
Within each of the eight alternative scenario models, the carbon footprint was highest for non-repaired scissors and lowest for those repaired onsite (Fig. 3). Similar patterns were seen across all other midpoint environmental impacts (Supplementary Tables 7A-C) with highest impact where scissors were not repaired and lowest where they were repaired onsite. This indicates that environmental impact reductions associated with repair were robust to alternative scenario analysis.
Scenario modelling. Legend: Waste segregation (scenario 7): sharps waste (scissors) sent for high-temperature incineration, cardboard and paper sent for recycling, and all other waste sent to landfill. Waste segregation (scenario 8): sharps waste (scissors) sent for high-temperature incineration, cardboard and paper sent for recycling, and all other waste sent to municipal incineration. CO2e, carbon dioxide equivalents
Across all scenarios, the highest carbon footprint was associated with scissors which were only used ten times and were not repaired (122 g CO2e/use; Scenario 1), whilst the lowest carbon footprint was associated with scissors which were used 400 times before repair onsite (53.5 g CO2e/use; Scenario 2). The carbon footprint of scissors which were not repaired but which were used 400 times (54.9 g CO2e/use) was only marginally greater than of those that were repaired (narrowing the gap between those that are repaired onsite versus offsite to 52.5 and 53.6 g CO2e/use respectively), indicating the number of uses is an important factor. Where scissors were repaired only once (either on or offsite), this resulted in an 11% carbon reduction compared with no repair (Scenario 3). Increasing the distance between the hospital and offsite repair centre (from 80 to 800 km; Scenario 4) made very little difference to the results. However, modelling Australian electricity for the decontamination impact significantly increased the carbon footprint, to the extent that using a reusable surgical scissor which underwent repair but was decontaminated in Australia (Scenario 5) had a greater carbon footprint than using one which was not repaired in the UK (baseline scenario). The only alternative waste scenario which had an impact of > 1% was recycling of all waste, and in turn this only had an impact where scissors were not repaired (Scenario 6).
3.2 Life cycle cost of repairing surgical scissors
The financial cost of purchasing a new pair of reusable scissors was GBP £23.45, and decontaminating these costs GBP £0.84 per pair, with small additional cost of disposal at the end of the functional life (GBP £0.05 per pair). The cost to repair scissors offsite was GBP £2.20, whilst onsite repair costs GBP £2.50. The cost of repair was significantly cheaper (89–91% for onsite and offsite repair respectively) than of purchasing a new pair of scissors. The life cycle cost per use for reusable scissors (GBP £1.43) was reduced by 32% when repaired, with marginally lower life cycle costs for offsite repair (GBP £0.965) compared with onsite repair (GBP £0.972) (Table 5).
4 Discussion
This study is the first to evaluate the environmental impact and cost of repairing surgical equipment. Here we found that using surgical scissors that had undergone repair reduced the carbon footprint by around one-fifth, and the financial cost by approximately one-third (summary of findings; Fig. 4), meeting our primary objective. Repairing scissors once achieved an 11% reduction in carbon footprint and 15% lower financial cost relative to replacing these with a new pair, indicating over half of the carbon and financial reductions associated with repair as modelled in our baseline scenario could be achieved through a single repair. We compared offsite versus onsite repair, and found that surprisingly this did not make a significant impact to the carbon footprint, but found that factors relating to decontamination and number of uses across the reusable scissors’ lifespan were important determinants of the carbon footprint.
The value of the global surgical scissors market was estimated at US $ 331 million (GBP £250 million) in 2019, of which approximately two-thirds were reusable and one-third single-use (Allied Market Research 2020). Assuming our purchase cost and use profile are representative and that the rate at which new scissors were purchased was equal to the rate at which they were disposed of (with no change in stock levels), we estimate that there are around 364 million uses of reusable scissors each year. Repairing these scissors at offsite centres would save approximately 4847 tonnes CO2e (equivalent to flying as a passenger from London to New York return around 2000 times) (Department for Environment, Food and Rural Affairs/ Department for Business, Energy & Industrial Strategy 2019) and around GBP £166 million each year. Previous research from three hospitals in the Netherlands found one-sixth of single-use and disposable stainless steel instruments destined for waste could potentially be refurbished, and that repairing or remanufacturing instead of purchasing new items saved almost € 39,000 (GBP £33,190) (van Straten et al. 2021).
The secondary objective of this study was to model alternative scenarios, and here we found the reduction in environmental impact associated with repair was robust to reducing number of reuses, reducing number of repairs, increasing the distance to offsite repair site, and using an electricity supply with lower proportion of renewables (Australian) for the decontamination process. Increasing the number of uses of scissors from 40 to 400 times before disposal reduced the carbon footprint by a similar proportion (around one-fifth) to reductions associated with repairing those used 40 times. It is therefore important to maximise the number of instrument uses between repair and before disposal. The barriers, enablers, and carbon footprint implication of extending the number of uses of surgical instruments across their lifetime are an important area of future research. Extending instrument lifetime may be facilitated by improving robustness at design stage, developing objective measures to evaluate functional failure, and proactive maintenance.
We found that decontamination made the biggest contribution to the carbon footprint across all baseline scenarios, ranging from three-quarters of the carbon footprint of scissors which were not repaired up to almost all (95–97%) of the carbon footprint of repaired scissors. Our own analysis published elsewhere found that the carbon footprint of decontamination and packaging of reusable instruments can be optimised through preparing instruments as part of a set (rather than individually wrapped items), optimising decontamination machine loading (number of instruments per machine slot), and recycling of associated packaging (Rizan et al. 2022). Adopting these strategies would reduce the carbon footprint of the decontamination phase by around one-third across all three base scenarios in the current study, resulting in similar carbon savings across the scissor life cycle to those associated with adopting repair. The importance of the proportion of renewable energy on the carbon footprint of medical equipment has previously been emphasised, including in studies of central venous catheter insertion kits (McGain et al. 2012) and of anaesthetic equipment (McGain et al. 2017), where modelling electricity from different regions was sufficient to change conclusions in relation to carbon footprint of single-use versus reusable equivalents. In the current study, we found that use of Australian electricity for the decontamination process increased the carbon footprint of the reusable scissors by around one-third (when not repaired). Our previous study also found using low carbon (Icelandic) energy in combination with the other strategies could reduce the carbon footprint of decontamination further (Rizan et al. 2022).
A previous study by Ibbotson et al. (2013) evaluated the carbon footprint of reusable scissors, assuming that these were repaired every 750 uses (repaired a total of five times, providing 4500 uses across the scissor life cycle). This contrasts with our own model in which we assumed that repair was required every 40 uses, and that repair was undertaken nine times, totalling 400 uses across the scissor lifespan. Our more conservative use profile assumptions are aligned with a study using radio frequency identification for tracking, which indicated that Cooper scissors were used 10–120 times before instrument failure (which included the need for repair) (Yoshikawa et al. 2019). Ibbotson et al. (2013) included the cost of repair within their analysis and assumed this was 75% of the cost of purchasing a new pair of scissors, whilst the current study uses primary data based on amount charged by two repair centres. The study by Ibbotson et al. (2013) did not evaluate the carbon footprint of repair itself and, unlike the current study, made no comparison to scenarios in which scissors were replaced instead of repaired. Instead, the study evaluated the impact of switching from single-use surgical scissors to reusable equivalents, and whilst figures were not reported directly, these can be estimated from a graph indicating the carbon footprint reduced roughly one 100–fold, from around 2200 g CO2e/use for single-use scissors to around 66 g CO2e/use for reusable scissors (including repair) (Ibbotson et al. 2013). The large difference in carbon footprint of single-use versus reusable surgical scissors found here relates to the increased requirements for raw material extraction, manufacture, distribution, and waste associated with the single-use scissors. The figure derived by Ibbotson et al. (2013) for reusable scissors was similar to our own baseline scenario estimates (56–70 g CO2e), although difficulty in interpreting the graph limits the extent to which the carbon footprint estimated for reusable scissors can be compared to our own.
Evidence from Ibbotson et al. (2013) points to significant differences in carbon footprint associated with switching single-use to reusable scissors (estimated at around 33-fold), and this is supported by studies of other equipment used in the operating theatre; for example, 16–18-fold reductions have been associated with switching single-use to reusable laryngoscope handles (Sherman et al. 2018). The reductions associated with switching from single-use to reusable medical equipment are likely greater than remanufacturing single-use equipment, with previous LCA research finding that remanufacturing single-use electrophysiology catheters halved the carbon footprint when compared with purchasing new single-use items (Schulte et al. 2021). It is important that the principle of reduce and reuse is prioritised, and the switch to reusable alternatives should be particularly encouraged in settings where single-use equipment is commonly used including emergency department, outpatient, and primary care settings. Once reusables are in place, strategies for further reductions in carbon footprint may then include repair, optimising decontamination (Rizan et al. 2022), and recycling (Rizan et al. 2021b). Comparing environmental impact of different strategies from across different products and author groups should be considered with caution, and a direct comparison of different approaches (e.g. remanufacture of single-use items, switching to reusables, repairing reusables) would be a useful area of future research.
Maintenance and repair services have been established in low-resource settings such as public hospitals in Honduras to meet demand for safe surgical instruments in the absence of resources to fund new equipment (Fitzgerald and Bhutta 2018). However, in high-income nations repair services are anecdotally under-utilised, resulting in premature obsolescence. To increase rates of repair, health facilities need to establish and expand repair contracts, and raise awareness of repair services amongst theatre and sterilisation services staff. To determine the scope for repair of instruments beyond surgical scissors, we retrospectively examined a dataset of all instrument repairs conducted over an 11-year period (February 2008–February 2019) at an onsite repair centre (The Royal London Hospital), finding most commonly repaired instruments were general surgical scissors, osteotomes, needle holders, retractors, and clamps (Supplementary Table 7). This highlights the feasibility of repair across a range of commonly used surgical instruments, although the environmental impact of such repair relative to purchasing new instruments will depend upon packaging and equipment required for repair, alongside decontamination processes.
We found similar reductions in carbon footprint and financial cost associated with both onsite versus offsite repair, indicating that the important message is that reusable scissors are sent for repair, whether that is onsite at the hospital or offsite with an external contractor. The carbon footprint of transporting the scissors for repair offsite was minimal, even where an 800 km journey to the repair centre was factored in (Scenario 4), although this was modelled using data on average couriers and heavy goods vehicles, and so the exact contribution would depend on how efficiently these are loaded. There were other minor differences in the processes used for repair onsite versus offsite such as use of bulk packaging when scissors were repaired onsite, and use of different materials to test scissor sharpness. Three-quarters of the GHGs associated with the offsite repair process itself were attributed to use of low-density polyethylene and paper predominantly within packaging, and use of bulk packaging or reusing packaging could significantly reduce the environmental impact of the repair process itself.
However, onsite repair may offer faster turnaround times, which may be especially important for instruments used frequently. We extracted data on the time delay between batches of instruments being sent for repair and them being returned and ready for use, using a smaller, more detailed and informative dataset for onsite repair between July 2018 and March 2019 at The Royal London hospital, and for offsite repair at the Royal Sussex County Hospital (RSCH) between January 2018 and January 2019 (missing data were excluded from analysis). The results show that the mean average turnaround time was 3.6 days (range 1–28 days) for onsite repair, and 31.6 days for offsite repair (range 9–57 days). However, offsite repair potentially offers the ability to repair more complex instruments (such as electrosurgical and endoscopic items) requiring more specialist equipment and expertise. For example, we found that the onsite repair centre at The Royal London Hospital sent a number of instruments for external repair, of which 36% were endoscopic scopes, 21% were needle holders, and 10% were endoscopic instruments. Encouraging uptake of offsite repair centres is likely more feasible than individual hospitals creating repair services, and purchase or loan of spare equipment can be used to minimise disruption (loan is already offered by some repair companies) (Medicines and Healthcare products Regulatory Agency 2021).
Data from the Royal London hospital show that of instruments considered irreparable, 46% was due to normal expected wear, 30% due to damage by external force (incorrect use), and 21% due to corrosion (which typically results from prolonged contact with bodily fluids such as blood, due to delays between the operation and decontamination), and 2% of those ‘irreparable’ were not repaired at the time due to insufficient decontamination. Damage may also arise due to impurities in water, use of incompatible chemicals, inadequate drying, and improper care when loading instruments for decontamination (Working Group Instrument Reprocessing 2017). Attempts to provide repair services for instruments must therefore be aligned with education to minimise avoidable instrument damage (including correct handling, decontamination processes, and instrument maintenance) and proactive onsite quality checking to identify damaged or sub-optimally performing instruments.
We also recognise additional harms from a model reliant on single-use surgical instruments, where cost pressures mean the majority of such scissors are produced in low-resource environments such as the surgical instrument manufacturing cluster in Sialkot, Pakistan. In such settings, workers suffer poor remuneration, and are exposed to risk of injury, noise-induced hearing loss, and inhalation of metal dust (Bhutta 2006; Swedwatch 2015; Junaid et al. 2016).
4.1 Limitations
As with all life cycle assessments, there were sources of uncertainty limiting the reliability and generalisability of findings. Parameter uncertainty refers to the extent to which the life cycle inventory (built upon activity data only here, as no direct emissions data were collected) and characterisation factors (embedded within SimaPro Version 9.10) truly reflect the environmental impact of the product under investigation (World Resources Institute 2011). We sought to use primary process activity data wherever possible throughout the product life cycle but were unable to obtain reliable primary data on the manufacture of surgical scissors from stainless steel, and instead used global average data embedded within Ecoinvent for production of chromium steel and metal working. Whilst this limits the specificity of our results in relation to the case study pair of scissors, this approach improves generalisability of findings through use of global average data aggregated from multiple sources. In general, the sample size of primary activity data was generally limited to ‘one’ within this study, so we did not perform formal parameter uncertainty analysis (through Monte Carlo approach, or via a pedigree approach) as it is not recommended in such instances (Heijungs 2020).
Our findings were limited by a number of methodological choices, resulting in scenario uncertainty (International Organization for Standardization 2006 A). For example, there was risk of truncation error whereby the results reported underestimate the true environmental impact due to the system boundary chosen (World Resources Institute 2013), although this was minimised through including all processes reaching the threshold of significance (World Resources Institute 2011) which we defined a priori as those likely to contribute ≥ 1% impact. We sought to evaluate the impact of key methodological assumptions through formal sensitivity analysis (International Organization for Standardization 2006 A) and finding conclusions were robust to alternative scenarios improved generalisability of results to other settings. Nevertheless, results are specific to the goal and scope of this study which focused on surgical scissors, and whilst findings may extend to other simple stainless steel instruments such as needle holders and forceps, we acknowledge that repair of complex equipment such as electrosurgical or endoscopic equipment may associate with greater environmental burden.
5 Conclusion
The environmental impact of repairing equipment instead of buying new items has previously been evaluated in other contexts (Wursthorn et al. 2010; Bovea et al. 2020), but this study is the first to explore the role of repair within a healthcare setting. Here we focused on surgical scissors, finding that repairing these at the end of their functional life instead of replacing them with a new pair can reduce environmental and financial cost. We found minimal difference in environmental impact and financial cost associated with onsite and offsite repair centres, indicating that development of regional or national repair centres is as good a strategy as developing local repair centres.
When surgical equipment fails, it is usually disposed of, and so education amongst equipment users (such as theatre staff) and those involved in processing (such as sterilisation personnel) will be important when introducing and expanding repair contracts. We found that decontamination was responsible for almost all of the carbon footprint of repaired scissors, and to reduce the environmental impact of repaired items further, it is important to optimise the decontamination process (Rizan et al. 2022). Repair has the potential to play an important role in mitigating environmental impacts of medical equipment, but the extent to which this applies across other medical equipment requires further research.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Allied Market Research (2020) Surgical scissors market by type (reusable surgical scissors and disposable surgical scissors), application (orthopedics, cardiology, neurology, oral and throat, gastroenterology, dermatology, and others), and end user (hospitals, ambulatory surgical centers, and others): global opportunity analysis and industry forecast, 2019–2027. https://www.alliedmarketresearch.com/surgical-scissors-market. Accessed 1 Oct 2021
Asthana S, Gibson A (2021) Averting a public health crisis in England’s coastal communities: a call for public health research and policy. J Public Health. Online ahead of print. https://academic.oup.com/jpubhealth/advance-article/doi/10.1093/pubmed/fdab130/6274872. Accessed 18 Nov 2021. https://doi.org/10.1093/pubmed/fdab130
Bhutta MF (2006) (2006) Fair trade for surgical instruments. BMJ 333(7562):297–299. https://doi.org/10.1136/bmj.38901.619074.55
Bovea MD, Ibáñez-Forés V, Pérez-Belis V (2020) Repair vs. replacement: selection of the best end-of-life scenario for small household electric and electronic equipment based on life cycle assessment. J Environ Manage 254:109679. https://doi.org/10.1016/j.jenvman.2019.109679
Davis NF, McGrath S, Quinlan M, Jack G, Lawrentschuk N, Bolton DM (2018) Carbon footprint in flexible ureteroscopy: a comparative study on the environmental impact of reusable and single-use ureteroscopes. J Endourol 32(3):214–217. https://doi.org/10.1089/end.2018.0001
Department for Environment, Food and Rural Affairs/ Department for Business, Energy & Industrial Strategy (2019) UK Government GHG Conversion Factors for Company Reporting. https://www.gov.uk/government/publications/greenhouse-gas-reporting-conversion-factors-2019. Accessed 13 Aug 2020
Dominguez ED, Rocos B (2019) Patient safety incidents caused by poor quality surgical instruments. Cureus 11(6):e4877. https://doi.org/10.7759/cureus.4877
Drew J, Christie SD, Tyedmers P, Smith-Forrester J, Rainham D (2021) Operating in a climate crisis: a state-of-the-science review of life cycle assessment within surgical and anesthetic care. Environ Health Perspect 129(7):76001. https://doi.org/10.1289/EHP8666
Eckelman M, Mosher M, Gonzalez A, Sherman J (2012) Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth Analg 114(5):1067–1072. https://doi.org/10.1213/ANE.0b013e31824f6959
Eckelman MJ, Sherman J (2016) Environmental impacts of the U.S. health care system and effects on public health. PLoS One 11(6):e0157014. https://doi.org/10.1371/journal.pone.0157014
Fitzgerald E, Bhutta M (2018) Tooling up. The Bulletin of the Royal College of Surgeons of England 100(6):269–270. https://doi.org/10.1308/rcsbull.2018.269
Haddad D, Worst JG (2002) The maintenance and repair of ophthalmic surgical instruments: training at the eye clinic. Commun Eye Health 15(44):60–1. PMCID: PMC1705877
Heijungs R (2020) On the number of Monte Carlo runs in comparative probabilistic LCA. Int J Life Cycle Assess 25:394–402. https://doi.org/10.1007/s11367-019-01698-4
Ibbotson S, Dettmer T, Kara S, Herrmann C (2013) Eco-efficiency of disposable and reusable surgical instruments- a scissors case. Int J Life Cycle Assess 18:1137–1148. https://doi.org/10.1007/s11367-013-0547-7
IPCC (2021) Climate change 2021: the physical science basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [Masson-Delmotte 2021 A. Pirani, S.L. Connors, C. Péan, S. Berger, N. Caud, Y. Chen, L. Goldfarb, M.I. Gomis, M. Huang, K. Leitzell, E. Lonnoy, J.B.R. Matthews, T.K. Maycock, T. Waterfield, O. Yelekçi, R. Yu, and B. Zhou (eds.)). Cambridge University Press. In Press. https://www.ipcc.ch/report/ar6/wg1/. Accessed 18 Nov 2021
International Organization for Standardization (2006a) ISO 14040:2006 Environmental management — life cycle assessment — principles and framework. https://www.iso.org/standard/37456.html. Accessed 13 April 2021
International Organization for Standardization (2006b) ISO 14044:2006 Environmental management — life cycle assessment requirements and guidelines. https://www.iso.org/standard/38498.html. Accessed 13 April 2021
Kummerer K, Dettenkofer M, Scherrer M (1996b) Comparison of reusable and disposable laparotomy pads. Int J Life Cycle Assess 1(2):67–73. https://doi.org/10.1007/BF02978647
Junaid M, Hashmi MZ, Malik RN (2016) Evaluating levels and health risk of heavy metals in exposed workers from surgical instrument manufacturing industries of Sialkot. Pakistan Environ Sci Pollut Res Int 23(18):18010–18026. https://doi.org/10.1007/s11356-016-6849-0
Leiden A, Cerdas F, Noriega D, Beyerlein J, Herrmann C (2020) Life cycle assessment of a disposable and a reusable surgery instrument set for spinal fusion surgeries Resources. Conserv Recycl 156:104704. https://doi.org/10.1016/j.resconrec.2020.104704
Malik A, Lenzen M, McAlister S, McGain F (2018) The carbon footprint of Australian health care. Lancet Planet Health 2(1):e27–e35. https://doi.org/10.1016/S2542-5196(17)30180-8
McGain F, McAlister S, McGavin A (2012) Story D (2012) A life cycle assessment of reusable and single-use central venous catheter insertion kits. Anesth Analg 114(5):1073–1080. https://doi.org/10.1213/ANE.0b013e31824e9b69
McGain F, Story D, Lim T, McAlister S (2017) Financial and environmental costs of reusable and single-use anaesthetic equipment. Br J Anaesth 118(6):862–869. https://doi.org/10.1093/bja/aex098
Medicines and Healthcare products Regulatory Agency (2021) Managing Medical Devices. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/965010/Managing_medical_devices022021.pdf. Accessed 13 April 2021
Munakomi S, Shah R, Shrestha S (2018) A pilot study comparing pattern of damage sustained among instruments from different surgical units in a tertiary care centre in Nepal - reappraising the role of instrument reprocessing in retaining their value. F1000Res. 7:102. https://doi.org/10.12688/f1000research.13699.1
NHS Digital (2020) Estates Return Information Collection (ERIC) for 2019/20. https://digital.nhs.uk/data-and-information/publications/statistical/estates-returns-information-collection. Accessed 13 April 2021.
NHS England, NHS Improvement (2020) Delivering a ‘Net Zero’ National Health Service. https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf. Accessed 13 April 2021.
Overcash M (2012) A comparison of reusable and disposable perioperative textiles: sustainability state-of-the-art. Anesth Analg 114(5):1055–1066. https://doi.org/10.1213/ANE.0b013e31824d9cc3
Pier2Pier (2020) Pier2Pier 2020. http://www.pier2pier.com/Co2/. Accessed 13 April 2021
Romanello M, McGushin A, Di Napoli C, Drummond P, Hughes N, Jamart L et al (2021) The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet 398(10311):1619–1662. https://doi.org/10.1016/S0140-6736(21)01787-6
Rizan C, Steinbach I, Nicholson R, Lillywhite R, Reed M, Bhutta M (2020) The carbon footprint of operating theatres: a systematic review. Ann Surg 272(6):986–995. https://doi.org/10.1097/SLA.0000000000003951
Rizan C, Bhutta MF (2021) Environmental impact and life cycle financial cost of hybrid (reusable/single-use) instruments versus single-use equivalents in laparoscopic cholecystectomy. Surg Endosc. Online ahead of print. https://link.springer.com/article/10.1007%2Fs00464-021-08728-z. Accessed 18 Nov 2021.
Rizan C, Reed M, Bhutta MF (2021a) Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic. J R Soc Med 114(5):250–263. https://doi.org/10.1177/01410768211001583
Rizan C, Bhutta M, Reed M et al (2021b) The carbon footprint of waste streams in a UK hospital. J Clean Prod 286:125446. https://doi.org/10.1016/j.jclepro.2020.125446
Rizan C, Lillywhite R, Reed M, Bhutta M (2022) Minimising carbon footprint and financial costs of decontamination (steam sterilisation) and packaging reusable surgical instruments. Br J Surg 109(2):200–210. https://doi.org/10.1093/bjs/znab406
Schulte A, Maga D, Thonemann N (2021) Combining life cycle assessment and circularity assessment to analyze environmental impacts of the medical remanufacturing of electrophysiology catheters. Sustainability 13(2):898. https://doi.org/10.3390/su13020898
Sherman JD, Raibley LA, Eckelman MJ (2018) Life cycle assessment and costing methods for device procurement: comparing reusable and single-use disposable laryngoscopes. Anesth Analg 127(2):434–443. https://doi.org/10.1213/ANE.0000000000002683
Shukla JB, Arora MS, Verma M, Misra AK, Takeuchi Y (2021) The impact of sea level rise due to global warming on the coastal population dynamics: a modeling study. Earth Systems and Environment. Online ahead of print. https://link.springer.com/article/10.1007/s41748-021-00246-1. Accessed 18 Nov 2021.
Sleeswijk AW, van Oers LF, Guinée JB, Struijs J, Huijbregts MA (2008) Normalisation in product life cycle assessment: an LCA of the global and European economic systems in the year 2000. Sci Total Environ 390(1):227–240. https://doi.org/10.1016/j.scitotenv.2007.09.040
Stutler S, Carne G, Gurr J (2013) Reduction in C-section surgical site infections (SSI) achieved through surgical instrument repair. Am J Infec Cont 41(6, Supplement):S16-S7. https://doi.org/10.1016/j.ajic.2013.03.031
Swedwatch Healthier Procurement (2015) Improvements to working conditions for surgical instrument manufacture in Pakistan Report #73. https://swedwatch.org/region/healthier-procurement/. Accessed 13 Dec 2021
Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T et al (2021) Health care’s response to climate change: a carbon footprint assessment of the NHS in England. The Lancet Planetary Health 5(2):e84–e92. https://doi.org/10.1016/S2542-5196(20)30271-0
Thiel CL, Schehlein E, Ravilla T, Ravindran RD, Robin AL, Saeedi OJ et al (2017) Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg 43(11):1391–1398. https://doi.org/10.1016/j.jcrs.2017.08.017
Unger S, Landis A (2016) Assessing the environmental, human health, and economic impacts of reprocessed medical devices in a Phoenix hospital’s supply chain. J Clean Prod 112:1995–2003. https://doi.org/10.1016/j.jclepro.2015.07.144
van Straten B, Dankelman JA, Horeman, T v.d.E (2021) A circular healthcare economy; a feasibility study to reduce surgical stainless steel waste. Sustain Prod Consum 27:169–175. https://doi.org/10.1016/j.spc.2020.10.030
Working Group Instrument Reprocessing (2017) Instrument reprocessing, reprocessing of instruments to retain value. https://8ad5d244-3245-4d36-bc7f-7e3589f4c29b.filesusr.com/ugd/e5e300_d8c2c54d2849453b89a265ae70443b19.pdf?index=true. Accessed 14 April 2021
World Health Organisation (2021) COP26 Health Programme Country Commitments. https://www.who.int/initiatives/cop26-health-programme/country-commitments. Accessed 18 Nov 2021
World Resources Institute (2011) Greenhouse gas protocol, product life cycle accounting and reporting standard. https://www.wri.org/publication/greenhouse-gas-protocol-product-life-cycle-accounting-and-reporting-standard. Accessed 13 April 2021
World Resources Institute (2013) Technical guidance for calculating scope 3 emissions. https://ghgprotocol.org/sites/default/files/standards/Scope3_Calculation_Guidance_0.pdf. Accessed 18 Nov 2021
Wu R (2019) The carbon footprint of the Chinese health-care system: an environmentally extended input–output and structural path analysis study. The Lancet Planetary Health 3(10):e413–e419. https://doi.org/10.1016/S2542-5196(19)30192-5
Wursthorn S, Feifel S, Walk W, Patyk A (2010) An environmental comparison of repair versus replacement in vehicle maintenance. Transp Res Part d: Transp Environ 15(6):356–361. https://doi.org/10.1016/j.trd.2010.02.011
Yoshikawa T, Kimura E, Akama E, Nakao H, Yorozuya T, Ishihara K (2019) Prediction of the service life of surgical instruments from the surgical instrument management system log using radio frequency identification. BMC Health Serv Res 19(1):695. https://doi.org/10.1186/s12913-019-4540-0
Acknowledgements
We thank Roger Manning, managing director of Ream Surgical, for supplying data on offsite instrument repairs, with additional data from sterilisation services staff at Royal Sussex County Hospital, and Tom Brophy (Lead Technologist, The Royal London Hospital) for data on onsite repair.
Funding
This work was conducted as part of Chantelle Rizan’s PhD, with research grants from Health Education England Kent Surrey and Sussex, and The Royal College of Surgeons of England.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Melissa Bilec.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rizan, C., Brophy, T., Lillywhite, R. et al. Life cycle assessment and life cycle cost of repairing surgical scissors. Int J Life Cycle Assess 27, 780–795 (2022). https://doi.org/10.1007/s11367-022-02064-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11367-022-02064-7