Abstract
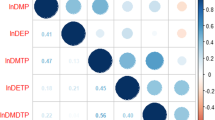
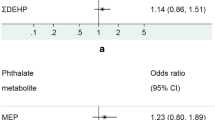
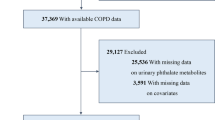
Human health is adversely affected by exposure to organophosphate (OP) pesticides. This study aims to investigate the correlation between urinary OP metabolites and the prevalence of asthma. In cross-sectional studies, data from the National Health and Nutrition Examination Survey (NHANES) projects conducted between 2003–2008, 2011–2012, and 2015–2018 were analyzed. Multiple logistic regressions and restricted cubic spline (RCS) regressions were utilized to examine the relationship between four urinary OP metabolites, namely dimethyl phosphate (DMP), diethyl phosphate (DEP), dimethyl phosphorothioate (DMTP), and diethyl phosphorothioate (DETP), and the prevalence of asthma. Additionally, quantile g-computation (QG-C) regression was employed to evaluate the association between urinary OP metabolites (both individual and combined exposures) and asthma prevalence. The results showed that a total of 9316 adults, including 1298 participants with asthma, were included in the analysis. The median age of the participants was 47.37 years, and 50.27% were female. In the comprehensive model, the third tertile of DMP and DEP exhibited a positive association with asthma prevalence compared to the first tertile (odds ratio [95% confidence interval]: 1.26 [1.01–1.57], Ptrend = 0.036; and 1.25 [1.07–1.51], Ptrend = 0.008, respectively). Moreover, a linear relationship was observed between DMP, DEP, and asthma prevalence (P for nonlinearity = 0.320 and 0.553, respectively). The QG-C regression revealed a positive association between the mixture of urinary OP metabolites and asthma prevalence (OR = 1.04 [1.01–1.07], P = 0.025), with DEP contributing the most substantial effect (weight = 0.564). Our findings suggest that exposure to OP pesticides is associated with an increased prevalence of asthma, with DEP demonstrating the strongest impact.




Similar content being viewed by others
Data availability
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/search/default.aspx.
References
Amitai G, Gaidukov L, Adani R, Yishay S, Yacov G, Kushnir M, Teitlboim S, Lindenbaum M, Bel P, Khersonsky O, Tawfik DS, Meshulam H (2006) Enhanced stereoselective hydrolysis of toxic organophosphates by directly evolved variants of mammalian serum paraoxonase. Febs j 273:1906–1919
Barnthouse M, Jones BL (2019) The impact of environmental chronic and toxic stress on asthma. Clin Rev Allergy Immunol 57:427–438
Beddhu S, Baird BC, Zitterkoph J, Neilson J, Greene T (2009) Physical activity and mortality in chronic kidney disease (NHANES III). Clin J Am Soc Nephrol 4:1901–1906
Bryant DH (1985) Asthma due to insecticide sensitivity. Aust N Z J Med 15:66–68
Costa LG (2018) Organophosphorus compounds at 80: some old and new issues. Toxicol Sci 162:24–35
Desquilbet L, Mariotti F (2010) Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 29:1037–1057
Dharmage SC, Perret JL, Custovic A (2019) Epidemiology of asthma in children and adults. Front Pediatr 7:246
Enilari O, Sinha S (2019) The global impact of asthma in adult populations. Ann Glob Health 85
Eskenazi B, Bradman A, Castorina R (1999) Exposures of children to organophosphate pesticides and their potential adverse health effects. Environ Health Perspect 107(Suppl 3):409–419
Fieten KB, Kromhout H, Heederik D, van Wendel de Joode B, (2009) Pesticide exposure and respiratory health of indigenous women in Costa Rica. Am J Epidemiol 169:1500–1506
Fryer AD, Lein PJ, Howard AS, Yost BL, Beckles RA, Jett DA (2004) Mechanisms of organophosphate insecticide-induced airway hyperreactivity. Am J Physiol Lung Cell Mol Physiol 286:L963–L969
Furlong MA, Herring A, Buckley JP, Goldman BD, Daniels JL, Engel LS, Wolff MS, Chen J, Wetmur J, Barr DB, Engel SM (2017) Prenatal exposure to organophosphorus pesticides and childhood neurodevelopmental phenotypes. Environ Res 158:737–747
Glover F, Eisenberg ML, Belladelli F, Del Giudice F, Chen T, Mulloy E, Caudle WM (2022) The association between organophosphate insecticides and blood pressure dysregulation: NHANES 2013–2014. Environ Health 21:74
Guo X, Wang H, Song Q, Li N, Liang Q, Su W, Liang M, Ding X, Sun C, Lowe S, Sun Y (2022) Association between exposure to organophosphorus pesticides and the risk of diabetes among US Adults: cross-sectional findings from the National Health and Nutrition Examination Survey. Chemosphere 301:134471
Hoppin JA, Umbach DM, London SJ, Henneberger PK, Kullman GJ, Alavanja MC, Sandler DP (2008) Pesticides and atopic and nonatopic asthma among farm women in the Agricultural Health Study. Am J Respir Crit Care Med 177:11–18
Hoppin JA, Umbach DM, Long S, London SJ, Henneberger PK, Blair A, Alavanja M, Freeman LE, Sandler DP (2017) Pesticides are associated with allergic and non-allergic wheeze among male farmers. Environ Health Perspect 125:535–543
Jackson-Browne MS, Eliot M, Patti M, Spanier AJ, Braun JM (2020) PFAS (per- and polyfluoroalkyl substances) and asthma in young children: NHANES 2013–2014. Int J Hyg Environ Health 229:113565
Jayatilaka NK, Restrepo P, Williams L, Ospina M, Valentin-Blasini L, Calafat AM (2017) Quantification of three chlorinated dialkyl phosphates, diphenyl phosphate, 2,3,4,5-tetrabromobenzoic acid, and four other organophosphates in human urine by solid phase extraction-high performance liquid chromatography-tandem mass spectrometry. Anal Bioanal Chem 409:1323–1332
Kapri A, Pant S, Gupta N, Paliwal S, Nain S (2022) Asthma history, current situation, an overview of its control history, challenges, and ongoing management programs: an updated review. Proc Natl Acad Sci India Sect B Biol Sci, 1–13
Kavvalakis MP, Tsatsakis AM (2012) The atlas of dialkylphosphates; assessment of cumulative human organophosphorus pesticides’ exposure. Forensic Sci Int 218:111–122
Keil AP, Buckley JP, O’Brien KM, Ferguson KK, Zhao S, White AJ (2020) A quantile-based g-computation approach to addressing the effects of exposure mixtures. Environ Health Perspect 128:47004
Li W, Ruan W, Cui X, Lu Z, Wang D (2022a) Blood volatile organic aromatic compounds concentrations across adulthood in relation to total and cause specific mortality: a prospective cohort study. Chemosphere 286:131590
Li W, Xiao H, Wu H, Xu X, Zhang Y (2022b) Organophosphate pesticide exposure and biomarkers of liver injury/liver function. Liver Int 42:2713–2723
Louis LM, Buckley JP, Kuiper JR, Meeker JD, Hansel NN, McCormack MC, Diette G, Quirós-Alcalá L (2023) Exposures to organophosphate esters and respiratory morbidity among school-aged children with asthma. Environ Sci Technol 57:6435–6443
Luo K, Zhang R, Aimuzi R, Wang Y, Nian M, Zhang J (2020) Exposure to organophosphate esters and metabolic syndrome in adults. Environ Int 143:105941
Mauer Y, Taliercio RM (2020) Managing adult asthma: the 2019 GINA guidelines. Cleve Clin J Med 87:569–575
Mazurek JM, Syamlal G (2018) Prevalence of asthma, asthma attacks, and emergency department visits for asthma among working adults - National Health Interview Survey, 2011–2016. MMWR Morb Mortal Wkly Rep 67:377–386
McKone TE, Castorina R, Harnly ME, Kuwabara Y, Eskenazi B, Bradman A (2007) Merging models and biomonitoring data to characterize sources and pathways of human exposure to organophosphorus pesticides in the Salinas Valley of California. Environ Sci Technol 41:3233–3240
Mdeni NL, Adeniji AO, Okoh AI, Okoh OO (2022) Analytical evaluation of carbamate and organophosphate pesticides in human and environmental matrices: a review. Molecules 27
Mendy A, Percy Z, Braun JM, Lanphear B, La Guardia MJ, Hale R, Yolton K, Chen A (2023) Exposure to dust organophosphate and replacement brominated flame retardants during infancy and risk of subsequent adverse respiratory outcomes. Environ Res 235:116560
Murrison LB, Brandt EB, Myers JB, Hershey GKK (2019) Environmental exposures and mechanisms in allergy and asthma development. J Clin Invest 129:1504–1515
Odebeatu CC, Taylor T, Fleming LE, N JO, (2019) Phthalates and asthma in children and adults: US NHANES 2007–2012. Environ Sci Pollut Res Int 26:28256–28269
Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC et al (1995) Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 273:402–407
Pathak MK, Fareed M, Srivastava AK, Pangtey BS, Bihari V, Kuddus M, Kesavachandran C (2013) Seasonal variations in cholinesterase activity, nerve conduction velocity and lung function among sprayers exposed to mixture of pesticides. Environ Sci Pollut Res Int 20:7296–7300
Proskocil BJ, Bruun DA, Jacoby DB, van Rooijen N, Lein PJ, Fryer AD (2013) Macrophage TNF-alpha mediates parathion-induced airway hyperreactivity in guinea pigs. Am J Physiol Lung Cell Mol Physiol 304:L519–L529
Qiu Z, Chen X, Geng T, Wan Z, Lu Q, Li L, Zhu K, Zhang X, Liu Y, Lin X, Chen L, Shan Z, Liu L, Pan A, Liu G (2022) Associations of serum carotenoids with risk of cardiovascular mortality among individuals with type 2 diabetes: results from NHANES. Diabetes Care 45:1453–1461
Raanan R, Balmes JR, Harley KG, Gunier RB, Magzamen S, Bradman A, Eskenazi B (2016) Decreased lung function in 7-year-old children with early-life organophosphate exposure. Thorax 71:148–153
Reddel HK et al. (2022) Global Initiative for Asthma Strategy 2021: executive summary and rationale for key changes. Eur Respir J 59
Rohlman DS, Anger WK, Lein PJ (2011) Correlating neurobehavioral performance with biomarkers of organophosphorous pesticide exposure. Neurotoxicology 32:268–276
Schmidt S (2020) Quantile g-computation: a new method for analyzing mixtures of environmental exposures. Environ Health Perspect 128:104004
Shaffo FC, Grodzki AC, Fryer AD, Lein PJ (2018) Mechanisms of organophosphorus pesticide toxicity in the context of airway hyperreactivity and asthma. Am J Physiol Lung Cell Mol Physiol 315:L485–L501
Suresh S, Sabanayagam C, Shankar A (2011) Socioeconomic status, self-rated health, and mortality in a multiethnic sample of US adults. J Epidemiol 21:337–345
Thivel D, Tremblay A, Genin PM, Panahi S, Rivière D, Duclos M (2018) Physical activity, inactivity, and sedentary behaviors: definitions and implications in occupational health. Front Public Health 6:288
Wang M, Jian Z, Ma Y, Jin X, Li H, Wang K (2022) Depression increases the risk of kidney stone: results from the National Health and Nutrition Examination Survey 2007–2018 and Mendelian randomization analysis. J Affect Disord 312:17–21
Wauters RH, Foster BE, Banks TA (2019) Environmental exposures and asthma in active duty service members. Curr Allergy Asthma Rep 19:43
Wu Y, Song J, Zhang Q, Yan S, Sun X, Yi W, Pan R, Cheng J, Xu Z, Su H (2023) Association between organophosphorus pesticide exposure and depression risk in adults: a cross-sectional study with NHANES data. Environ Pollut 316:120445
Yang KJ, Lee J, Park HL (2020) Organophosphate pesticide exposure and breast cancer risk: a rapid review of human, animal, and cell-based studies. Int J Environ Res Public Health 17
Zhang W, Li W, Du J (2022) Association between dietary carotenoid intakes and the risk of asthma in adults: a cross-sectional study of NHANES, 2007–2012. BMJ Open 12:e052320
Zhang Y, Ji L, Hu Y, Tse LA, Wang Y, Qin K, Ding G, Zhou Y, Yu X, Ouyang F, Zhang J, Gao Y, Tian Y, Shanghai Birth Cohort S (2020) Exposure to organophosphate pesticides and menstrual cycle characteristics in chinese preconceptional women. Am J Epidemiol 189:375–383
Acknowledgements
We would like to thank the Centers for Disease Control and Prevention and all research subjects for their participation.
Funding
This study was supported by the Science and Technology Innovation 2025 Major Project of Ningbo (2019B10037).
Author information
Authors and Affiliations
Contributions
Ning Zhu, Shanhong Lin, and Chao Cao conceived and designed the study. Ning Zhu, Hang Yu, and Weina Huang extracted the data and analyzed and interpreted the data. Ning Zhu, Chao Cao, and Shanhong Lin contributed to drafting and editing the paper and full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors have given the final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. This study uses only secondary data analyses without any personal information identified using statistical data from NHANES website; no further ethical approval for conducting the present study is required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, N., Lin, S., Huang, W. et al. Association of urinary organophosphate metabolites with adult asthma patients: a cross-sectional population-based study. Environ Sci Pollut Res 30, 112977–112987 (2023). https://doi.org/10.1007/s11356-023-30174-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-30174-8