Abstract
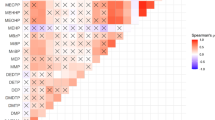
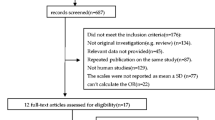
Attention deficit hyperactivity disorder (ADHD) is associated with heavy metal exposure during adolescent development. However, the direct clinical evidence is limited. To investigate the possible association between environmental heavy metal exposure and ADHD, a case-control study was conducted with children aged 6–14 years in Guangzhou, China. Results showed that median concentrations of chromium (Cr), manganese (Mn), cobalt (Co), nickel (Ni), copper (Cu), molybdenum (Mo), tin (Sn), barium (Ba), and lead (Pb) in the urine of the case group were significantly higher than those of the control group. Children with ADHD had significantly higher levels of 8-OHdG and MDA compared with those from the control group. In addition, correlations between urinary Co, Ni, Cu, Mo, and Sn were significantly correlated with 8-OHdG and MDA concentrations in urine. After the case and control groups were combined together and the first quartile was used as the reference category, odds ratios (ORs) of ADHD for children increased significantly with the quartile increasing of urinary Co, Cu, and Sn. Our study provides a clinical evidence that Co, Cu, and Sn exposure, particularly Sn exposure, may be an environmental risk of the incurrence of ADHD for children. Furthermore, Co, Ni, Cu, Mo, and Sn exposures were significantly correlated with DNA and lipid damage.


Similar content being viewed by others
References
Abdullah MM, Ly AR, Goldberg WA, Clarke-Stewart KA, Dudgeon JV, Mull CG, Chan TJ, Kent EE, Mason AZ, Ericson JE (2012) Heavy metal in children’s tooth enamel: related to autism and disruptive behaviors? J Autism Dev Disord 42:929–936
Achenbach TMEC (1983) Manual for the child: behavior checklist and revised child behavior profile. Manual for the Child: Behavior Checklist and Revised Child Behavior Profile
Akhondzadeh S, Mohammadi MR, Khademi M (2004) Zinc sulfate as an adjunct to methylphenidate for the treatment of attention deficit hyperactivity disorder in children: a double blind and randomized trial [ISRCTN64132371]. Bmc Psychiatry 4:9
Arnold LE, DiSilvestro RA (2005) Zinc in attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 15:619–627
Association AP (2013) Diagnostic and statistical manual of mental disorders (DSM-5). American Psychiatric Publishing
Balaban CD, O’Callaghan JP, Billingsley ML (1988) Trimethyltin-induced neuronal damage in the rat brain: comparative studies using silver degeneration stains, immunocytochemistry and immunoassay for neuronotypic and gliotypic proteins. Neuroscience 26:337–361
Barkley RA, Murphy KR, Dupaul GJ, Bush T (2002) Driving in young adults with attention deficit hyperactivity disorder: knowledge, performance, adverse outcomes, and the role of executive functioning. J Int Neuropsychol Soc 8:655–672
Bilici M, Yildirim F, Kandil S, Bekaroglu M, Yildirmis S, Deger O, Ulgen M, Yildiran A, Aksu H (2004) Double-blind, placebo-controlled study of zinc sulfate in the treatment of attention deficit hyperactivity disorder. Prog Neuro-Psychopharmacol Biol Psychiatry 28:181–190
Black MM (1998) Zinc deficiency and child development. Am J Clin Nutr 68:464S–469S
Bradberry SM (2016) Metals (cobalt, copper, lead, mercury). Medicine 44:182–184
Buck LB (2004) The search for odorant receptors. Cell 116:S117–S119
Casas M, Forns J, Martinez D, Avella-Garcia C, Valvi D, Ballesteros-Gomez A, Luque N, Rubio S, Julvez J, Sunyer J, Vrijheid M (2015) Exposure to bisphenol A during pregnancy and child neuropsychological development in the INMA-Sabadell cohort. Environ Res 142:671–679
Chang LW, Tiemeyer TM, Wenger GR, McMillan DE (1982) Neuropathology of mouse hippocampus in acute trimethyltin intoxication. Neurobehav Toxicol Teratol 4:149–156
Chauhan A, Chauhan V, Brown WT, Cohen I (2004) Oxidative stress in autism: Increased lipid peroxidation and reduced serum levels of ceruloplasmin and transferrin - the antioxidant proteins. Life Sci 75:2539–2549
Chovanova Z, Muchova J, Sivonova M, Dvorakova M, Zitnanova I, Waczulikova I, Trebaticka J, Skodacek I, Durackova Z (2006) Effect of polyphenolic extract, Pycnogenol (R), on the level of 8-oxoguanine in children suffering from attention deficit/hyperactivity disorder. Free Radic Res 40:1003–1010
Dyer RS, Walsh TJ, Wonderlin WF, Bercegeay M (1982) The trimethyltin syndrome in rats. Neurobehav Toxicol Teratol 4:127–133
Feldman RG, White RF, Eriator II (1993) Trimethyltin encephalopathy. Arch Neurol 50:1320–1324
Goodlad JK, Marcus DK, Fulton JJ (2013) Lead and attention-deficit/hyperactivity disorder (ADHD) symptoms: a meta-analysis. Clin Psychol Rev 33:417–425
Goyette CH, Conners CK, Ulrich RF (1978) Normative data on revised Conners parent and teacher rating scales. J Abnorm Child Psychol 6:221–236
Harley KG, Gunier RB, Kogut K, Johnson C, Bradman A, Calafat AM, Eskenazi B (2013) Prenatal and early childhood bisphenol A concentrations and behavior in school-aged children. Environ Res 126:43–50
He J, Ning H, Huang R (2019) Low blood lead levels and attention-deficit hyperactivity disorder in children: a systematic review and meta-analysis. Environ Sci Pollut Res Int 26:17875–17884
Huang S, Hu H, Sánchez BN, Peterson KE, Ettinger AS, Lamadrid-Figueroa H, Schnaas L, Mercado-García A, Wright RO, Basu N, Cantonwine DE, Hernández-Avila M, Téllez-Rojo MM (2016) Childhood blood lead levels and symptoms of attention deficit hyperactivity disorder (ADHD): a cross-sectional study of Mexican children. Environ Health Perspect 124:868–874
Hubbs-Tait L, Nation JR, Krebs NF, Bellinger DC (2005) Neurotoxicants, micronutrients, and social environments: individual and combined effects on children’s development. Psychol Sci Public Interest 6:57–121
Kiecolt-Glaser JK, Graham JE, Malarkey WB, Porter K, Lemeshow S, Glaser R (2008) Olfactory influences on mood and autonomic, endocrine, and immune function. Psychoneurol Endocrinol 33:328–339
Lecendreux M, Konofal E, Faraone SV (2011) Prevalence of attention deficit hyperactivity disorder and associated features among children in France. J Atten Disord 15:516–524
Li Y, Zhang H, Kuang H, Fan R, Cha C, Li G, Luo Z, Pang Q (2018) Relationship between bisphenol A exposure and attention-deficit/ hyperactivity disorder: a case-control study for primary school children in Guangzhou, China. Environ Pollut 235:141–149
Misra MK, Sarwat M, Bhakuni P, Tuteja R, Tuteja N (2009) Oxidative stress and ischemic myocardial syndromes. Med Sci Monit 15:RA209–RA219
Mitra AK, Ahua E, Saha PK (2012) Prevalence of and risk factors for lead poisoning in young children in Bangladesh. J Health Popul Nutr 30:404–409
Moon GJ, Kim SJ, Cho YH, Ryoo S, Bang OY (2014) Antioxidant effects of statins in patients with atherosclerotic cerebrovascular disease. J Clin Neurol 10:140–147
Needleman HL (2004) Low level lead exposure and the development of children. Southeast Asian J Trop Med Public Health 35:252–254
Nigg JT, Nikolas M, Knottnerus GM, Cavanagh K, Friderici K (2010) Confirmation and extension of association of blood lead with attention-deficit/hyperactivity disorder (ADHD) and ADHD symptom domains at population-typical exposure levels. J Child Psychol Psychiatry 51:58–65
Palur G, Gunasekar VMDK, Vladislav Eybl AGEI (2001) Role of astrocytes in trimethyltin neurotoxicity. J Biochem Mol Toxicol 15:256–262
Patros CHG, Alderson RM, Kasper LJ, Tarle SJ, Lea SE, Hudec KL (2016) Choice-impulsivity in children and adolescents with attention-deficit/hyperactivity disorder (ADHD): a meta-analytic review. Clin Psychol Rev 43:162–174
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatr 164:942–948
Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA (2014) ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol 43:434–442
Quist JF, Kennedy JL (2001) Genetics of childhood disorders: XXIII. ADHD, Part 7: The serotonin system. J Am Acad Child Adolesc Psychiatry 40:253–256
Russo AJ (2010) Decreased serum Cu/Zn SOD associated with high copper in children with attention deficit hyperactivity disorder (ADHD). J Cent Nerv Syst Dis 2:9–14
Saiki R, Park H, Ishii I, Yoshida M, Nishimura K, Toida T, Tatsukawa H, Kojima S, Ikeguchi Y, Pegg AE, Kashiwagi K, Igarashi K (2011) Brain infarction correlates more closely with acrolein than with reactive oxygen species. Biochem Biophys Res Commun 404:1044–1049
Segal M (1988) Behavioral and physiological effects of trimethyltin in the rat hippocampus. Neurotoxicology 9:481–490
Simsek S, Gencoglan S, Ozaner S, Kaplan I, Kaya MC (2016) Antioxidant status and DNA damage in children with attention deficit hyperactivity disorder with or without comorbid disruptive behavioral disorders. Klin Psikofarmakol B 26:119–125
Skalny AV, Mazaletskaya AL, Ajsuvakova OP, Bjørklund G, Skalnaya MG, Chao JCJ, Chernova LN, Shakieva RA, Kopylov PY, Skalny AA, Tinkov AA (2020) Serum zinc, copper, zinc-to-copper ratio, and other essential elements and minerals in children with attention deficit/hyperactivity disorder (ADHD). J Trace Elem Med Biol 58:126445
Stanton ME, Jensen KF, Pickens CV (1991) Neonatal exposure to trimethyltin disrupts spatial delayed alternation learning in preweanling rats. Neurotoxicol Teratol 13:525–530
Talarovicova A, Krskova L, Kiss A (2007) Some assessments of the amygdala role in suprahypothalamic neuroendocrine regulation: a minireview. Endocr Regul 41:155–162
Tamburella A, Micale V, Mazzola C, Salomone S, Drago F (2012) The selective norepinephrine reuptake inhibitor atomoxetine counteracts behavioral impairments in trimethyltin-intoxicated rats. Eur J Pharmacol 683:148–154
Tewar S, Auinger P, Braun JM, Lanphear B, Yolton K, Epstein JN, Ehrlich S, Froehlich TE (2016) Association of bisphenol A exposure and attention-deficit/hyperactivity disorder in a national sample of US children. Environ Res 150:112–118
Thomas R, Sanders S, Doust J, Beller E, Glasziou P (2015) Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics 135:E994–E1001
Tinkov AA, Mazaletskaya AL, Ajsuvakova OP, Bjorklund G, Huang PT, Chernova LN, Skalny AA, Skalny AV (2019) ICP-MS assessment of hair essential trace elements and minerals in Russian preschool and primary school children with attention-deficit/hyperactivity disorder (ADHD). Biol Trace Elem Res
Toren P, Eldar S, Sela BA, Wolmer L, Weitz R, Inbar D, Koren S, Reiss A, Weizman R, Laor N (1996) Zinc deficiency in attention-deficit hyperactivity disorder. Biol Psychiatry 40:1308–1310
Wang T, Liu K, Li Z, Xu Y, Liu Y, Shi W, Chen L (2017) Prevalence of attention deficit/hyperactivity disorder among children and adolescents in China: a systematic review and meta-analysis. Bmc Psychiatry 17:32
Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, Loo SK, Carlson CL, McBurnett K, Lahey BB (2012) Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. J Abnorm Psychol 121:991–1010
Winneke G (2011) Developmental aspects of environmental neurotoxicology: lessons from lead and polychlorinated biphenyls. J Neurol Sci 308:9–15
Yanofsky NN, Nierenberg D, Turco JH (1991) Acute short-term memory loss from trimethyltin exposure. J Emerg Med 9:137–139
Yousef S, Adem A, Zoubeidi T, Kosanovic M, Mabrouk AA, Eapen V (2011) Attention deficit hyperactivity disorder and environmental toxic metal exposure in the United Arab Emirates. J Trop Pediatr 57:457–460
Zhang H, Kuang H, Luo Y, Liu S, Meng L, Pang Q, Fan R (2019) Low-dose bisphenol A exposure impairs learning and memory ability with alterations of neuromorphology and neurotransmitters in rats. Sci Total Environ 697:134036
Zhou F, Wu F, Zou S, Chen Y, Feng C, Fan G (2016) Dietary, nutrient patterns and blood essential elements in Chinese children with ADHD. Nutrients 352:1–14
Zhou Y, Wang Z, Xia M, Zhuang S, Gong X, Pan J, Li C, Fan R, Pang Q, Lu S (2017) Neurotoxicity of low bisphenol A (BPA) exposure for young male mice: implications for children exposed to environmental levels of BPA. Environ Pollut 229:40–48
Funding
This research was supported by grants from the Opening Foundation of Guangdong Key Laboratory of Environmental Catalysis and Health Risk Control (No. GKECHRC-04) and the National Natural Science Foundation of China (No. 21777048, No. 21477041 and No. 41731279).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
This study was approved by the Research Ethics Committee of South China Normal University.
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Responsible editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Y., Cha, C., Lv, X. et al. Association between 10 urinary heavy metal exposure and attention deficit hyperactivity disorder for children. Environ Sci Pollut Res 27, 31233–31242 (2020). https://doi.org/10.1007/s11356-020-09421-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-020-09421-9