Abstract
Purpose
The aim of this study was to investigate the effects of high-intensity interval training (HIIT) with probiotic supplementation (Lactobacillus rhamnosus GG) on gene expression of NF-κβ and CXCL2 in small intestine of rats with hepatic steatosis (induced by tetracycline).
Methods
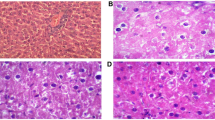
Forty male Wistar rats (200 ± 20 g) were randomly divided into five groups of (n = 8 in each group): healthy control (HC), hepatic steatosis (HS), HS + HIIT, HS + probiotic (Pro) 5. HS + HIIT + Pro. Tetracycline was gavage at a dose of 140 mg/kg, for 7 days, to induce hepatic steatosis. The HIIT performed 5 sessions per week for 5 weeks on the rodent treadmill. Probiotic groups received 109 CFU/ml of Lactobacillus rhamnosus GG by oral gavage for 5 weeks (daily). ALT and AST were measured to confirm of HS. NF-κβ and CXCL2 genes were measured by Real-Time PCR in small intestine (jejunum).
Results
The results showed that there was a significant difference in gene expression of NF-κβ and CXCL2 (jejunum) between groups (p < 0.001). NF-κβ and CXCL2 mRNA levels in the steatosis group were greater than healthy controls (p < 0.05), while probiotic and HIIT groups had a lower intestinal NF-κβ and CXCL2 mRNA compared to steatosis group (p < 0.05).
Conclusions
Probiotic supplementation with HIIT leads to optimal cellular adaptation and the lower expression of NF-κβ and CXCL2 in the intestinal tissue of rats with fatty liver (steatosis). Due to the role of NF-κβ in regulation of apoptotic genes and proinflammatory cytokines, as well as the effect of CXCL2 on metabolism, insulin function and inflammatory responses, it seems that HIIT and probiotic may be effective in controlling fatty liver and gastrointestinal diseases.





Similar content being viewed by others
References
Odiaga JA, Doucette J (2017) Technological media and sedentary behavior in pediatrics. J Nurse Pract 13(1):72–78
Willett WC et al. (2006) Prevention of chronic disease by means of diet and lifestyle changes, in disease control priorities in developing countries, 2nd edition. The International Bank for Reconstruction and Development/The World Bank
Nasr P et al (2020) The amount of liver fat predicts mortality and development of type 2 diabetes in non-alcoholic fatty liver disease. Liver Int 40(5):1069–1078
Brouwers MC et al (2020) Non-alcoholic fatty liver disease and cardiovascular disease: assessing the evidence for causality. Diabetologia 63:253
Tarantino G, Balsano C (2020) Gastrointestinal peptides and nonalcoholic fatty liver disease. Curr Opin Endocrinol Diabetes Obes 27(1):11–15
Gomez-Dominguez E et al (2006) A pilot study of atorvastatin treatment in dyslipemid, non-alcoholic fatty liver patients. Aliment Pharmacol Ther 23(11):1643–1647
Hallsworth K et al (2011) Resistance exercise reduces liver fat and its mediators in non-alcoholic fatty liver disease independent of weight loss. Gut 60(9):1278–1283
Skrypnik D et al (2016) Effects of endurance and endurance–strength exercise on biochemical parameters of liver function in women with abdominal obesity. Biomed Pharmacother 80:1–7
Arabzadeh E et al (2020) Alteration of follistatin-like 1, neuron-derived neurotrophic factor, and vascular endothelial growth factor in diabetic cardiac muscle after moderate-intensity aerobic exercise with insulin. Sport Sci Health. https://doi.org/10.1007/s11332-020-00631-9
van der Windt DJ et al (2018) The effects of physical exercise on fatty liver disease. Gene Expr 18(2):89
Hashida R et al (2017) Aerobic vs. resistance exercise in non-alcoholic fatty liver disease: a systematic review. J hepatol 66(1):142–152
Hallsworth K et al (2015) Modified high-intensity interval training reduces liver fat and improves cardiac function in non-alcoholic fatty liver disease: a randomized controlled trial. Clin Sci 129(12):1097–1105
Pedersen BK, Fischer CP (2007) Beneficial health effects of exercise–the role of IL-6 as a myokine. Trends Pharmacol Sci 28(4):152–156
Catoire M et al (2014) Identification of human exercise-induced myokines using secretome analysis. Physiol Genom 46(7):256–267
Sun S-C (2017) The non-canonical NF-κB pathway in immunity and inflammation. Nat Rev Immunol 17(9):545
Kapil S et al (2016) Small intestinal bacterial overgrowth and toll-like receptor signaling in patients with non-alcoholic fatty liver disease. J Gastroenterol Hepatol 31(1):213–221
Anuradha S, Rajeshwari K (2005) Probiotics in health and disease. J Indian Acad Clin Med 6(1):67–72
Dilnawaz P, Shakeel M, Tabrez S (2011) A review on probiotics. Int Res J Pharm 2:26–33
Shabana M et al (2012) Influence of rifampicin and tetracycline administration on some biochemical and histological parameters in albino rats. J Basic Appl Zool 65(5):299–308
Kalaki-Jouybari F et al (2020) High-intensity interval training (HIIT) alleviated NAFLD feature via miR-122 induction in liver of high-fat high-fructose diet induced diabetic rats. Arch Physiol Biochem 126(3):242–249
Brunt EM et al (1999) Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol 94(9):2467–2474
Sakharkar AJ et al (2014) Effects of acute ethanol exposure on anxiety measures and epigenetic modifiers in the extended amygdala of adolescent rats. Int J Neuropsychopharmacol 17(12):2057–2067
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2− ΔΔCT method. Methods 25(4):402–408
Schnabl B, Brenner DA (2014) Interactions between the intestinal microbiome and liver diseases. Gastroenterology 146(6):1513–1524
Ley RE et al (2006) Human gut microbes associated with obesity. Nature 444(7122):1022–1023
Zhang H et al (2009) Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci 106(7):2365–2370
Luedde T, Schwabe RF (2011) NF-κB in the liver—linking injury, fibrosis and hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol 8(2):108–118
Sun B, Karin M (2008) NF-κB signaling, liver disease and hepatoprotective agents. Oncogene 27(48):6228–6244
Taghibeigi Hoseinabadi H et al (2019) Effects of eight weeks of aerobic training on expression levels of the HMGB1-RAGE/TLR4-NF-kB proinflammatory pathway in cardiac tissue of male rats with hyperglycemia. Iran J Endocrinol Metab 20(5):246–252
Chen J, Thomsen M, Vitetta L (2019) Interaction of gut microbiota with dysregulation of bile acids in the pathogenesis of nonalcoholic fatty liver disease and potential therapeutic implications of probiotics. J Cell Biochem 120(3):2713–2720
Chavez-Tapia NC et al (2015) Current evidence on the use of probiotics in liver diseases. J Funct Foods 17:137–151
Rodrigues FM et al (2019) Physical exercise alters hepatic morphology of low-density lipoprotein receptor knockout ovariectomized mice. Med Mol Morphol 52(1):15–22
Ma Y-Y et al (2013) Effects of probiotics on nonalcoholic fatty liver disease: a meta-analysis. World J Gastroenterol 19(40):6911
Paolella G et al (2014) Gut-liver axis and probiotics: their role in non-alcoholic fatty liver disease. World J Gastroenterol 20(42):15518
Barry JC et al (2017) Short-term exercise training alters leukocyte chemokine receptors in obese adults. Med Sci Sports Exerc 49(8):1631–1640
Ha J et al (2010) CXC chemokine ligand 2 induced by receptor activator of NF-κB ligand enhances osteoclastogenesis. J Immunol 184(9):4717–4724
Carlin JL et al (2016) Voluntary exercise blocks Western diet-induced gene expression of the chemokines CXCL10 and CCL2 in the prefrontal cortex. Brain Behav Immun 58:82–90
Arabzadeh E, Mirdar S, Moradiani H (2016) Nigella sativa supplementation attenuates exercise-induced bronchoconstriction in the maturing rat: a histometric and histologic study. Comp Clin Pathol 25(1):1–5
Funding
No funding.
Author information
Authors and Affiliations
Contributions
All authors equally contribute in preparation of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All experimental protocols were approved by the Ethics Committee of the Baqiyatallah University of Medical Science.
Informed consent
All authors consent to this manuscript submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohammadi, S., Rostamkhani, F., Riyahi Malayeri, S. et al. High-intensity interval training with probiotic supplementation decreases gene expression of NF-κβ and CXCL2 in small intestine of rats with steatosis. Sport Sci Health 18, 491–497 (2022). https://doi.org/10.1007/s11332-021-00829-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-021-00829-5