Abstract
Background
There is the highest estimated number of patients with obstructive sleep apnea (OSA) in China. Early treatment could lead to fewer complications associated with OSA. This study aimed to analyze the factors influencing help-seeking from the first symptom discovery to treatment in OSA.
Methods
Semi-structured interview outline was designed to conduct face-to-face interview based on the analyses of a great number of related literatures on the delay in seeking medical attention of patients with OSA. 15 patients diagnosed were interviewed between June 2021 to September 2022 in general hospital of Shenyang, Northeastern of China. Qualitative data was analyzed by content analysis using the Model of Pathways to Treatment.
Results
Analyses identified factors contributing to elapsed time from first symptom discovery to received treatment that are linked to disease characteristic, patients, health system organization. Appraisal interval is most obvious for patients with OSA, but it is difficult to pinpoint precisely because the patients didn’t remember exactly when the first symptom was detected.
Conclusions
Patients diagnosed with OSA didn’t initially interpret the snore as a warning sign and even thought it was a blessing. The findings provided guidance or avenues for reducing elapsed time between the first symptom and received treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a common sleep disorder caused by repeated upper airway partial or total collapse at night during sleep, resulting in hypopnea and a drop in blood oxygen [1]. It could bring about different degrees of chronic intermittent hypoxia and hypercarbia, often accompanied by daytime sleepiness, fatigue, depression and other symptoms, which further lead to the other multi-system lesions and damage including cardiovascular system, endocrine system, nervous system and so on. Evidence suggests that the incidence rates of OSA has showed a gradual increasing trend [2].
However, the medical treatment status of OSA patients is not optimistic. Furthermore, it is a very important thought-provoking problem that delay in medical treatment of OSA patients. Finkel et al. [3, 4] pointed out that 82% of men and 93% of women in patients with moderate and severe OSA hadn’t been diagnosed definitively due to that they were not aware of their snoring symptom at night and did not seek medical attention in time. Henry [5] conducted semi-structured interviews with 24 OSA patients and their families, and pointed out that the average delay in seeking medical treatment for OSA patients was (4.8 ± 5.8) years, (5.5 ± 8.7) years for male patients and (4.0 ± 3.4) years for female patients. It was reported that the fatality rate was 13% of OSA patients who were not diagnosed and treated timely due to delayed medical treatment within 5 years, and 37% of OSA patients with apnea hypopnea index (AHI) above 20 within 8 years [6]. What is the status quo of the delays of 176 million OSA patients in China? And what are the influencing factors for them?
The objective of the article is to identify the influencing factors delay in seeking medical attention of patients with OSA. It is necessary to understand the process of delayed medical treatment in OSA patients and its related influencing factors for medical personnel and healthcare policymakers. However, there were few studies on the delay of medical treatment of OSA at home and abroad, which didn’t pay attention to the delay of diagnosis and treatment, and lack of theoretical support. The study attempted to apply the Model of Pathways to Treatment originally applied to cancer research to the study of delay in seeking medical attention of OSA.
New contribution
The contribution of the article is threefold. First, the Model of Pathways to Treatment was applied in patients with OSA. According to the theory, the results reveal that the delay in appraisal interval is most obvious to patients with OSA, which provide a certain direction for the formulation of relevant intervention policies. More potential influencing factors that may delay medical treatment could be uncovered by semi-open-ended questions, which can be divided into individual, the health service system and the disease. Moreover, the results show that to improve delay in seeking medical treatment requires the efforts of individuals, society and the state.
Methods
Conceptual framework
The Model of Pathways to Treatment was originated and refined from the Andersen’s Model of Total Patient Delay [7]. There were five stages: appraisal delay, illness delay, behavioral delay, scheduling delay, treatment delay in Andersen’s Model of Total Patient Delay. However, it has the flaws of lack of specification of time intervals measured for illness delay and appraisal delay. And it was difficult to confirm the exact duration of the behavior delay. Thus, the Model of Pathways to Treatment was modified by Walter [8] (see Fig. 1). The refinement of Andersen’s model identified four intervals: appraisal interval, help-seeking interval, diagnostic interval, pre-treatment interval. The appraisal interval refers to the period of time between the onset of somatic symptoms and the awareness to seek medical attention. The help-seeking interval is the period a person conscious of seeking medical attention decides to consult up to the first visit with a physician. The diagnostic interval is the interval between a person consulting up to the first visit with a physician and be diagnosed definitely after various tests and examinations. The pre-treatment interval could be defined as the hesitating stage before a planned treatment. There are serious advantages of The Model of Pathways to Treatment. The first and most important feature is that the starting point of each stage can be identified by patients, clinicians and researchers distinctly. Secondly, many influencing aspects have been clearly identified during the whole process of delays in seeking medical care by The Model of Pathways to Treatment, such as the individual, the health service system and the disease. The Model of Pathways to Treatment had been applied ever since it was proposed in many studies, which is widely used in the research of tumors, such as colorectal cancer, female tumors with high incidence, brain tumors. It is well suited to elaborate entire process of delays in seeking medical attention of OSA with The Model of Pathways to Treatment for that the theory has a good predictive and explanatory power on medical seeking behavior.
The Model of pathways to treatment [8] (HCP, healthcare professional)
Study design and collection and analysis of qualitative data
The qualitative research presented here was conducted among 15 adult patients with OSA to reveal the factors influencing the delays in seeking medical attention between first symptom and treatment with adult patients with OSA. The enrolled subjects were located in three provinces in northeast China.
We defined the operational definition of delay in seeking medical attention with adult patients with OSA on the basis of following these steps. Delay in seeking medical attention was defined as the time interval between the onset of moderate to severe snoring symptoms and the first visit to the doctor for the symptom of OSA being more than 3 months. First, we have carried through literature reviews for the purpose of forming operational definition of delaying in seeking medical attention with adult patients with OSA. According to the selection criteria, 5 experts in related fields were selected and invited. The selection criteria for experts were as follows: (a) Higher academic level in OSA treatment and nursing; (b) Rich experience in clinical treatment and nursing; (c) Be familiar with the development of measuring tools and measuring methods of psychometric characteristics; (d) Associate senior or above professional titles. Then we had an expert consultation by Delphi method for an uncertainty. The uncertainty stems from the fact that OSA is essentially a different disease from cancer. As for cancer, the interval time that three months or over was defined as delay in seeking medical attention. What about for OSA? Or that, the interval time that between the onset of somatic symptoms and serious complication of OSA was defined as delay in seeking medical attention. Which one was more appropriate for OSA? Finally, the perspectives or recommendations of experts were asked in person or by email about the definition of delay in seeking medical attention. Two rounds of expert consultations had been conducted until expert consensus is reached.
The project has been approved by the Ethics Committee of the First Affiliated Hospital of China Medical University. Before the start of the study, the purpose and significance of the study were explained to the patients and their families, and then the informed consent was signed with the participant to ensure that the investigation results were only used in the study and the strict confidentiality principle should be followed.
Semi-structured interviews lasting approximately 30 min to one hour were conducted by the researcher and were audio-recorded with the respondents’ consent. According to the willingness of the participants, the interview was conducted in the quiet environment, such as a sleep clinic laboratory, a group meeting room or the participants’ home. All interviews were transcribed and subsequently analyzed by the method of theme analysis within 24 h. The facts that the initial symptom of respondents’, the reasons for not seeking medical attention in time, and the barriers encountered during the medical treatment, such as financial difficulties and complicated medical procedures were explored by open-ended questions. When patients forgot the specific date of their first symptom, they would been given some questions that the events of special significance of the life designed to minimize memory bias, such as “were you married at the time? did you already have your first baby? and how old was the first baby?” We conducted 15 in-depth interviews between June 2021 and September 2022. All interviews were double-coded separately by two researchers. If there were any divergences, it would be discussed in the team meetings in order to reach a consensus. We have summarized and analyzed each subject’s treatment pathway. When there were no more new themes, that was, theme saturation, the interview was stopped. However, we can’t say we’ve explored all the examples because of the diversity of the stories.
Results
The characteristics of 15 patients with OSA in the interview were displayed in Table 1. A large proportion of onset symptoms of OSA could be easily recognized except that a fraction of symptoms is less typical, such as encephalalgia, fatigue. For example, respondent 13 finally was recommended for polysomnography (PSG) after seeking medical recommendations of a lot of different departments for her atypical headache. We have arranged the appraisal interval from six months to 50 years (see Table 2).
The intervals
The longest appraisal interval from first onset symptom to the awareness to seek medical attention is 50 years and the shortest, six months. Sometimes it is difficult for subjects to accurately quantify the appraisal interval. The help-seeking interval is generally shorter than the appraisal interval, ranging from four days to three years. The longest diagnostic interval is two years due to lack of necessary doctors and equipment or absence of a companion. The respondent 13 who had been suffering from headache delayed for 2 years, one reason was that the local hospital did not have relevant equipment, so she had to go to a superior hospital, and the other reason was that it must been accompanied to do polysomnography (PSG) in the superior hospital. The absence of the pre-treatment interval here is due to the fact that only three subjects showed a preference of treatment, which was also confirmed at the follow-ups, two respondents underwent surgery of ear, nose, and throat (ENT) department within six months and one continuous positive airway pressure (CPAP) within one year.
Explanatory factors related to OSA
All participants in the interviews reported clinical symptoms. Two respondents (respondents 3, 10) reported suffering from throat symptoms (polyp of vocal cord, hypertrophy of tonsil), but no apnea, which wasn’t the same as five respondents (respondents 2, 5, 6, 8, 11). However, the other five respondents (respondents 4, 7, 9, 14, 15) didn’t seek medical attention until they developed various complications (gastroesophageal reflux, high blood pressure, heart trouble). The symptom of two patients interviewed (respondents 1, 12) was fatigue. Respondent 13 had been plagued by headache for years. The clinical manifestations of these non-acute symptoms affect patients’ seeking medical attention behavior to some extent.
Factors related to patients
Most people hadn’t been conscious of the fact that they were snoring before informed by their partner or roommate. For example, respondent 4 hadn’t been aware of his snoring until his roommate told him. In addition to this, some subjects also reported periods of fatigues that were mistaken for being too tired at work. We observed two extremes of reported truths from the respondents in the interviews. One was that the patients with stronger social support had relatively shorter intervals, whose medical seeking behaviors were produced from respondents’ spouse (husband or wife) or relatives and friends. The other fact was the respondents with a family history of snoring had longer intervals. They mistook that they should be fine because the older generation in their family have been snoring for years and still be fine. Besides, the respondents with a family history were universally less confident in treatment.
Factors related to health system organization
The 15 respondents were from primary hospitals, municipal hospitals and provincial hospitals according to the location of seeking medical attention. The primary hospital refers to township hospitals, village clinics and community hospitals that provide basic public health services and basic medical services, mainly serving rural residents. There are few outpatient clinics for OSA in primary hospitals. We found that there was no respondent had been referred by primary hospitals except for respondent 5. Most people were referred from municipal hospitals, which are mainly managed by the municipal-level health system organization and provide medical and health services to residents in the entire municipal area. Some municipal hospitals in part don’t have enough the diagnostic or therapeutic equipment. Thus, they tended to prefer provincial hospitals encouraged by municipal hospitals. But, for provincial hospitals, there were fewer beds per capita in the sleep laboratory room or center available for appointment more patients. The main reason is that provincial hospitals provide health services within the province and throughout the country, which are usually directly managed by the provincial-level health system organization. These factors prolonged the patient’s diagnosis delay to a certain extent.
Discussion
Strengths and limitations of the study
The study was based on the theory of the Model of Pathways to Treatment. The application of the Model of Pathways to Treatment in the study made up for the lack of theoretical support in previous studies on the delay in medical treatment of patients with OSA. According to the theory, the patient’s delay was divided into appraisal interval, help-seeking interval, diagnostic interval. And most importantly, we were able to clearly understand the most obvious part of the patient’s delay, which was the appraisal interval. After that, we have analyzed the factors that affected the delays in seeking medical attention from the perspectives of the individual, the disease, and the health service system. So, the results provided a powerful intervention direction for future research and the public health administration. However, one thing to be clear was that the self-reported intervals in the interviews were estimated by the events of special significance in their lives, which was impossible to pinpoint the exact date.
Time elapsed before diagnosed and determining factors
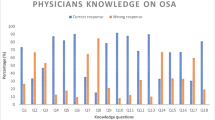
It can be seen that the delay rate for patients with OSA in seeking health care is relatively high. The interviews show that the shortest delay interval for patients with OSA to seek health care behavior is 0.5 years, all of which are more than 3 months, with a delay rate of 100% and the longest time being 50 years. As far as the respondents were concerned, they often didn’t aware the fact that they were snoring during the sleep, the leading cause of delayed medical treatment. They didn’t realize it until they were told by their spouse or roommate. Furthermore, traditional wisdom holds that snoring is a sign of good health and happiness, or the snoring is a blessing in Chinese culture. In the situation, they don’t know what OSA is and how harmful it is to the target organ. They assumed that snoring was not a big deal even though they already knew that they were snoring in the sleep, which was most obvious in the 13 patients with a family history of snoring. It’s not surprising that the subjects with the false perception had a long delay in seeking medical advice. What’s more, the subjects with lower social support, were more likely to delay in seeking medical treatment than those with higher social support mainly from their spouses [5, 9,10,11]. Besides, the subjects often use busyness as an excuse to delay seeking medical attention [12]. However, this phenomenon is more evident in the middle-aged and elderly than in the young and middle-aged. Patients in the young and middle-aged, the life stage of “having both parents and young children to support and take care of”, may pay more attention to the health because a strong sense of responsibility forces them to keep healthy, which promotes them to seek medical treatment as soon as possible [13]. Factors related to the disease itself are as follows: firstly, our results showed that atypical or vague symptoms of OSA led to longer pre-diagnostic intervals, except for those typical symptoms, such as frequent suffocation in the sleep or falling asleep while waiting for a traffic light. The symptoms are usually little by little aggravated, not as urgent as a heart attack or a brain hemorrhage, which are usually life-threatening. The respondents reported that their symptoms were daytime sleepiness but far from affecting their daily lives [14]. None of the respondents had ever been to the emergency room for their symptoms. Furthermore, it’s well known that OSA and obesity are mutually causal. Most of the obese patients thought their symptoms would ease after losing weight. The health system’s organization mainly affect the delay in diagnostic interval and pre-treatment interval of patients with OSA. The study indicated that health resources were unequal: some patients complained that local hospitals had a lower medical level and were far away from superior hospitals, for that reason, there were few integrated prevention and control networks of hospitals at all levels. Some factors resulting in patients not receiving timely diagnosis and treatment have been shown, such as imperfect sleep monitoring equipment, a lack of multidisciplinary sleep diagnosis centers, fewer sleep monitoring beds per capita, and complex medical procedures in hospitals with inconvenient emergency room green paths, a longer waiting time for examination, and insufficient understanding of the OSA for some medical staff [15,16,17,18]. The medical treatment behavior of OSA patients would have been affected by country medical insurance policies, reimbursement modes and proportions of provinces and cities, and coverage of private medical insurance [18,19,20,21,22,23]. For example, the government fully bears the treatment cost of OSA in France, while it only partially reimburses the surgical treatment cost of OSA in China. Its first-line treatment, CPAP, is still self-funded in China. Now, Polysomnographic monitoring is not included in routine hospital physical examinations or in special populations, for example, drivers and obese people. Thus, it is recommended that PSG should been included in routine physical examination for patients with obesity or other special conditions, even if they have no symptoms.
Avenues for improving early OSA diagnosis
National health authorities should make corresponding publicity for patients, so that the general public gradually understand the OSA and its harm, and the corresponding treatment. Medical-seeking behavior is primarily the result of personal knowledge, attitude/belief and practice [24, 25]. Compared with chronic diseases such as hypertension and diabetes, OSA has a lower awareness rate [26]. The results indicated that eight participants (respondents 3, 6, 9, 10, 11, 12, 13, 15) were unaware of OSA, six participants (respondents 4, 7, 8, 1, 2, 14) had heard of OSA as a disorder but did not take it seriously, and only one participant (respondents 5) had known about it. One in 15 participants opted for CPAP within one year, which is far lower than the 50 percent reported [27]. The damages and complications of OSA to target organs cannot be recognized properly and in time [28], and then timely treatment is not possible after diagnosis. Patients may choose treatment only when accompanied by severe symptoms, resulting in a lower treatment level. At the same time, the medical staff’s cognition of OSA should also be improved to ensure the alertness of OSA [29, 30]. Our analysis indicated that it is possible to prompt early medical treatment and standardize treatment management for patients with OSA, provided that awareness of OSA is increased.
Diseases have their own natural evolutionary progression, which no intervention can change. In this case, we can’t change the path of it, but can only detect it early. Currently, Polysomnography is not included in routine medical examinations in China. Thus, we recommend that different strategies are needed for the different types of people in routine medical check-ups. For special high-risk occupational groups, like a driver, OSA screening for every commercial driver is advocated, given under-resources medical system. In addition, Polysomnography test should be prescribed by clinicians in routine medical check-ups for those special populations who have a short neck with small jaws, rhinitis, excess fat with a neck circumference of more than 40 cm [31].
In addition, the state and the government should vigorously adjust medical resources and strengthen the attention to primary hospitals by improving the relevant diagnostic equipment to improve the situation. It is necessary to establish a diagnosis and treatment system suitable for grassroots work and train medical teams that can stick to working at the grassroots level for a long time and are familiar with the diagnosis and treatment technology of OSA. It is more important to establish a comprehensive prevention and control network based on grassroots medical institutions and coordinated by hospitals at all levels. And further national health authorities need to increase the reimbursement rate for the treatment of OSA, both surgical and CPAP for further improving situation of OSA patients’ medical treatment. Let it be sooner rather than later.
Conclusions
This study illuminated the influencing factors of the elapsed time between first symptom and diagnosis to be longer for some patients than others. These influencing factors can be broadly divided into three categories, namely, disease characteristic, patients, and health service system organization. The OSA does not cause serious complications in a short time, and only affects life when it progresses to a serious degree and the special characteristics of it have led to a general lack of attention to OSA. Besides, patients have serious cognitive deficits and deep-rooted beliefs about OSA in Chinese culture. And one more important thing, there are significant inequalities in access to health resources and services. We hope that the results can provide a reference for national and local medical policies and solutions.
Data availability
The datasets analyzed during the current study are not publicly available due to the fact that it might create a breach in participant confidentiality but are available from the corresponding author on reasonable request.
Abbreviations
- OSA:
-
Obstructive sleep apnea
- AHI:
-
Apnea hypopnea index
- HCP:
-
Healthcare professional
- LSpO2 :
-
Lowest saturation of peripheral oxygen
- PSG:
-
Polysomnography
- ENT:
-
Ear, nose, and throat
- CPAP:
-
Continuous positive airway pressure
- MRI:
-
Nuclear magnetic resonance imaging
References
Patel SR (2019) Obstructive sleep apnea. Ann Intern Med 171(11):Itc81-itc96. https://doi.org/10.7326/aitc201912030
Gottlieb DJ, Punjabi NM (2020) Diagnosis and management of obstructive sleep apnea: a review. JAMA 323(14):1389–1400. https://doi.org/10.1001/jama.2020.3514
Finkel KJ, Searleman AC, Tymkew H, Tanaka CY, Saager L, Safer-Zadeh E et al (2009) Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med 10(7):753–758. https://doi.org/10.1016/j.sleep.2008.08.007
Black JK, Whittaker AC, Balanos GM (2019) Undiagnosed obstructive sleep apnea and physical activity in older manual workers. J Aging Phys Act 27(3):293–299. https://doi.org/10.1123/japa.2018-0096
Henry D, Rosenthal L (2013) “Listening for his breath:” the significance of gender and partner reporting on the diagnosis, management, and treatment of obstructive sleep apnea. Soc Sci Med 79:48–56. https://doi.org/10.1016/j.socscimed.2012.05.021
Vianello A, Bisogni V, Rinaldo C, Gallan F, Maiolino G, Braccioni F et al (2016) Recent advances in the diagnosis and management of obstructive sleep apnea. Minerva Med 107(6):437–451
Walter F, Webster A, Scott S, Emery J (2012) The Andersen Model of Total Patient Delay: a systematic review of its application in cancer diagnosis. J Health Serv Res Policy 17(2):110–118. https://doi.org/10.1258/jhsrp.2011.010113
Scott SE, Walter FM, Webster A, Sutton S, Emery J (2013) The model of pathways to treatment: conceptualization and integration with existing theory. Br J Health Psychol 18(1):45–65. https://doi.org/10.1111/j.2044-8287.2012.02077.x
Njuki R, Kimani J, Obare F, Warren C (2014) Using verbal and social autopsies to explore health-seeking behaviour among HIV-positive women in Kenya: a retrospective study. BMC Womens Health 14:77. https://doi.org/10.1186/1472-6874-14-77
Pedersen AF, Olesen F, Hansen RP, Zachariae R, Vedsted P (2011) Social support, gender and patient delay. Br J Cancer 104(8):1249–1255. https://doi.org/10.1038/bjc.2011.87
Zhang H, Wang G, Zhang J, Lu Y, Jiang X (2019) Patient delay and associated factors among Chinese women with breast cancer: a cross-sectional study. Medicine (Baltimore) 98(40):e17454. https://doi.org/10.1097/md.0000000000017454
Zarhin D (2018) Delaying and seeking care for obstructive sleep apnea: the role of gender, family, and morality. Health (London) 22(1):36–53. https://doi.org/10.1177/1363459316677625
Zarhin D (2016) Sleep as a gendered family affair: snoring and the “dark side” of relationships. Qual Health Res 26(14):1888–1901. https://doi.org/10.1177/1049732315583270
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K et al (2017) Clinical Practice Guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506
Allen AJ, Amram O, Tavakoli H, Almeida FR, Hamoda M, Ayas NT (2016) Relationship between travel time from home to a regional sleep apnea clinic in British Columbia, Canada, and the severity of obstructive sleep. Ann Am Thorac Soc 13(5):719–723. https://doi.org/10.1513/AnnalsATS.201509-613BC
Evans J, Skomro R, Driver H, Graham B, Mayers I, McRae L et al (2014) Sleep laboratory test referrals in Canada: sleep apnea rapid response survey. Can Respir J21(1):e4-10. https://doi.org/10.1155/2014/592947
Chai-Coetzer CL, Antic NA, McEvoy RD (2015) Identifying and managing sleep disorders in primary care. Lancet Respir Med 3(5):337–339. https://doi.org/10.1016/s2213-2600(15)00141-1
Pendharkar SR, Povitz M, Bansback N, George CFP, Morrison D, Ayas NT (2017) Testing and treatment for obstructive sleep apnea in Canada: funding models must change. CMAJ 189(49):E1524-e1528. https://doi.org/10.1503/cmaj.170393
Richards W, Ferdman RM (2000) Prolonged morbidity due to delays in the diagnosis and treatment of obstructive sleep apnea in children. Clin Pediatr (Phila) 39(2):103–108. https://doi.org/10.1177/000992280003900205
Patel J, Topf MC, Huntley C, Boon M (2019) Does insurance status impact delivery of care with upper airway stimulation for OSA? Ann Otol Rhinol Laryngol:3489419878454. https://doi.org/10.1177/0003489419878454
Thomson MD, Siminoff LA (2015) Finding medical care for colorectal cancer symptoms: experiences among those facing financial barriers. Health Educ Behav 42(1):46–54. https://doi.org/10.1177/1090198114557123
Smolderen KG, Spertus JA, Nallamothu BK, Krumholz HM, Tang F, Ross JS et al (2010) Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA 303(14):1392–1400. https://doi.org/10.1001/jama.2010.409
Marchildon GP, Katapally TR, Beck CA, Abonyi S, Episkenew J, Pahwa P et al (2015) Exploring policy driven systemic inequities leading to differential access to care among Indigenous populations with obstructive sleep apnea in Canada. Int J Equity Health 14:148. https://doi.org/10.1186/s12939-015-0279-3
Schlyter M, Andre-Petersson L, Engstrom G, Tyden P, Ostman M (2011) The impact of personality factors on delay in seeking treatment of acute myocardial infarction. BMC Cardiovasc Disord 11:21. https://doi.org/10.1186/1471-2261-11-21
Thompson AE, Anisimowicz Y, Miedema B, Hogg W, Wodchis WP, Aubrey-Bassler K (2016) The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract 17:38. https://doi.org/10.1186/s12875-016-0440-0
Xue B, Jingying G, Ying N, Yifei W, Jiao L, Lu W et al (2023) Status of snoring among elderly patients with chronic diseases and their awareness of obstructive sleep apnea syndrome in a community of Beijing. Chin J Clin Healthc 26(6):778–781. https://doi.org/10.3969/J.issn.1672-6790.2023.06.014
MacKay SG, Lewis R, McEvoy D, Joosten S, Holt NR (2020) Surgical management of obstructive sleep apnoea: a position statement of the Australasian Sleep Association. Respirology 25(12):1292–1308. https://doi.org/10.1111/resp.13967
Forrest LF, Sowden S, Rubin G, White M, Adams J (2017) Socio-economic inequalities in stage at diagnosis, and in time intervals on the lung cancer pathway from first symptom to treatment: systematic review and meta-analysis. Thorax 72(5):430–436. https://doi.org/10.1136/thoraxjnl-2016-209013
Waldman LT, Parthasarathy S, Villa KF, Bron M, Bujanover S, Brod M (2020) Understanding the burden of illness of excessive daytime sleepiness associated with obstructive sleep apnea: a qualitative study. Health Qual Life Outcomes 18(1):128. https://doi.org/10.1186/s12955-020-01382-4
Jennum P, Ibsen R, Kjellberg J (2014) Social consequences of sleep disordered breathing on patients and their partners: a controlled national study. Eur Respir J43(1):134–144. https://doi.org/10.1183/09031936.00169212
Ong TH, Raudha S, Fook-Chong S, Lew N, Hsu AA (2010) Simplifying STOP-BANG: use of a simple questionnaire to screen for OSA in an Asian population. Sleep Breath 14(4):371–376. https://doi.org/10.1007/s11325-010-0350-7
Funding
The authors are grateful to the Fonds Hefei Institute of Physical Sciences, Chinese Academy of Sciences (grant number 202004h07020017) for its financial support to this research project.
Author information
Authors and Affiliations
Contributions
Hongyan Shang carried out the study and drafted the manuscript. Dandan Chen and Qingmei Deng participated in the design of the study and performed the statistical analysis. Zuchang Ma conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors reviewed the results and approved the final version of manuscript.
Corresponding author
Ethics declarations
Ethics approval
The research was conducted in accordance with the Declaration of Helsinki and approved by Medical Research Ethics Committee of the First Affiliated Hospital of China Medical University (2019–306-2).
Consent to participate
All participants signed the approved consent form before the interview, in which they accepted to participate in the study.
Consent for publication
All authors approve the publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shang, H., Chen, D., Deng, Q. et al. Influencing factors of delay in seeking medical attention of patients with obstructive sleep apnea based on the Model of Pathways to Treatment in China: a qualitative analysis. Sleep Breath (2024). https://doi.org/10.1007/s11325-024-03078-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-024-03078-1